Abstract
Introduction
Neurogenic hip dislocation is quite common in children with cerebral palsy (CP). The purpose of this study was to evaluate the long-term outcome of single-event multilevel surgery (SEMLS) in combination with hip reconstruction by using a periacetabular osteotomy as described by Dega concerning post-operative remodeling and plasticity of the femoral head post-operatively.
Methods
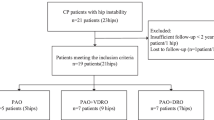
A total of 72 patients with CP as the primary disease and in whom a complex surgical hip reconstruction was performed during SEMLS between 1998 and 2004 were included in the study. There were 45 men and 27 women, with a median age of 7.6 (4.7–16.3) years at the time SEMLS was performed. The mean follow-up time was 7.7 years (4.9–11.8). X-rays were taken before and after surgery, and Rippstein 1 and 2 were used for follow-up. As the most reliable value for decentration, migration percentage (MP) as described by Reimers was used. To measure hip-joint cover at follow-up, the centre-edge angle was used. The hip was divided into four different categories according to sphericity and congruity. Using this approach, we could evaluate joint remodeling.
Results
Pre-operatively, the mean MP measured by X-ray was 68 %. Directly after surgery, this value decreased on average by 12 % and at the long-term follow-up was 16.0 % on average. A high rate of incongruence was observed on X-rays taken directly after surgery: 66 hip joints were classified as incongruent. The number of aspherical and incongruent joints decreased to 54 at the follow-up examination.
Conclusion
Data of our study with high plasticity of the hip joint suggest that even if the femoral head is deformed and a persistent incongruency after surgery is expected, hip reconstruction can be recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neurogenic hip dislocation is quite common in children with cerebral palsy (CP). Damage to the central nervous system represents the primary underlying cause of CP, and the force of spastic muscles and muscular imbalance promote lateralisation of the femoral head and decentration of the hip joint. The changes to the musculoskeletal system constitute secondary damage. The adductors and iliopsoas contribute significantly when the femoral head becomes dislocated. The vector of the resulting force is directed in lateral, superior and posterior directions and, in most cases, any defect of the acetabular rim is in this position. The proximal femur follows the altered function in accordance with increases in neck-shaft angle and femoral anteversion, forming coxa valga and coxa antetorta. The lateral capsule of the hip joint and the caput reflexum of the rectus femoris muscle causes deformity of the femoral head. Hip pain is closely associated with migration and deformity, and once the femur is deformed, the hip joint is usually painful [1].This situation deteriorates if left untreated and leads to further subluxation or dislocation, pain, loss of function and, consequently, loss of quality of life [2–4] . The risk increases with the loss of mobility and ability to walk, which is classified in the Gross Motor Function Classification Scale (GMFCS) [5, 6]. In early stages of dislocation, physiotherapy and soft-tissue lengthening of the adductor and iliopsoas muscles can be effective in improving the situation at the hip joint. Conservative treatment can influence the progression of femoral-head migration but cannot stop it [7, 8]. In some cases displacement of the hip continues and further measures need to be undertaken. Treatment with botulinum toxin and bracing are ineffective in patients with subluxated hips [9]. Moreover, there is controversy concerning the timing of surgery and the procedure itself. Some authors have reported good results with physiotherapy and a close surveillance and prevention programme [10]. Others authors use soft-tissue lengthening with good long-term results in patients in whom the migration percentage (MP) does not yet exceed 40 % [11]. In the last decade single-event multilevel surgery (SEMLS) combined with bony reconstruction of the hip has been used to treat patients with increasing dislocations [12–14] . The treatment of hip decentration begins with night splinting and physiotherapy. If the lateralisation is >40 % or the hip is dislocated, a bony reconstruction is necessary, and in recent years combining reconstruction with soft-tissue procedures has become the standard treatment to improve function. Reconstruction of the acetabulum using the technique of Dega stabilises the pelvis better than the techniques described by Chiari or Salter because it is a stable and incomplete osteotomy [15] and the medial corticalis of the os ilium is not affected.
