Abstract
Background
Postoperative eyelid asymmetry is the most common complaint of patients after undergoing blepharoplasty and ptosis correction surgery. Calibrating eyelid asymmetry during ptosis correction surgery is still difficult for surgeons despite the development of innovative procedures. Our levator pull-out suture technique for correcting postoperative eyelid asymmetry after ptosis surgery is introduced.
Methods
A total of 330 patients who underwent ptosis correction surgery with upper blepharoplasty from 2016 to 2017 were enrolled in our study. All surgeries were performed using the levator pull-out suture technique, and the postoperative eyelid asymmetry was corrected in the outpatient clinic at 2–3 days after the operation. Patient satisfaction was evaluated preoperatively and at 1 week and 2 months postoperatively using a questionnaire. Visual acuity, marginal reflex distance 1 (MRD1), and vertical palpebral fissure length asymmetry were measured preoperatively and compared to values taken postoperatively.
Results
Patient satisfaction regarding asymmetry increased from 2.7/5 (preoperatively) to 4.1/5 points (postoperatively). MRD1 and vertical palpebral fissure length increased from 1.1/1.2 and 6.8/6.8 mm (preoperatively), respectively, to 2.8/2.9 and 8.5/8.6 mm (postoperatively), respectively. The asymmetry of MRD1 and vertical palpebral fissure length before and after surgery were corrected from 0.45/1.81 to 0.01/0.19 mm (p < 0.01).
Conclusion
Our innovative surgical method of using the levator pull-out suture technique is relatively simple and allows for finer suture adjustments postoperatively to effectively correct eyelid asymmetry, with satisfactory results.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative eye asymmetry is a common complication of upper eyelid surgery, including blepharoplasty or double eyelid surgery, in the Asian population [1,2,3]. Although patients are well informed by surgeons of the possible postoperative outcomes, there are numerous complaints about postoperative asymmetry [4]. An individual’s eyes are perfectly symmetrical [5], and even the best outcome from the surgeon’s standpoint can result in disgruntled patients.
However, achieving the perfect eye symmetry is difficult, even with revision eyelid surgery. Although much attention is given in the preoperative design [6] and in developing various innovative procedures [7], postoperative eye asymmetry is still common. Eyelid asymmetry is the main cause of long-term dissatisfaction in these patients (Table 1). In addition, the upper eyelid anatomy of Asians differs from that of Caucasians, and specifically, ptosis correction of Asians is more likely to be asymmetrical compared to that of Caucasians [8].
Calibrating eye symmetry during surgery is difficult because of intraoperative bleeding and tissue edema caused by local injection of a solution preoperatively. In addition, the solution is locally injected into the levator and Muller muscles, which are the muscles involved in eye opening. Thus, perfectly opening the eyes during the surgery to assess eyelid asymmetry can be difficult. Postoperatively, if full voluntary eyelid opening, in which the levator muscles can be controlled, is possible after the effects of the drugs have completely worn off, it is possible to more finely adjust the symmetry of the bilateral eyelid. In addition, as postoperative asymmetry is a relatively subjective complaint, resolving the eyelid asymmetry immediately after the operation will lead to greater patient satisfaction.
This study aimed to introduce a new innovative technique for ptosis correction surgery to effectively and immediately correct postoperative asymmetry.
Methods
Patients
Our study procedures adhered to the principles of the Declaration of Helsinki. Informed written consent was obtained from all participants. Between January 2016 and January 2017, patients who underwent blepharoplasty with ptosis correction were included in this study. All operations were performed by the senior author. Medical photographs were taken of all patients. The levator function, marginal reflex distance 1 (MRD1), and vertical palpebral fissure lengths in both eyes were measured by the surgeon preoperatively and at 2 months postoperatively.
Operative Method
Design
Preoperatively, the degree of ptosis was measured, while the patient was sitting upright in a comfortable position. The patient was instructed to repeatedly open and close his or her eyes. The ptosis grade was noted, and the patient’s natural eyelid crease, desired new crease, and expected degree of levator muscle plication were marked and noted in advance. Finally, the medial and lateral borders of the pupil and iris, as well as the medial and lateral canthi, were marked, and the need for skin excision and amount of resection were assessed based on the patients’ preoperative skin laxity.
Incision and Dissection
A solution of 1:100,000 epinephrine mixed with 2% lidocaine was locally injected into the skin and tarsal plate, and after 3–4 min, an incision along the marked eyelid crease was made. The skin, orbicularis oculi muscle, and septum were incised simultaneously. Dissection was performed under the tarsal plate, and the inner surface of the septum and levator aponeurosis were separated. Dissection was carried out inferiorly to the adhesion of the tarsal plate and levator muscles and superiorly to the superior orbital rim.
