Abstract
The soft tissue profile is crucial to esthetics after orthognathic surgery. The aim of this study was to assess the soft tissue changes of the subnasal and submental regions more than 1 year after a sagittal split ramus osteotomy (SSRO) in patients with skeletal class III malocclusion. A total of 22 patients with mandibular prognathism were included in this study. Patients had lateral cephalograms before and more than 1 year after they underwent an isolated SSRO. Soft and hard tissue changes were assessed using the lateral cephalograms. The lower lip, labiomenton, and soft tissue menton moved posteriorly by 85, 89, and 88% compared with the corresponding hard tissue, and the movement of the soft tissue B point and the top of the chin nearly reflected the displacement of the hard tissues, at 96 and 99%, respectively. The labiomenton, stomions, and naso-labial angles were changed after the mandibular set-back and the changes in these angles correlated with either the width of the soft tissue or skeletal displacement. The naso-labial angle could be altered even if an isolated mandibular osteotomy is performed. Changes to the stomions and naso-labial angles were affected by hard tissue movement, while changes to the labiomental angle were affected by the width of the soft tissue after the mandibular osteotomy. It is important to create an accurate preoperative prediction of the esthetic outcomes after a mandibular osteotomy by considering the interrelations between the hard and soft tissues.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A good smile is composed of three crucial factors: the teeth, gingiva, and lips [1]. It is, therefore, necessary to consider esthetics when orthognathic surgery is performed on a patient with a jaw deformity. This is because of changes to the shape of the middle and lower face after surgery. Ghassemi et al. [2] suggested that an ideal outcome of jaw deformity correction must include optimal esthetics, function, and long-term stability. Phillips et al. [3] also noted the importance of esthetics in patients with jaw deformity, stating that improved esthetics and function are significant motivators for the patient to pursue treatment. Proffit and White [4] reported that a combination of orthodontic and orthognathic surgical treatment should be considered for patients who would not have had a satisfactory esthetic outcome with orthodontic treatment alone. The primary goal of orthognathic treatment is to establish a favorable soft tissue contour [5, 6]. Prior reports suggest that predicting postsurgical changes to soft tissue is as important as considering hard tissue changes when surgically correcting a jaw deformity.
Although there have been many prior studies that assessed skeletal stability after orthognathic surgery [7], there is insufficient information assessing soft tissue changes after surgery. Most previous reports that assessed soft tissue changes focused on patients who underwent maxillo-mandibular surgery [8–11]. There are few reports that discuss soft tissue changes after a mandibular osteotomy alone [12–17]. Of these rare reports, two assessed soft tissue changes approximately 6 months after surgery [15, 17]. However, it is recommended that soft tissue changes only be assessed a minimum of 1 year after surgery, as the soft tissue may only stabilize following the completion of bone remodeling at that time point. Furthermore, most previous reports assessed the soft tissue from the upper lip to the submental region. Very few reports assessed soft tissue changes in the subnasal region after surgery.
We hypothesized that the subnasal region would be altered by a mandibular set-back due to the increased traction of the surrounding tissue. The aim of this study was to assess the changes in the soft tissue of the subnasal to submental regions more than 1 year after a sagittal split ramus osteotomy (SSRO) in patients with skeletal class III malocclusion.
Materials and methods
This study was ethically approved by clinical research ethics committee of the institution.
Patients
This study included 22 patients (6 males and 16 females) who underwent a short lingual osteotomy (SLO) [18, 19], a modified SSRO technique, for mandibular prognathism. In SLO, the osteotomy of the lingual side of the ramus is further cut anteriorly, resulting in the minimum bone interference [20]. The mean patient age was 22.45 years (range 17–37 years). No patients had undergone any previous orthodontic or orthognathic treatments. Their jaw set-back was more than 3 mm (mean: 6.72 mm, 3–10.5 mm). The bilateral difference in jaw set-back was less than 5 mm. After surgery, patients were managed using our standard postoperative regimen, which is based on the “physiological positioning strategy” [21, 22]. Briefly, the bony segments were not fixed each other after osteotomy and maxillo-mandibular fixation was performed with wires. The wires were replaced to elastics and jaw exercise was initiated with wearing occlusal splint and elastics at the second postoperative day.
Cephalometric analysis
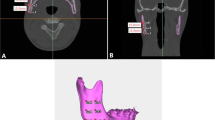
Cephalometric analysis was performed prior to surgery (T1) and more than 1 year postoperatively (T2) using lateral cephalograms. A horizontal reference line was set at a seven degree clockwise rotation from the sella-nasion (SN) line, which was defined as the x-axis based on previous studies [23]. The perpendicular line from the x-axis through the sella (S) was used as the y-axis (Fig. 1). The B point (B), the most anterior points on the upper and lower central incisors (U1C and L1C), and the menton (Me) were used as hard tissue landmarks. The points where lines parallel to the x-axis from B and Me cross the soft tissue plane were assigned the labels Bs and Mes. The subnasal point (SNs), the most anterior point on the chin (TCs), the most anterior points on the upper and lower lips (TULs and TLLs), and the innermost point between the lower lip and the chin (Labiomenton; Labs) were used as soft tissue landmarks. The sella-nasion-B point (SNB) was also measured to assess for mandibular change. To assess the soft tissue angles, the naso-labial angle (NLA), the angle between the upper and lower lips (Stomions angle; Sto), and the angle between lines tangential to the lower lip and chin from Labs (Labiomental angle; Lab) were also measured.
