Abstract
Background
Upper blepharoplasty is indicated in Asians for double-eyelid fold creation, periorbital rejuvenation, and functional visual field improvement. This article introduces a technical classification for blepharoplasty methods and investigates approaches to evaluate its outcomes.
Methods
Of 535 patients undergoing aesthetic upper blepharoplasty in our institution in 1998–2011, 136 patients who were well followed up were retrospectively reviewed and categorized into four groups according to the techniques employed. Blepharoplasty with skin excision only was indicated for upper eyelid-skin redundancy patients with prominent double eyelids (n = 20). Blepharoplasty with skin excision and nonburied suture fixation was indicated for patients with upper lid-skin redundancy and weak double eyelids (n = 15). Blepharoplasty with skin excision and buried suture fixation was indicated for patients with upper lid-skin redundancy but no double-eyelid folds (n = 46). Finally, blepharoplasty with simultaneous ptosis correction was utilized for patients with senile or subclinical ptosis requesting upper blepharoplasty (n = 55). The mean age was 48.7 years at surgery; the mean follow-up period was 6 months. Digital photographs were used to compare changes in marginal reflex distance 1 (MRD1), percentage of the area of corneal exposure (%ACE), and brow height.
Results
MRD1 increased from 1.92 to 2.84 mm in the whole patient group after upper blepharoplasty; it increased the most in blepharoplasty with simultaneous ptosis correction (1.22 mm). %ACE increased from 62.1 to 76.6% (14.5%), whereas brow height decreased from 29.4 to 26.7 mm (9.2%).
Conclusion
Upper blepharoplasty improves palpebral fissure. Numerically measured palpebral fissure changes facilitate operation outcome measurement.
Level of Evidence III
This journal requires that authors assign a level of evidence to each submission to which Evidence-Based Medicine rankings are applicable. This excludes Review Articles, Book Reviews, and manuscripts that concern Basic Science, Animal Studies, Cadaver Studies, and Experimental Studies. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blepharoplasty is one of the most common procedures in aesthetic surgery. In particular, double-eyelid surgery is the most common aesthetic surgery in Korea [1]. Asian upper blepharoplasty, which is often synonymous with double-eyelid surgery, is performed mainly to create a well-defined supratarsal crease and thus a supratarsal fold. Some young Asians may seek upper blepharoplasty to reduce the puffiness of their upper eyelids, tighten the supratarsal skin, enlarge the vertical palpebral fissures, or achieve some eversion of the eyelashes [2]. In middle-aged and older patients, upper blepharoplasty is an effective way to achieve periorbital rejuvenation, with conservative excision of redundant skin, muscle, and orbital fat to preserve the fullness of lateral upper eyelids that portrays youthfulness [3]. Improving visual field deficits, especially in the upper temporal area, is a functional indication in some patients.
Various blepharoplasty techniques for Asian patients have been described in the literature. These methods have been generally classified into nonincision methods and incision methods. In some studies, partial or mini-incision methods are added as a third category [4, 5]. These methods can be further subclassified into the nonburied suture methods and buried suture methods. The creation of a double eyelid is dependent on skin-to-levator aponeurosis or skin-to-tarsus fixation with subsequent formation of fibrous adhesions in all of these methods.
Nonincision methods are suitable for young patients who do not require skin excision and have no excess fat. Partial incision methods have the advantages of removing excess fat through a small incision while sharing the minimally invasive features of nonincision methods. Although there are trends and demands concerning minimal surgical scars and swifter postoperative recovery, incision methods still play important roles as effective and standard methods. Incision methods are indicated in the presence of redundant skin or even dermatochalasis, fat prolapse, ptosis, asymmetric eyelids, scars in the upper eyelids, and revision or reoperation cases, or for making more prominent and vivid double eyelid through the formation of a tougher cicatricial connection from the skin to the upper tarsus or aponeurosis [4].