Tarsodermal Suture and Levator Plication
To make a double-fold of the eyelid, tarsodermal suturing was performed in the following three locations using a 7–0 nylon suture: midline of the pupil, medial limbus, and lateral limbus. Subsequently, we performed the levator plication suturing. Initially, the suture was placed at the position depending on the degree of plication, and the suture was fixed in the tarsal plate to complete the plication.
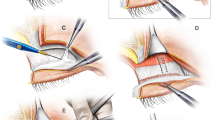
Levator Pull-Out Suturing
Levator pull-out suturing was performed on the eye with the most severe degree of asymmetry, as determined preoperatively. If the ptosis on both sides was similar to the degree of asymmetry not greater than 4 mm, both sides were plicated, and levator pull-out suturing was performed on the more severe eye with ptosis. In contrast, if ptosis on one side is severe, whereas the other side is normal, an appropriate degree of plication on the eye with ptosis was performed and levator pull-out suturing without plication was performed on the contralateral normal eye.
The levator pull-out suture was placed at two points, at both the lateral limbal margins. The plication was performed in the same manner as that previously performed for levator plication sutures because both the levator pull-out suturing and the levator plication suturing began from the levator, passed through the tarsal plate, and then reached the levator. However, in the case of pull-out suturing, the amount of plication was bigger because the pull-out sutures were fixated at the upper part of the levator about 8–12 mm higher than the previous sutures.
The suture was left untied after passing through the levator aponeurosis, and temporary suturing was performed outside of the skin flap. Then, the knot was pulled out of the eye, and the rest of the skin suture was completed (Fig. 1). After completing the operation, the threaded part containing the knot is temporarily fixed using a tape (Video 1).
Postoperative Suture Adjustment and Management
Postoperative edema was minimized by immediately applying ice on the operative site. The levator control suture was adjusted during the first follow-up visit of the patient on the third day postoperatively (Figs. 2b, 3 Middle). When the opening of the eye with the pull-out suture was insufficient, the amount of additional plication of the levator was analyzed, and asymmetry was adjusted by additionally tying the pull-out suture after removing the temporary knot. The surgeon controlled the pull-out suture by tying the first knot, and then the surgeon asked the patients to fully open their eyes. If overcorrection was present, the tie was loosened and was corrected again. After the adjustment was completed, the knot was cut very shortly to fit under the skin flap (Video 2) (Figs. 2c, 3 Bottom). The skin suture was removed on the sixth day postoperatively leaving no visible scar (Fig. 4).
Evaluation of Patient Satisfaction
The patients were asked to complete a questionnaire that evaluated their level of satisfaction preoperatively and at 1 week and 2 months postoperatively. The following items were evaluated using a 5-point grading system [from 1 (very poor) to 5 points (very satisfied)] (Table 1).
Results
A total of 330 (72 men and 258 women) patients who underwent blepharoplasty with ptosis correction from January 2016 to January 2017 were included in this study. Mean postoperative follow-up duration was 2.5 months (range 2 months–2 years), and the mean age was 27 (range 18–49) years. A total of 291 and 39 patients underwent primary and revision blepharoplasty operations, respectively. The patients had an average of 2.4 revision surgeries (range 1–4, the number of previous operations). Sixty-five (20%) and 20 (6%) patients underwent rhinoplasty, and bone contouring surgery, respectively, simultaneously with the ptosis surgery. They had no notable severe complications, such as postoperative infection, retrobulbar hematoma, or blindness.
Subjective Results of Patient Satisfaction Questionnaire
Preoperatively, most patients complained of inadequate eye opening (1.5/5). They were also dissatisfied with their vertical palpebral fissure length (2.5/5). At 1 week postoperatively, the patients complained of discomfort (1.6/5) around the eyes. At 2 months postoperatively, the patients were generally satisfied with eye opening (4.8/5), vertical palpebral fissure length (4.5/5), and asymmetry (4.1/5).
Objective Measurements
The visual acuity of the patients before and after surgery did not change (Table 2). On the other hand, a statistically significant difference was found in the patients’ levator function (preoperative 4.9/5.3, postoperative 10.3/11.8, p < 0.001), MRD1 (preoperative 1.1/1.2, postoperative 2.8/2.9, p < 0.001), and vertical palpebral fissure length (preoperative 6.8/6.8, postoperative 8.5/8/6, p = 0.02) before and after the surgery. In addition, the MRD1 and vertical palpebral fissure length asymmetry before surgery were corrected to a significant degree at 2 months postoperatively (preoperative 0.45/1.81, p = 0.01, postoperative 0.01/0.19, p < 0.001).
Discussion
In this study, we introduced an innovative surgical method for ptosis correction surgery. Our levator pull-out suture technique is relatively simple and allows for a finer adjustment after surgery to effectively correct postoperative eyelid asymmetry, and it obtained satisfactory results.
