Abstract
Background
At birth, no difference exists between the hips of children with spastic cerebral palsy and the hips of other children. The typical pathologic deformities of the hips in children with spastic cerebral palsy develop as the child gets older. One of our goals was to evaluate the change in quality of life of children with cerebral palsy after hip reconstruction. For classification of the children’s condition, we assessed sitting and standing abilities and used the Gross Motor Function Classification System. To evaluate the effect of hip dislocation on the spine, we assessed symmetry while the patient was lying down, sitting, and standing.
Methods
The results of surgical reconstruction of hip joints in 54 patients with severe cerebral palsy who had 66 severely subluxated or dislocated hip joints were retrospectively analyzed. The study was based on a research questionnaire with a mean follow-up of 4 years 10 months. The purpose of the questionnaire was to evaluate the pain, functional abilities, symmetry, and independence of the patients by using the modified Barthel index.
Results
Pain was fully relieved in 62 and was eased in 35% of preoperatively painful hips. The functional abilities of sitting and standing were not influenced statistically significantly by the operation. An improvement in sitting symmetry was observed in 40% and improvement in lying symmetry was observed in 32% of the patients. The mean center-edge angle improved from −24.9° ± 39° (mean ± standard deviation) to 25.9° ± 14°. The acetabular index improved from 30.2° ± 8° to 17.1° ± 7°.
Conclusions
The independence of the patients, based on the modified Barthel index, did not change significantly after surgery. Most improvements in quality of life were observed in those patients who had pain in the hip before the operation as a result of reduction of pain and improved mobility of the hip.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
At birth, no difference exists between the hips of children with spastic cerebral palsy and the hips of other children [1]. The typical pathologic deformities of the hips in children with spastic cerebral palsy—femoral anteversion and coxa valga antetorsa—are manifested during the development of the child [2–4].
The driving force of normal development of the hip is learning sitting and standing abilities [5, 6]. According to Heimkes et al. [5], reduced activity of the hip abductor muscles in comparison to the spastic adductors leads to diminished growth of the greater trochanter. The consequences are that the main direction of the hip abductors becomes more vertical and the longitudinal growth plate of the femoral neck stays in a horizontal position. This leads to the commonly known coxa valga [5, 6].
The increased femoral anteversion is also a consequence of the reduced activity of the gluteus maximus, medius, and minimus muscles in comparison to the spastic adductors [5]. The study presented by Laplaza et al. [4] shows increased femoral anteversion for persons of all ages with cerebral palsy. Fabry et al. [2] reported mean femoral anteversion of 39° for persons with cerebral palsy, which is 15° more than in the reference group with normal femoral anteversion.
According to Heimkes et al. [5], for untreated patients, dislocation of the hip typically occurs at age 2–7 years with a maximum at the age of 6 years. A study presented by Samilson et al. [7] showed that the dislocation occurs at a mean age of 7 years. In a study presented by Vidal et al. [8], the mean age for occurrence of dislocation of the hip was 10–12 years, with earlier dislocation occurring in nonambulant children. In our patients, dislocation of the hip typically occurred at the age of 7 years and at the age of 14–17 years, after puberty.
One of our goals was to evaluate the change in quality of life of children with cerebral palsy after hip reconstruction. The International Classification of Impairments, Disabilities and Handicaps [9, 10], which is published by the World Health Organization, is a system for classifying the consequences of disease. A patient can be classified in three dimensions. The dimensions are impairment (organ and body dimension), disability (individual dimension), and handicap (social dimension). Impairment includes body function and body structure. Disability covers the complete range of activities performed by a person. Handicap classifies areas of life in which a person is involved, areas in life that a person has access to, social opportunities, and social barriers. Any disorder in the body (e.g., anatomic structures, physiologic and psychologic functions) leads to impairment. Impairment can lead to limitation of activities (e.g., walking, self-care). Activity limitation can lead to participation restriction (e.g., participation in nutrition, participation in mobility). The goal of treatments should be to improve the activities and participation by improving bodily disorders.
In the literature, few articles regarding quality of life and assessment scales are available. Ketelaar et al. [11] present an overview of assessment scales for children with cerebral palsy. The assessment scales include two main groups: discriminative and evaluative indices. A discriminative index distinguishes between persons with and without a particular characteristic or function. An evaluative index is used to measure the magnitude of change in function over time or after treatment. We decided to use the modified Barthel index [12] as a questionnaire for retrospective evaluation for measuring the independence of the patient, as one part of quality of life.