Incision methods are divided into simple and complex techniques, as described by Fernandez [6]. The simple technique involves resecting a skin strip and suturing the lower incision margin skin to the deeper tissues without dissecting the aponeurosis, thereby creating a static crease by supratarsal or intratarsal fixation. In the complex technique, the levator aponeurosis is freed from the tarsal plate and Muller’s muscle and sutured to the lower incision margin dermis, resulting in a deeper and dynamic crease. Fernandez’s complex technique was later modified to become the anchor or invagination blepharoplasty technique, which brings the free levator aponeurosis to the supratarsal skin to create a well-defined eyelid crease [7].
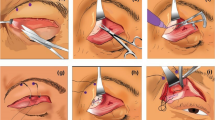
In this study, the authors introduce an operative classification for Asian blepharoplasty incision methods, namely (1) blepharoplasty with skin excision only, (2) blepharoplasty with skin excision and tarsal fixation, (3) blepharoplasty with skin excision and tarsal fixation with buried suture fixation, and (4) blepharoplasty with simultaneous ptosis correction (Fig. 1). In addition, we aim to investigate objective methods for evaluating the functional and aesthetic outcomes with these techniques using the marginal reflex distance 1 (MRD1), brow height (BH) changes, and the percentage of the area of corneal exposure (%ACE).
Technical classification of upper blepharoplasty. a Technique I: blepharoplasty with skin excision only. b Technique II: blepharoplasty with skin excision and nonburied suture fixation. c Technique III: blepharoplasty with skin excision and buried suture fixation. d Technique IV(a): blepharoplasty with simultaneous ptosis correction. Levator aponeurosis plication. e Technique IV(b): levator advancement or Muller muscle and aponeurosis composite flap advancement
Patients and Methods
Study Patients
In 1998–2015, a total of 535 patients undergoing aesthetic upper blepharoplasty with incision methods for the purpose of double-eyelid formation and rejuvenation at our medical institution were identified by the senior author. Their clinical data were retrospectively reviewed and included for analysis. The mean age was 48.7 years at the time of surgery, and the mean follow-up period was 6 months postoperatively. A total of 136 patients who were well followed up were selected for photographic analysis. They were categorized into four groups according to the techniques used for upper blepharoplasty.
Surgical Techniques
Operative Techniques
Technique I: Blepharoplasty with Skin Excision Only
For this technique, surgery was performed under local anesthesia using 1% lidocaine with 1:100,000 adrenaline. The skin incision was then made, and the premarked strip of excess skin was excised with a size 15 blade. The orbicularis oculi muscle (OOM) was preserved unless there was hypertrophy of the muscle and puffiness of the upper eyelids. Pinpoint insulated cautery (Colorado Micro Dissection Needle, Stryker Leibinger, Inc., Kalamazoo, MI) was used to diathermize along the lower incision margin. Three key sutures are placed at the vertical markings with three interrupted nylon 7/0 sutures. The skin wound was closed in a single layer with several simple interrupted tag sutures and then continuous running nylon 7/0 suture (Fig. 1a).
Technique II: Blepharoplasty with Skin Excision and Nonburied Suture
In technique II, the supratarsal crease and skin incision marking, local anesthesia injection, and skin incision or excision steps were performed as in technique I. After the pre-aponeurotic fat was teased out from the septum window, a tenotomy scissor was inserted and the septum was fully opened. Only a thin strip of OOM and supratarsal fat overlying the superior tarsal margin was excised using the tip of the tenotomy scissors to expose the superior tarsal margin and distal part of the levator aponeurosis. Fixation was accomplished using nonburied 6/0 nylon sutures. Four-point fixations were usually performed at the axis of the midpupillary, medial limbus, lateral limbus, and between the lateral limbus and lateral canthus. The superior tarsal margin was marked after identification and grasping with fine-tooth forceps. For the skin-to-tarsal fixation, the first fixation suture was placed vertically through the superior incision margin, horizontally through the tarsus at the level of 2 mm inferior to the superior tarsal margin, and then vertically through the superior incision margin; it was then firmly tied down with 4–5 square knots (Fig. 1b). Alternatively, skin-to-levator aponeurosis fixation could be performed.