Statistical analysis
The x-axis value of each landmark, angle measurement, and soft tissue width was analyzed using Pearson’s correlation coefficient. A p value < 0.05 was considered significant.
Results
The discrepancy between the hard and soft tissue changes after an SLO (Fig. 2)
While the TLL shifted posteriorly by 6.24 mm 1 year after surgery, the TLLs moved posteriorly by 5.30 mm. The ratio of the TLLs displacement to the TLL was 85%. Similarly, the ratios of the Labs and Mes displacement compared with the Lab and Me were 89 and 88%, respectively. In contrast, the movement of the Bs and TCs almost reflected the movement of the hard tissues, with a B: Bs of 96% and a TC: TCs of 99%.
Change of the labiomental angle (Fig. 3)
Changes in the labiomental angle 1 year after surgery were characterized by the width of Labs–Lab (r = 0.62131), TCs–TC (r = 0.56653), and Mes–Me (r = 0.81534). Each was positively correlated. The labiomental angle after surgery tended to be narrower when the soft tissue of the mandible was thinner. This was especially the case with Mes–Me, which had a strong positive correlation.
Change in the stomions angle Fig. 4
Unlike the labiomental angle, changes to the stomions angle were independent of the soft tissue width of the mandible. In contrast, the stomions angle showed a negative correlation with the amount of TC (r = −0.5124), B (r = −0.4424), Me (r = −0.5266), and L1C (r = −0.4867) movement 1 year after surgery. The stomions angle after surgery tended to be wider when the amount of mandibular set-back was greater.
Changes in the naso-labial angle Fig. 5
The naso-labial angle was changed 1 year after surgery, but it was not correlated with the soft tissue width of the mandible in a similar manner to the stomions angle. Change in the naso-labial angle was negatively correlated with the movement of the hard tissue of the mandible. This meant that the naso-labial angle tended to be wider when the amount of mandibular set-back was greater.
Discussion
Although it has been well known that the naso-labial angle will be altered after a maxilla-mandibular osteotomy, we found that the naso-labial angle would change even in the cases of an isolated mandibular osteotomy. The stomions angle and naso-labial angle were affected by the degree of hard tissue movement, while the labiomental angle was affected by the width of the soft tissue around the mental region postoperatively. The set-back amount may have an effect on the soft tissue response. These hard and soft tissue changes must be considered when making a preoperative prediction of fascial esthetics, and to truly obtain informed consent from the patient.
Jung et al. [16] and Verdenik and Ihan [17] evaluated the naso-labial angle and labiomental angle 6 months after a mandibular osteotomy. Both groups found that these angles were increased in patients with a greater mandibular set-back. Moreover, Legan et al. [24] reported that the naso-labial angle was smaller in patients with a skeletal class III malocclusion. According to these findings, the movement of the mandibular bone could affect the soft tissue around the subnasal region. The naso-labial angle may widen due to soft tissue traction around the mouth after a mandibular set-back.
With respect to the mental region, the hard tissue movement observed here reflected changes to Labs and Bs more than TLLs and Mes. Consequently, the labiomental angle tended to be smaller after a mandibular set-back. Furthermore, the labiomental angle was affected by the width of the soft tissue of the mental region, with an increased angle in cases of thicker soft tissue. It appears that the changes in the metal region after a mandibular osteotomy are important to predict the patient’s facial appearance after orthognathic surgery and to determine the need for a genioplasty.
Although computed tomography (CT) imaging is useful to assess the hard tissue of the jaw, it is difficult to perform frequent imaging due to increased radiation exposure and cost. Furthermore, the patient’s soft tissue contour could be different when in the supine or standing positions. Patients usually assess their facial appearance while standing. Therefore, a CT in the supine position may not be an appropriate method to assess the facial appearance of a patient with a jaw deformity. Laser scans [16] and cone beam CTs [17] can assess the patient’s soft tissue, while he/she is in a standing position. However, these devices are not yet popular. In contrast, a cephalogram can be taken at almost any institution, where orthognathic surgery is performed. X-ray exposure is minimal, and the procedure is standardized. It is important for the patient to relax without excessive muscle strain when the cephalogram is taken. Since the soft tissue contour is easily changed by muscle strain, the shorter exposure time of a cephalogram is better than the longer exposure time of CT scans.
PPS showed good skeletal stability with little TMD [21, 22]. The good skeletal stability may make it easy to expect the soft tissue changes after surgery. In addition, TMD influences the jaw moving and this may contribute the soft tissue changing after surgery. Therefore, PPS was adapted to all patients in this study. It is important to consider the potential for postoperative changes to the naso-labial angle as part of the preoperative workup of patients who must undergo an isolated mandibular osteotomy. Postoperative facial appearance could be correctly predicted if the soft tissue width and hard tissue movement are considered. These measurements can be useful tools for preoperative planning and in discussions with the patient before surgery.