Is it possible to achieve perfect eyelid symmetry after blepharoplasty? The most common complaint we encountered after eye surgeries in several patients was with regard to eyelid asymmetry (Table 3). Although there is an acceptable degree of asymmetry [9], in our experience, the severity of asymmetry was not necessarily related to the complaint of the patient, and even if the surgeon considered the result of the operation satisfactory, the patient frequently had different opinions. Surprisingly, there were fewer complaints about the extent of ptosis correction after the surgery, as the operation concentrated more on the effective plication of levator muscles.
Numerous oculoplastic surgeons have had similar concerns, and there have been many references to various correction methods of preoperative asymmetry and of adjusting postoperative asymmetry. Park et al. [10] and Collin et al. [3] attempted to correct preoperative asymmetry by overcorrection of the eyes with severe ptosis, compared to the other eye conditions, using various methods, such as levator resection, brow suspension, and frontalis myofascial flap. Moreover, Ben Simon et al. [11] injected hyaluronic acid beneath the upper eyelid of the overcorrected eye to reduce unnecessary eye opening, and Muhlbauer et al. [12] administered Botox injection in the overcorrected eye or performed selective neurotomy in patients with more severe asymmetry. However, none of the above-mentioned methods provided satisfactory results in overcoming postoperative eyelid asymmetry and could not reduce patients’ complaint or dissatisfaction.
In addition, the eyelid anatomy of Asians has several important differences compared to that of Caucasians, which are directly related to the caution in ptosis correction. First, the Asian eyelid has a low lid crease and lash ptosis because it has a richer fullness of the upper eyelid. In addition, because of the low eyelid height and short fissure length, asymmetry is more obvious and less acceptable in Asians than in Caucasians [8]. Finally, because the levator muscle attachment is often not strong, it is more difficult to control the amount of levator advancement procedure [13]. All these difficulties were experienced by authors when performing ptosis correction surgery; hence, we developed the pull-out suture technique to address these problems.
In the preoperative design or surgical planning stage, we considered Hering’s law [10] and performed proper undercorrection. Moreover, even though the designs on both sides are exactly the same, they can still vary [6], and there can be an undesirable difference in both sides of the skin. We also attempted using intraoperative voluntary opening of the eyelid as a reference during the operation. However, swelling due to the solution injected locally and temporary paralysis of the levator and muller muscles due to lidocaine injection made it impossible for us to perform finer adjustments to achieve bilateral symmetry. When there is severe postoperative eyelid asymmetry, patients are advised to undergo reoperation after a certain period of time after the initial surgery [7, 14, 15]. Although reoperation can be performed, it still does not guarantee perfect eyelid symmetry, Moreover, the broken trust between the patient and the surgeon may be difficult to rebuild.
To reduce or completely eliminate patients’ complaints of eye asymmetry after surgery, we performed the levator pull-out suture technique. This method effectively prevented and corrected postoperative eyelid asymmetry, which we thought impossible to resolve. Moreover, this technique was more effective than the conventional levator plication technique. This is because the vertical length difference between both eyes is more effectively corrected.
If the tissue edema has moderately subsided 5–7 days after surgery and the effect of anesthesia has completely worn off, more accurate adjustment can be performed in addition to intraoperative levator control. Furthermore, the surgeon continues to perform surgery with one more effective tool to correct bilateral asymmetry after surgery so that the patients do not have to get up, sit down, or repeatedly open and close their eyes. In addition, because of the anesthetic drug injected during surgery, relying on this method does not help to prevent asymmetry after surgery.
The amount of postoperative correction with the pull-out suture should not be overdone or significant. As the general recovery time to achieve stable results is as long as 2 months [15, 16], if the change is more dramatic, there can be a higher possibility of overcorrection on the pull-out suture side. As the additional amount of plication with the pull-out suture is usually 4–8 mm, the opening of the eyelid is adjusted 1 or 2 mm as a result; thus, the difference does not appear as dramatic as expected. We have encountered overcorrection problems in our early experiences, and we learned not to overdo the postoperative correction with pull-out sutures.
Our technique has a few disadvantages. First, given that additional procedures are performed a few days after the surgery, the exposed operative site can be vulnerable to infection and patients may experience additional discomfort during the procedure. However, blepharoplasty has a lower risk of infection compared to other facial plastic surgeries [17]. In fact, none of our patients had an infection. In addition, if patients are well informed and the sealing of the thread is completed by taping, discomfort can be avoided. Second, the patient may experience some pain when adjusting the pull-out suture a few days after the surgery. However, the pain had a short duration, and despite the pain, the majority of patients were very satisfied with the fact that their eye asymmetry was being corrected.