Technique III: Blepharoplasty with Skin Excision and Buried Suture Fixation
The supratarsal crease and skin incision marking, local anesthesia injection, skin excision, opening of orbital septum, preserving of pre-aponeurotic fat, and exposure of the superior tarsal were performed similarly to technique II, as described above. The inferior skin incision margin could be fixed to the superior tarsus or levator aponeurosis using buried 5/0 or 6/0 PDS sutures. Four-point fixations were usually performed, as described above. For the skin-to-tarsal fixation, the suture was passed through the dermomuscular edge of the inferior incision skin margin and horizontally through the tarsus about 2 mm from the superior tarsal margin; it was then tied down with 4–5 firm square knots (Fig. 1c).
Technique IV: Blepharoplasty with Simultaneous Ptosis Correction
-
(a)
Levator aponeurosis plication.
In ptosis with good (8–12 mm) or fair (5–7 mm) levator function, a levator plication was performed. The position of the lid margin was adjusted to 1–2 mm below the upper limbus in bilateral cases. In unilateral cases, the position of the lid margin was adjusted to the level of the superior limbus according to that on the nonptotic side. After exposing the superior tarsal margin and levator aponeurosis, marking of the superior tarsal margin was identified. The predetermined level of levator plication was marked on the aponeurosis with a temporary suture. The two plication sutures were placed at the medial and lateral limbus axis using double-needle PDS 5/0 suture. One of the needles was passed horizontally through the tarsus 2 mm from the superior tarsal margin and then vertically through the superior tarsus to the marked level of the aponeurosis. The other needle was also passed vertically through the superior tarsus to the marked level of the aponeurosis and temporarily tied to the first suture end. Further reinforcement plication between the levator aponeurosis and superior tarsus was performed using Vicryl 6/0 sutures (Fig. 1d). Skin-to-skin approximation for skin closure was performed with continuous running 7/0 nylon.
-
(b)
Levator advancement or Muller muscle and aponeurosis composite flap advancement.
Through the double-eyelid incision, a portion of the OOM and supratarsal fat overlying the superior tarsus was removed to expose the upper tarsus and levator aponeurosis. With the upper eyelid inverted, the conjunctiva was separated from the Muller muscle laterally to medially using iris scissors. A mosquito instrument was passed horizontally between the conjunctiva and the Muller muscle. When the upper eyelid was replaced to the normal position, the Muller muscle and levator aponeurosis were cut horizontally. The detached Muller muscle–levator aponeurosis composite flap was marked at the predetermined level. This is advanced on the anterior surface of the tarsus using 5-0 PDS suture (Fig. 1e). When the eyelid level was confirmed to be satisfactory on primary gaze, further reinforcement sutures between the original sutures were performed using Vicryl 6/0. Skin-to-skin approximation for skin closure was carried out with continuous running 7/0 nylon.
Anthropometry and Photographic Analysis
Preoperative frontal view digital photographs were obtained in all patients using a Nikon D80 digital camera (Nikon Corporation, Tokyo, Japan) with a standardized lens. To acquire the photographs, patients sat approximately 1.0 m away from the camera with eyes in primary gaze, and the same horizontal axis was used. Postoperative photographs were taken at 1 month after surgery. The preoperative and postoperative images were analyzed using the qualitatively analyzed software Adobe Photoshop 7.0.1 (Adobe Inc., San Jose, CA) and Java-based image processing software (ImageJ 1.40; National Institutes of Health, Bethesda, MD).
Measurement of MRD1 (Marginal Reflex Distance)
Two horizontal lines were drawn through the center of the pupil and the superior eyelid margin on the image in Adobe Photoshop. The perpendicular distance between these lines was taken as MRD1. Three measurements were taken for each patient by the same observer, and the average was taken as the final measured MRD1 (Fig. 2). Due to ratio difference between digital photographs, a correction value with corneal diameter was utilized in proportional expression for numerical transformation of the measured data. As the corneal diameter is quite consistent in the same adult population, we applied 11.45 ± 0.9 mm as the average real cornea diameter of Koreans [8] to calculate the real MRD1 in Microsoft Excel 2011 with the formula.
Percentage of Corneal Exposure Area (%CEA)
With the digital photographs opened in Adobe Photoshop, the visualized corneal area was outlined on one eye and total corneal area was outlined on the same eye (Fig. 3). The corneal areas were measured. The same technique was repeated for the opposite eye to obtain an average. The corneal exposure area was quantified with ImageJ to calculate the percentage with the formula.