If the pelvis remains more stable after surgery, the rehabilitation process is shorter and the complication rate lower [16]. There is evidence that the form of the femoral head and acetabulum is adjusted after a Salter procedure [3, 17] but not after periacetabular osteotomies, such as the Dega osteotomy. Further investigations are needed to prove that by following this better post-operative function, the shape and form of the hip joint will adjust. The purpose of this study was to evaluate the long-term outcome of SEMLS in combination with hip reconstruction using periacetabular osteotomy, as described by Dega, regarding remodeling and plasticity of the femoral head.
Methods
A total of 72 patients with CP as the primary disease and in whom a complex surgical hip reconstruction was performed during SEMLS between 1998 and 2004 were included in the study. Among the patients were 45 males and 27 females with a median age of 7.6 (4.7 to 16.3) at the time SEMLS was performed. The mean follow-up time was 7.7 years (4.9 to 11.8) post-operatively. The examination consisted of a standardised clinical evaluation, analysis of the latest X-ray and a specially designed questionnaire. Within that questionnaire patients were asked about their level of pain, functional development and general satisfaction with the results of surgery. We assessed patients by using the GMFCS [6]. Seven patients had GMFCS level 2, 23 had level 3, 26 had level 4 and 16 had level 5. Due to the fact that the GMFCS had not been reliably documented in the clinical records before surgery, we evaluated patients according to their status during the follow-up. Surgical procedures, concomitant diagnosis and other clinical information were collected from the clinical records. Of the follow-up investigations, 66 took place at our outpatient clinic. Six patients were surveyed at another hospital that is specialised in paediatric orthopaedics.
For radiographic measurements X-rays were taken before and after surgery; for follow-up, Rippstein 1 and 2 were used. As the most reliable value for decentration, we used migration percentage (MP) as described by Reimers [18–20]. A totally dislocated hip was classified as MP of 100 %. The defined cutoff point for a subluxation position was MP of 33 %. To measure hip-joint covering at follow-up, the centre-edge angle (CE) was used, which does not require open acetabular triradiate cartilage. The hip was divided into four different categories according to sphericity and congruity. With this approach we could evaluate joint remodeling. To measure hip congruity, we used the Rippstein-1 image and determined whether the size of the medial and lateral joint gap were the same. We considered the joint congruent if joint-space aberration was no larger than 2 mm. If the shape of the femoral head and acetabulum were lined up like circles with only a different diameter (within 1 mm), we considered the hip joint as spherical.
Questionnaire
A specific questionnaire was developed to determine reasons for the operation; complications; walking ability and walking aids; restrictions in basic functions, including positioning, personal care, sitting and standing (e.g. for transfer); and pain [visual analogue scale (VAS)] before and after the operation. The main objective was to evaluate functional improvement in after multilevel surgery with hip reconstruction. According to daily life activities, general mobility was measured using a three-scale system: better, worse, no change. Transferability was assessed as from bed alone, with assistance but weight bearing and only possible when being carried.
Surgical technique
The standard surgical technique in our department is a modified Dega acetabuloplasty, as described by Kim et al. [21], in combination with proximal femoral shortening as well as varisation and derotation osteotomy of the proximal femur (VDRSO) (Fig. 1), The bone removed from the femoral osteotomy was then reshaped and placed in the acetabular osteotomy site, as described by Sankar et al. and Mallet et al. [17, 22]. Hip-reconstruction surgery is always carried out as part of SEMLS. In 39 cases a closed reposition of dislocation was not possible, and in addition to VDRSO and the acetabuloplasty, an open reduction was required.
Consent and ethical approval
All patients/parents gave written consent for surgery and for participation in the study, which was performed in accordance with the local ethics committee and Declaration of Helsinki (World Medical Association).