The limitation of our study is its retrospective nature, owing to which some variables, such as preoperative asymmetry, vertical palpebral fissure length, or racial differences, may not be well controlled. However, the technique has many advantages in correcting ptosis and preventing postoperative asymmetry, and we would like to share the technique; furthermore, future studies should evaluate additional results from various eyelid surgeries such as Asian non-incisional double eyelid surgery and conventional blepharoplasty without ptosis correction.
Conclusion
In this study, we introduced an innovative surgical method for ptosis correction surgery. Our levator pull-out suture technique is relatively simple and allows for a finer adjustment after surgery to effectively correct postoperative eyelid asymmetry.
References
Golan S, Goldberg RA (2017) Time course analysis of upper blepharoplasty complications. Dermatol Surg 43:307–309
Czyz CN, Lam VB, Foster JA (2011) Management of complications of upper eyelid blepharoplasty (Master techniques in blepharoplasty and periorbital rejuvenation). Springer, New York
Collin J (1979) Complications of ptosis surgery and their management: a review. J R Soc Med 72:25–26
Chang S, Lehrman C, Itani K, Rohrich RJ (2012) A systematic review of comparison of upper eyelid involutional ptosis repair techniques: efficacy and complication rates. Plast Reconstr Surg 129:149–157
Pool SM, van der Lei B (2015) Asymmetry in upper blepharoplasty: a retrospective evaluation study of 365 bilateral upper blepharoplasties conducted between January 2004 and December 2013. J Plast Reconstr Aesthet Surg 68:464–468
Yi MY, Choi HS, Jang JW, Kim SJ, Jang SY (2017) Asymmetry of preoperative incision design markings for upper blepharoplasty. J Craniofac Surg 28:e419–e422
Park KS, Park DD (2017) Objective outcome measurement after upper blepharoplasty: an analysis of different operative techniques. Aesthet Plast Surg 41:64–72
Saonanon P (2014) Update on Asian eyelid anatomy and clinical relevance. Curr Opin Ophtalmol 25:436–442
Wang TT, Wessels L, Hussain G, Merten S (2017) Discriminative thresholds in facial asymmetry: a review of the literature. Aesthet Surg J 37:375–385
Park DH, Kim CW, Shim JS (2008) Strategies for simultaneous double eyelid blepharoplasty in Asian patients with congenital blepharoptosis. Aesthet Plast Surg 32:66–71
Ben Simon GJ, Lee S, Schwarcz RM, McCann JD, Goldberg RA (2007) Muller’s muscle-conjunctival resection for correction of upper eyelid ptosis: relationship between phenylephrine testing and the amount of tissue resected with final eyelid position. Arch Facial Plast Surg 9:413–417
Mühlbauer W, Holm C (1998) Eyebrow asymmetry: ways of correction. Aesth Plast Surg 22:366–371
Kakizaki H, Malhotra R, Selva D (2009) Upper eyelid anatomy: an update. Ann Plast Surg 63:336–343
Chen B, Song H, Gao Q, Xu M, Wang J, Wang F, Chen S, Wu J, Li H (2017) Measuring satisfaction with appearance: validation of the FACE-Q scales for double-eyelid blepharoplasty with minor incision in young Asians- retrospective study of 200 cases. J Plast Reconstr Aesthet Surg 70:1129–1135
Lee JH, Nam SM, Kim YB (2015) Blepharoptosis correction: levator aponeurosis-Muller muscle complex advancement with three partial incisions. Plast Reconstr Surg 135:388–395
Oster G, Sullivan SD, Dalal MR, Kazemi MR, Rojeski M, Wysham CH, Sung J, Johnstone B, Cali AM, Wei LJ, Traylor L, Anhalt H, Hull M, Van Vleet J, Meneghini LF (2016) Achieve control: a pragmatic clinical trial of insulin glargine 300 U/mL versus other basal insulins in insulin-naive patients with type 2 diabetes. Postgrad Med 128:731–739
Gravante G, Caruso R, Araco A, Cervelli V (2008) Infections after plastic procedures: incidences, etiologies, risk factors, and antibiotic prophylaxis. Aesth Plast Surg 32:243–251
Acknowledgements
None of the authors have financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Intraoperative video of performing levator correction surgery with the pull-out suture technique. (MP4 17574 kb)
Video presentation of the surgeon adjusting the pull-out suture of the patient (from Video 1 and Fig. 2) at three days after the operation in the outpatient clinic. (MP4 21897 kb)
Rights and permissions
About this article
Cite this article
Hwang, I., Myung, Y. & Park, S. Levator Pull-Out Suture Technique for Immediate Postoperative Correction of Eyelid Asymmetry After Ptosis Surgery in Asians. Aesth Plast Surg 43, 388–394 (2019). https://doi.org/10.1007/s00266-018-1276-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-018-1276-x