Brow Height (BH)
A horizontal line passing through both medial canthi was drawn on the photographs using Photoshop. From the horizontal line, three vertical lines were drawn passing through the lateral canthus, the center of pupil, and the medial canthus to the superior margin of eyebrow. Lateral brow height (H1), middle brow height (H2), and medial brow height (H3) were measured from the superior eyebrow margin passing through the lateral canthus, the center of pupil, and the medial canthus to horizontal line, respectively (Fig. 4). The BH was taken as the average of H1, H2, and H3.
Statistical Analysis
The statistical analyses were performed using statistical package for the social sciences (SPSS) version 14.0 for Windows. The changes in preoperative and postoperative MRD1, %CEA, and BH were compared using paired t tests. The statistical significance of the difference was determined when p < 0.05 based on a 95% confidence level.
Results
The results are summarized in Table 1. There was an overall increase in MRD1 of 0.92 mm (from 1.92 ± 0.86 to 2.84 ± 1.13 mm) in the total patient group after upper blepharoplasty. MRD1 increased the least when skin excision with the nonburied suture fixation technique (0.55 mm) was performed, increasing from 2.3 to 2.8 mm, whereas it increased the most in blepharoplasty with simultaneous ptosis correction (1.22 mm), increasing from 1.55 to 2.77 mm. The result was statistically significant (p < 0.05).
The %CEA increased from 62.1 to 76.6% (increment of 14.5%) in the total patient group postoperatively. The increment in %CEA was greatest in the blepharoplasty with simultaneous ptosis group, at 19.9% (from 527 to 72.5%), whereas it was smallest in the skin excision with buried suture fixation group, at 10.6% (from 72.3 to 82.9%). The result was statistically significant (p < 0.05).
In the total patient group, the BH decreased from 29.4 to 26.7 mm (9.2%). The BH was reduced most in the midpupillary axis (H2; 10.6%) compared to the lateral canthus axis (H1; 9.4%) and medial canthus axis (H3; 7.1%). It was reduced most in blepharoplasty with simultaneous ptosis correction (10.8%) and least in blepharoplasty with skin excision without fixation (7.0%). The result was statistically significant (p < 0.05).
Complications are summarized in Table 2. In the blepharoplasty with skin excision only group, there were two complications in 20 patients (10%), namely undercorrection and asymmetry of double folds. In the blepharoplasty with skin excision and nonburied suture fixation group, there was one complication among 15 patients (6.6%), representing undercorrection. In the blepharoplasty with skin excision and buried suture fixation group, there were four complications in 55 patients. Two cases involved undercorrection, and the other two involved asymmetries of double folds and abnormal eyelid contour. Finally, of 55 patients undergoing blepharoplasty with simultaneous ptosis correction, complications occurred in 14 patients (25%), with eight undercorrection cases, two cases of asymmetry of double folds, three overcorrection cases, and one abnormal eyelid contour case. There was no significant difference in the complication rate among the three groups except for blepharoplasty with simultaneous ptosis correction.
Discussion
The eyes are important facial aesthetic structures that define one’s overall appearance and beauty. The morphological differences of the eyelids due to ethnicity have been well described in the literature. Typical Asian eyes are characterized by puffiness of the upper eyelid with a low or absent supratarsal crease (single eyelid), laxity of supratarsal skin, the presence of medial epicanthal folds, a vertically narrowed palpebral fissure, and upslanting appearance, which gives the impression of tiredness [9–11]. In contrast, individuals with wider palpebral fissures and double-eyelid creases are culturally perceived as more friendly and alert. This cultural ideal of beauty has driven the desire to have double-eyelid surgery [12, 13]. Generally, the surgical goals in aesthetic and rejuvenating upper blepharoplasty include restoration of volume, the creation or accentuation of double-eyelid folds with an arched contour, and a well-defined eyeshadow space [14].