Statstical analysis
For statistical evaluation, SPSS 20.0 and Student’s t test for dependent variables were used. The level of significance was defined as p < 0.05.
Results
Pre-operatively, mean MP measured by X-ray was 68 %. Directly after surgery this value decreased on average by 12 % and at the long-term examination was 16.0 % on average (Fig. 2); 89 % of patients had an MP <30 % at follow-up.
To assess shape and coverage of the femoral head, the CE angle was measured according to Wiberg. The CE angle improved during the post-operative course from 25° after surgery to 32° at follow-up (Fig. 3). This difference was significant (p < 0.001).
Congruity
Preoperatively, all 72 hip joints were incongruent, and 64 were aspheric as well. X-ray analysis immediately after surgery classified 66 hip joints as incongruent, with 58 being aspherical as well. Six hip joints are considered congruent in the first examination after surgery. One patient had a proximal femur resection after a femoral fracture. The number of patients for long-term analysis of congruity was 71. During the follow-up, hip-joint incongruity decreased to 54, with 50 of those hip joints being aspherical. The number of congruent hip joints increased from six right after surgery to 17 at follow-up and spherical hips from 0 to 7. The number of aspherical and incongruent joints decreased from 66 after surgery to 54 at follow-up. There was a shift to more physiological hip-joint morphologies: at follow-up, the number of incongruent joints decreased and a better relationship was found between femoral head and acetabulum (Fig. 4).
Function
Regarding functional changes, patients reported the following results: ability to stand with or without an assistive device was possible for 38 patients before surgery; at follow-up, 59 patients were able to maintain a standing position either with or without an assistive device. Before surgery, walking was possible for 24 patients, including those who needed an assistive device.; at follow-up, the number of ambulatory patients rose to 48, including those who were only able to take a few steps with an assistive device. In the questionnaire 50 patients stated that their overall mobility had improved. Sixteen reported that there were no significant changes and six that their overall mobility had deteriorated.
Pain
Pre-operatively, 31 patients had no pain; six had a maximum intensity of ten according to the VAS 10. At follow-up, 50 patients had no pain (VAS 0) and one had VAS 10. There was a significant reduction in pain from pre-operatively to follow-up (p < 0,001).
Discussion
Hip decentration is a common problem in patients with CP [23]. There is consensus that progressive hip subluxation with loss of function and pain should be treated surgically [12, 24]. The primary brain damage at the source of CP is closely related with gestational age and the type of CP [25, 26]. Secondary disorders affecting the locomotor and musculoskeletal systems show a typical natural history, with a windblown hip deformity typically starts in middle childhood and begins developing fixed contractures by late middle childhood [27]. Whereas no misalignment of the hip is observed at birth in these patients, the risk of subluxation increases with the disability and ability to walk, which can be classified by using the GMFCS. For all patients, the risk of hip dislocation is ∼35 % [2, 21]. In the period before hip surveillance programmes, as described by Hägglund [10], the reason for hip reconstruction often was pain and loss of function. In these cases the femoral head was often deformed and had an impression from the lateral capsule and caput reflexum of the rectus femoris muscle. Indeed, hip pain in patients with CP is closely associated with migration and deformity [1]. Patients in our study had pre-operative decentration with an MP of 68 %. Only six patients experienced maximum pain (VAS 10), but there was a high rate of incongruent and aspherical hip joints. However, MP according to Reimers appears to be a reliable tool for pre- and post-operative monitoring [28]. MP provides no information about femoral-head deformity. Goldschmidt recommended an intra-operative decision after inspecting the femoral head: if there is a loss of >50 % of the articular cartilage, reduction is not indicated, and the author preferred using salvage procedures [29].