References
Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontology. 2000;1996(11):18–28.
Ghassemi M, Hilgers RD, Jamilian A, Hölzle F, Fritz U, Gerressen M, Ghassemi A. Consideration of effect of the amount of mandibular setback on the submental resion in the planning of orthodontic-orthognathic treatment. Br J Oral Maxillofac Surg. 2014;52:334–9.
Phillips C, Broder HL, Bennett ME. Dentofacial disharmony: motivations for seeking treatment. Int J Adult Orthodon Orthognath Surg. 1997;12:7–15.
Proffit WR, White RP Jr. Who needs surgicalorthodontic treatment? Int J Adult Orthod Orthog Surg. 1990;5:81.
Worms FW, Isaacson RJ, Spiedel TM. Surgical orthodontic treatment planning: profile analysis and mandibular surgery. Angle Orthod. 1976;46:1–25.
McCollum AG, Evans WG. Facial soft tissue: the alpha and omega of treatment planning in orthognathic surgey. Semin Ortho. 2009;15:196–216.
Becker OE, Avelar RL, do Dolzan NA, Haas OL Jr, Scholari N, de Oliveira RB. Soft and hard tissue changed in skeletal class III patients treated with double-jaw orthognathic surgery- maxillary advancement and mandibular setback. Int J Oral Maxillofac Surg. 2014;43:204–12.
Soncul M, Bamber MA. Evaluation of facial soft tissue changes with optical surface scan after surgical correction of class III deformities. J Oral Maxillofac Surg. 2004;62:1331–40.
Aydemir H, Efendiyeva R, Karasu H, Toygar-Memikoğlu U. Evaluation of long-term soft tissue changes after biomaxillary orthognathic surgery in class III patients. Angle Orthod. 2015;85:631–7.
Chew MT. Soft and hard tissue changes after bimaxillary surgery in Chinese class III patients. Angle Orthod. 2005;75:959–63.
Altug-Atac AT, Bolatoglu H, Memikoglu UT. Facial soft tissue profile following bimaxillary orthognathic surgery. Angle Orthod. 2008;78:50–7.
Robinson SW, Speidel TM, Isaagson RJ, et al. Soft tissue profile change produced by reduction of mandibular prognathism. Angle Orthod. 1972;42:227–35.
Hershey HG, Smith LH. Soft-tissue profile change associated with surgical correction of the prognathic mandible. Am J Orthod. 1974;65:483–502.
Suckiel JM, Kohn MW. Soft-tissue changes related to the surgical management of mandibular prognathism. Am J Orthod. 1978;73:676–80.
Lee ST, Minami K, An CH, Park JW, Kwon TG. Does skeletal surgery for asymmetric mandibular prognathism influence the soft tissue contour and thickness? J Oral Maxillofac Surg. 2013;71:1577–87.
Jung YJ, Kim MJ, Baek SH. Hard and soft tissue changes after correction of mandibular prognarhism and facial asymmetry by mandibular setback surgery: three-dimensional analysis using computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:76–771.
Verdenik M, Ihan Hren N. Differences in three-dimensional soft tissue changes after upper, lower or both jaw orthognathic surgery in skeletal class III patients. Int J Oral Maxillofac Surg. 2014;43:1345–51.
Hunsuck EE. A modified intraoral sagittal splitting technique for correction of mandibular prognathism. J Oral Surg. 1968;26:250–3.
Epker BN. Modification in the sagittal osteotomy of the mandible. J Oral Surg. 1977;35:157–9.
Yang HJ, Lee WJ, Yi WJ, Hwang SJ. Interferences between mandibular proximal and distal segments in orthognathic surgery for patients with asymmetric mandibular prognathism depending on different osteotomy techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:18–24.
Ohba S, Yoshida M, Kohara H, Kawasaki T, Minamizato T, Koga T, Nakatanin Y, Watanabe E, Nakao N, Yoshida N, Asahina I. Short lingual osteotomy without fixation; a new strategy for mandibular osteotomy known as “physiological positioning”. Br J Oral Maxillolfac Surg. 2014;52:e9–13.
Ohba S, Nakao N, Nakatani Y, Kawasaki T, Minamizato T, Koga T, Kohara H, Yoshida N, Asahina I. The skeletal stability after maxilla-mandibular osteotomy with a “physiological positioning strategy”. Br J Oral Maxillofac Surg. 2014;52:965–9.
Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for orthognathic surgery. J Oral Surg. 1978;36:269–75.
Legan HL, et al. Soft tissue cephalometric analysis for orthognathic surgery. J Oral Surg. 1980;38:744–51.
Acknowledgements
We thank to all staffs at the Departments of Regenerative Oral Surgery and Orthodontics and Dentofacial Orthopedics for their clinical helps.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ohba, S., Kohara, H., Koga, T. et al. Soft tissue changes after a mandibular osteotomy for symmetric skeletal class III malocclusion. Odontology 105, 375–381 (2017). https://doi.org/10.1007/s10266-016-0280-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10266-016-0280-3