In contrast to the previous classification, which was divided into simple and anchor (complex) blepharoplasty [7, 15], we proposed an operative classification for incision upper blepharoplasty. This is classified into four types according to the methods used to create a double-fold (supratarsal) crease and simultaneous ptosis correction. The first type, blepharoplasty with skin excision only, is indicated for patients who already have a prominent double eyelid but exhibit redundant skin. The second type, blepharoplasty with skin excision and tarsal fixation, is performed for patients with weak double eyelids and redundant skin. The third type, blepharoplasty with skin excision and tarsal fixation with buried suture fixation, is indicated for patients with redundant skin but without double eyelids. Finally, the fourth type, blepharoplasty with simultaneous ptosis correction, is utilized for patients with senile or subclinical ptosis requesting upper blepharoplasty.
In the presence of redundant skin, this technique of upper blepharoplasty will include an excision of a strip of upper eyelid skin, as judged clinically with the pinch test. This redundant skin is one of the prominent signs of periorbital aging. Its removal is a cornerstone of upper eyelid rejuvenation, allowing a smooth arched eyelid crease with desirable supratarsal skin of 2–3 mm to be created [16]. This is favored by some female patients who wish to apply makeup and have it remain visible on the supratarsal skin. The design of this skin excision is well planned to avoid postoperative lagophthalmos or corneal exposure. Generally, the nasal half of the skin should be excised more conservatively than the temporal quarter. The skin excision will have the advantages of creating a more prominent eyelid crease in addition to facilitating dissection of subsequent layers of tissue [17]. Nevertheless, skin excision may be preferable in all patients, especially young individuals who are suitable for nonincision upper blepharoplasty but prefer an incision technique for its longer-lasting crease formation.
The concept of volume restoration and preservation has been emphasized in upper blepharoplasty in recent years [3]. The removal of redundant skin of the upper eyelid carried out conservatively is adequate for volume conservation as determined by the senior author to prevent an unnatural and sculpted appearance, as advocated in previous literature [18, 19]. The same principle is applied when dealing with the excision of OOM and pre-aponeurotic fat. This technique will often preserve most of the muscle and fat unless there is bulkiness or fat prolapse of the upper eyelids noted preoperatively. In skin excision without the fixation technique, only the skin is raised from the underlying OOM, preserving the muscle and fat. In techniques in which skin-to-tarsus or aponeurosis fixation will be performed, only a narrow strip of muscle overlying the superior tarsus is excised to expose it; this facilitates the suture fixation. As the excision of the strip of muscle can lead to disruption of the levator aponeurosis to the tarsus, predisposing patients to postoperative ptosis, thus suture fixation of the tarsus or aponeurosis is required; this is also necessary to ensure well-defined crease formation. Our experience shows that the aesthetic outcome of volume preservation is superior to tissue resection in upper blepharoplasty, although this was not quantified in the current study.
Aesthetic objectives with exact anthropometric analysis need to be defined to achieve consistent surgical outcomes in rejuvenating procedures [20]. Objective evaluations of functional and aesthetic outcomes in blepharoplasty are essential for preoperative planning and comparison of the results between various techniques. Conventionally, the eyelid and eyebrow measurements are performed via graduated ruler clinical measurement, which will result in large interobserver variation and inaccuracy in quantifying the pre- and postoperative changes after blepharoplasty. Measurements of the palpebral fissure by MRD1, marginal limbal distance (MLD), and vertical height of the palpebral fissure (VPH) are commonly used for this evaluation [21, 22]. However, because the measurements are one-dimensional figures that measure the distance between two points, they are unable to measure a three-dimensional ocular surface. Results of these measurements could be different between experienced surgeons and nonexperienced surgeons. It also makes patients nervous. Therefore, in our study, we measured the percentage of corneal exposure area which shows a two-dimensional area, by using a digital photographic technique, Adobe Photoshop and ImageJ in a simple method. It appears to be a substantially more convenient and accurate method for eyelid measurement.
Conclusion
Through this study, it was demonstrated that upper blepharoplasty with or without ptosis correction brings about improvement in the palpebral fissure, especially when it comes to lid fissure size changes. Although blepharoplasty with buried or nonburied suture approaches for double-fold creation clearly results in subjective satisfactory changes of the eyelids, the actual measured difference was not significant when compared to blepharoplasty with skin excision only. This numerically measured preoperative and postoperative palpebral fissure improvement will be helpful for operation outcome measurement.