The indication for hip surgery in our study was not hip pain but decentration of the femoral head measured using the MP, which was 68 % pre-operatively. There seems to be a relationship between hip-joint deformity and pain, as reported by Boldingh [1]. Long-term examination showed a shift to more congruent and physiological hip-joint morphologies and a significant reduction of pain. Post-operative MP results were in line with the literature [3]. Jozwiak et al. reported good results after bony reconstruction of the hip joint with pelvic osteotomy, as described by Dega. Included in that study were 30 patients and an almost five year follow-up; MP was reduced from 98.9 % to 15.9 %. [30]. The slight increase in MP in our study from post-operative to long-term examination was in line with other reports [3]. One-stage reconstruction during SEMLS seems to be the standard procedure [21]. Sankar et al. reported good results after one-stage reconstruction, with hip-joint range of motion and walking ability significantly improved. Pain reduction was impressive, and hip stability was excellent, even after 16.7 years [17]. Soft-tissue procedures and other conservative treatment can influence progression of femoral-head migration but cannot stop it [7, 8]. If the MP is >60 % or a defect of the acetabular rim is present—which in most cases is laterally, superiorly and posteriorly directed—bony reconstruction of the hip should be performed to re-establish good coverage and joint shape [12, 31]. Salter osteotomies in cases of a high hip dislocation produced good functional results and better congruity at long-term follow up [3]. With the surveillance programmes described by Hägglund [10] and the Australian Hip Surveillance Working Group [32, 33], it is possible to detect hip decentration in patients with CP very early, and situations with a high hip dislocation with destruction of the femoral head can be avoided. The technique used currently for bony hip reconstruction in cases of decentration in patients with CP is the modified Dega osteotomy [21], which gives a better coverage of the femoral head in the superior and posterior part of the acetabulum.
Jozwiak et al. reported good results after bony reconstruction of the hip joint with pelvic osteotomy, as described by Dega. MP could be reduced from 98.9 % to 15.9 %. However, no information is given about functional abilities [30]. Al-Ghahir investigated the differences between pelvic osteotomy combined with a VDRSO and VDRSO alone. The authors showed that at a follow-up of 4.4 years, VDRSO alone is not as effective as a combined procedure in terms of loss of coverage and risk of recurrence and repeat surgery [34]. The conclusion that reconstruction surgery should be carried out if the MP is >60 % and that periacetabular osteotomy should be combined with VDRSO is in line with results of our study, with a mean MP of 68 % that was reduced after surgery to 12 %. The VDRSO alone has less influence on congruity than the combination of VDRSO and a Dega osteotomy.
In our long-term results was a shift to more physiological hip-joint morphologies, and hip pain decreased significantly. It seems that the shape of the hip joint adapts to a more physiological function, and form follows function. Only a few papers have been published about improving congruity of the hip joint after reconstruction surgery. Only regarding the Salter operation has a report appeared on restoring joint congruity in CP patients after hip-reconstruction surgery [3]. That study showed a shift to more congruent hip-joint morphologies and pain reduction in the follow-up examination. No further data about the development of congruity and hip pain are currently available in the literature.
Our investigation suggests that hip joints of a growing patient are highly plastic and adaptable if a situation is created at surgery in which the femoral head and acetabulum are placed in a nearly natural position. Krebs et al. reported on a group of 54 severely affected CP patients and reported a great reduction in pain at a nearly five year; functional improvement was only visible with the patient lying down, however. Sitting and standing were not significantly influenced, and self-reliance in everyday life did not change after the index operation [35].
The more these patients are affected by hip subluxation, the more likely they are to be suffering from pain [36]. If severe pain develops, there is consensus that surgery should be performed to relieve it. Pain reduces time in a wheelchair and thus participation in activities of daily living. Prevention programmes such as that described by Hägglund [10] and the Australian Hip Surveillance Working Group [32, 33] avoid painful hips, and hip surgery is not performed unless pain and femoral-head destruction has already developed. The MP according to Reimers appears to be a reliable tool for pre- and post-operative monitoring [23]. Operative treatment planning starts if X-rays show an MP >40 %, even if a clinical correlate is lacking.