References
Han KH, Yeo HJ, Choi TH, Son DG, Kim JH (2010) Intratarsal fixation at the same level as the skin incision to reduce asymmetric double eyelids: evaluation of symmetry using photogrammetry. Ann Plast Surg 64:259–265
Yoon KC, Park SH (1998) Systematic approach and selective tissue removal in blepharoplasty for young Asians. Plast Reconstr Surg 102:502–508
Lee JW, Baker SR (2013) Esthetic enhancements in upper blepharoplasty. Clin Plast Surg 40:139–146
Park DH, Kim YK (2008) Blepharoplasty techniques in Asians. In: Mirrafati SJ, Shiffman MA, Lam SM (eds) Simplified facial rejuvenation. Springer, Berlin, pp 457–470
Ma FY, Cheng MS (2010) Mini-incision double eyelidplasty. Aesthet Surg J 30:329–334
Fernandez LR (1960) Double eyelid operation in the oriental in Hawaii. Plast Reconstr Surg Transpl Bull 25:257–264
Flowers RS (1993) Upper blepharoplasty by eyelid invagination. Anchor blepharoplasty. Clin Plast Surg 20:193–207
Bae TH, Kim JC, Kim WS, Kim HK, Kim SH (2007) A photogrammetic study of the eyes in Korean youths. J Korean Soc Plast Reconstr Surg 34:37–43
Shunsuke Y, Kiyoshi M, Hideo K (2000) An anatomical structure which results in puffiness of the upper eyelid and a narrow palpebral fissure in the Mongoloid eye. Br J Plast Surg 53:466–472
Kim MK, Rathbun JE, Aguilar GL, Seiff SR (1989) Ptosis surgery in the Asian eyelid. Ophthal Plast Reconstr Surg 5:118–126
Zhaung H, Zhaung H, Yu H et al (2006) A new Z-epicanthoplasty and a concomitant double eyelidplasty in Chinese eyelids. Plast Reconstr Surg 118:900–907
Rhee SC, Woo KS, Kwon B (2012) Biometric study of eyelid shape and dimensions of different races with references to beauty. Aesth Plast Surg 36:1236–1245
Park DH, Choi WS, Yoon WS, Song CH (2008) Anthropometry of Asian eyelids by age. Plast Reconstr Surg 121:1405–1413
Codner MA, Kikkawa DO, Korn BS, Pacella SJ (2010) Blepharoplasty and brow lift. Plast Reconstr Surg 126:1e–17e
Jr JF, Ellis M (2013) Blepharoplasty. In: Nelligan PC (ed) Plastic surgery. Elsevier, London, pp 108–137
Friedland JA, Lalonde DH, Rohrich RJ (2010) An evidence-based approach to blepharoplasty. Plast Reconstr Surg 126:2222–2229
Chen WP (2006) Asian blepharoplasty steps: the first vector. In: Chen WP (ed) Asian Blepharoplasty and the eyelid crease. Butterworth Heinemann, Los Angeles, pp 61–68
Rohrich RJ, Coberly DM, Fagien S, Stuzin JM (2004) Current concepts in aesthetic upper blepharoplasty. Plast Reconstr Surg 113:32e–42e
Fagien S (2002) Advanced rejuvenative upper blepharoplasty: enhancing aesthetics of the upper periorbita. Plast Reconstr Surg 110:278–291
Matros E, Garcia JA, Yaremchuk MJ (2009) Changes in eyebrow position and shape with aging. Plast Reconstr Surg 124:1296–1301
Morris CL, Morris WR, Fleming JC (2011) A histological analysis of the mullerectomy: redefining Its mechanism in ptosis repair. Plast Reconstr Surg 127:2333–2341
Park DH, Jung JM, Song CH (2008) Anthropometric analysis of levator muscle function. Plast Reconstr Surg 121:1181–1187
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Park, Ks., Park, D.DH. Objective Outcome Measurement After Upper Blepharoplasty: An Analysis of Different Operative Techniques. Aesth Plast Surg 41, 64–72 (2017). https://doi.org/10.1007/s00266-016-0747-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-016-0747-1