According to our results and in accordance with the literature, we suggest that multilevel surgery combined with VDRSO and transiliacic osteotomy—a modified Dega osteotomy—should be carried out if the MP is >40 % and the patient is > five years. Functional benefits are remarkable, and pain and femoral-head destruction can be effectively prevented. Coverage remains stable over a long period, even during the pubertal growth spurt. The risk of recurrence and subluxation is rather small. We observed good hip stabilisation, a low deformity recurrence rate and an impressive morphological adjustment of the hip with a reduction of hip pain. Data from our study and high hip-joint plasticity suggest that even if the femoral head is deformed and a persistent incongruency after the surgery is expected, hip reconstruction can be recommended.
References
Boldingh EJ, Jacobs-van der Bruggen MA, Bos CF, Lankhorst GJ, Bouter LM (2005) Determinants of hip pain in adult patients with severe cerebral palsy. J Pediatr Orthop B 14(2):120–125
Moreau M, Drummond DS, Rogala E, Ashworth A, Porter T (1979) Natural history of the dislocated hip in spastic cerebral palsy. Dev Med Child Neurol 21(6):749–753
Braatz F, Eidemüller A, Klotz MC, Beckmann NA, Wolf SI, Dreher T (2014) Hip reconstruction surgery is successful in restoring joint congruity in patients with cerebral palsy: long-term outcome. Int Orthop 38(11):2237–2243
Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R, Reddihough D, Graham KH (2006) Hip displacement in cerebral palsy. J Bone Joint Surg (Br) 88-A:121–129
Palisano RJ, Hanna SE, Rosenbaum PL et al (2000) Validation of a model of gross motor function for children with cerebral palsy. Phys Ther 80:974–985
Graham HK (2005) Classifying cerebral palsy. J Pediatr Orthop 25(1):127–128
Terjesen T, Lie GD, Hyldmo AA, Knaus A (2005) Adductor tenotomy in spastic cerebral palsy. A long-term follow-up study of 78 patients. Acta Orthop 76(1):128–137
Jung NH, Heinen F, Westhoff B, Doederlein L, Reissig A, Berweck S, Linder-Lucht M, Schandelmaier S, Mall V, German Abo study group (2011) Hip lateralisation in children with bilateral spastic cerebral palsy treated with botulinum toxin type a: a 2-year follow-up. Neuropediatrics 42(1):18–23
Graham HK, Boyd R, Carlin JB, Dobson F, Lowe K, Nattrass G, Thomason P, Wolfe R, Reddihough D (2008) Does botulinum toxin a combined with bracing prevent hip displacement in children with cerebral palsy and “hips at risk”? A randomized, controlled trial. J Bone Joint Surg Am 90(1):23–33
Hägglund G, Andersson S, Duppe H, Lauge-Pedersen H, Nordmark E, Westbom L (2005) Prevention of dislocation of the hip in children with cerebral palsy. The first ten years of a population-based prevention programme. J Bone Joint Surg Br 87:95–101
Miller F, Cardoso Dias R, Dabney KW, Lipton GE, Triana M (1997) Soft-tissue release for spastic hip subluxation in cerebral palsy. J Pediatr Orthop 17(5):571–584
Valencia FG (2010) Management of hip deformities in cerebral palsy. Orthop Clin North Am 41(4):549–559
Karol LA (2004) Surgical management of the lower extremity in ambulatory children with cerebral palsy. J Am Acad Orthop Surg 12(3):196–203
Saraph V, Zwick EB, Zwick G, Steinwender C, Steinwender G, Linhart W (2002) Multilevel surgery in spastic diplegia: evaluation by physical examination and gait analysis in 25 children. J Pediatr Orthop 22(2):150–157
El-Sayed M, Ahmed T, Fathy S et al (2012) The effect of Dega acetabuloplasty and Salter innominate osteotomy on acetabular remodeling monitored by the acetabular index in walking DDH patients between 2 and 6 years of age: short- to middle-term follow-up. J Child Orthop 6(6):471–477
Karlen JW et al (2009) The Dega osteotomy: a versatile osteotomy in the treatment of developmental and neuromuscular hip pathology. J Pediatr Orthop 29(7):676–682
Sankar WN et al (2006) Long-term follow-up after one-stage reconstruction of dislocated hips in patients with cerebral palsy. J Pediatr Orthop 26(1):1–7
Faraj S, Atherton WG, Stott NS (2004) Inter- and intra-measurer error in the measurement of Reimer’s hip migration percentage. J Bone Joint Surg 86:434–437
Hägglund G, Lauge-Pedersen H, Wagner P (2007) Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord 26(8):101
Reimers J (1980) The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 184:1–100
Kim HT, Jang JH, Ahn JM, Lee JS, Kang DJ (2012) Early results of one-stage correction for hip instability in cerebral palsy. Clin Orthop Surg 4(2):139–148
Mallet C, Ilharreborde B, Presedo A et al (2014) One-stage hip reconstruction in children with cerebral palsy: long-term results at skeletal maturity. J Child Orthop 8(3):221–228
Terjesen T (2012) The natural history of hip development in cerebral palsy. Dev Med Child Neurol 54:951–957
Koman LA, Smith BP, Shilt JS (2004) Cerebral palsy. Lancet 363(9421):1619–1631
Okumura A, Hayakawa F, Kato T, Kuno K, Watanabe K (1997) MRI findings in patients with spastic cerebral palsy. I: Correlation with gestational age at birth.Dev. Med Child Neurol 39(6):363–368
Okumura A, Kato T, Kuno K, Hayakawa F, Watanabe K (1997) MRI findings in patients with spastic cerebral palsy. II: Correlation with type of cerebral palsy. Dev Med Child Neurol 39(6):369–372
Miller F (2005) Cerebral palsy. Springer Sci. 601
Kim SM, Sim EG, Lim SG, Park ES (2012) Reliability of Hip migration index in children with cerebral palsy: the classic and modified methods. Ann Rehabil Med 36(1):33–38
Goldschmidt RB (1998) Instaility of the hip in cerebral palsy. Curr Orthop 12:40–50
Jozwiak M, Koch A (2011) Two-stage surgery in the treatment of spastic hip dislocation--comparison between early and late results of open reduction and derotation-varus femoral osteotomy combined with Dega pelvic osteotomy preceded by soft tissue release. Ortop Traumatol Rehabil 13(2):144–154
Flynn JM, Miller F (2002) Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg 10(3):198–209
Wynter M, Gibson N, Kentish M, Love S, Thomason P, Kerr GH (2011) The development of Australian standards of care for Hip surveillance in children with cerebral palsy: how did we reach consensus? J Pediatr Rehabil Med 4(3):171–182
Wynter M, Gibson N, Willoughby KL, Love S, Kentish M, Thomason P, Graham HK; National Hip Surveillance Working Group (2015) Australian hip surveillance guidelines for children with cerebral palsy: 5-year review. Dev Med Child Neurol. Apr 3
Al-Ghadir M et al (2009) Combined femoral and pelvic osteotomies versus femoral osteotomy alone in the treatment of hip dysplasia in children with cerebral palsy. J Pediatr Orthop 29(7):779–783
Krebs A, Strobl WM, Grill F (2008) Neurogenic hip dislocation in cerebral palsy: quality of life and results after hip reconstruction. J Child Orthop 2(2):125–131
Hodgkinson I et al (2001) Hip pain in 234 non-ambulatory adolescents and young adults with cerebral palsy: a cross-sectional multicentre study. Dev Med Child Neurol 43(12):806–808
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Braatz, F., Staude, D., Klotz, M.C. et al. Hip-joint congruity after Dega osteotomy in patients with cerebral palsy: long-term results. International Orthopaedics (SICOT) 40, 1663–1668 (2016). https://doi.org/10.1007/s00264-015-3013-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3013-2