The Barthel index is an evaluative index. It was developed for quantifying self-confidence of disabled persons. The Barthel index includes ten items, and the participant receives a score of his or her degree of independence in the performance of each item. The items are feeding, bathing, grooming, dressing, bowel control, bladder control, toilet use, transfers (bed to chair and back), mobility, and stair climbing. The scores of the different items are summed to form an overall index. The index ranges from 0 to 100, with 0 representing complete dependence and 100 representing complete independence in the performance of all items. The original Barthel index [13] scales each item in three categories (fully dependent, assistance required, and fully independent). The index ranges from 0 to 20. The modified Barthel index defines three subcategories for the category of assistance required: attempts task but unsafe, moderate help required, and minimal help required. The purpose of the use of subcategories is to improve sensitivity.
One important factor for quality of life—pain—is not mentioned in the evaluation indices but is a very important factor for the patients. Thus, we added a visual analogue scale to assess pain.
For classification of the children’s condition, we used the gross motor function classification system (GMFCS) [27]. The children are classified in five levels. Level 1 is the mildest, with good walking abilities. Until level 3 children are able to walk with an assistive device. Level 4 has good control of upper extremities but no walking abilities, and Level 5 has no weight bearing and needs a sitting device.
Further we assessed sitting and standing abilities. Sitting ability was classified into free sitting, sitting with little support, sitting in a sitting device, and no sitting ability. Standing ability was classified into free standing, standing with little assistance, standing with moderate support like a walking device, standing only with the assistance of one or two persons, and no standing ability. To evaluate the relationship between hip dislocation and spine, we assessed symmetry while the patient was lying down, sitting, and standing. Neurogenic scoliosis with pelvic obliquity and windblown deformity with adduction of one hip and abduction of the other hip can increase the rate of hip dislocation.
Materials and methods
We retrospectively analyzed the radiographs and research questionnaires of our patients who underwent reconstruction of neurogenic hip dislocation between August 1989 and March 2000. All patients had severe spastic cerebral palsy and neurogenic hip dislocation or subluxation. Fifty-four patients (66 hips) were included in the study. Two patients were lost to follow-up because of death unrelated to orthopaedic conditions. The guardian of one patient (patient 18) did not allow clinical or radiographic examinations, but the attendants in that case were able to answer the questionnaire.
The radiographs of 51 patients (63 hips) were obtained during an average follow-up period of 4 years 10 months (range, 11 months to 11 years 10 months). The research questionnaires were answered by 45 patients (57 hips), with an average duration of follow-up of 4 years 9 months (range, 11 months to 11 years 3 months). The guardian of three patients (patients 15, 17, and 31) did not allow evaluations. Four patients (patients 4, 16, 45, and 49) could not be located. The radiographs of these seven patients were obtained from the most recent orthopaedic follow-up examination at the hospital.
The mean patient age at the time of operation was 8 years 6 months (range, 1 year 8 months to 19 years 7 months). The mean age at follow-up was 13 years 3 months (6 years 10 months to 23 years 7 months).
The functional status according to the GMFCS showed walking abilities (levels 1–3) in ten hips (16%) and no walking abilities (levels 4 and 5) in 54 hips (84%). The neurological diagnosis was whole body involvement cerebral palsy in 55 hips (86%), diparesis in seven hips (11%), and one patient with two affected hips had a Pelizaeus Maerzbacher Syndrome. The X-rays showed dislocation in 42 hips (66%) and subluxation in 22 hips (34%). The hip was counted as dislocated if the CE-angle was below 0°, and subluxated if the CE-angle was between 0° and 20°.
Ten patients had undergone previous soft-tissue surgery, one patient had undergone angulation osteotomy, and two patients had undergone hip reconstruction. Twenty-six (46%) of the 57 hips for which returned questionnaires were available were preoperatively painful, 26 were free from pain, and five were unquantified. Twenty-five hips (44%) showed no weight bearing preoperatively. For 32 hips (56%), the patients were able to stand with the use of different aids, and none of the patients had free-standing ability. For 13 hips (23%), the patients had free-sitting ability; for 40 hips (70%), the patients required sitting support; and for four hips (7%), the patients were bedridden.
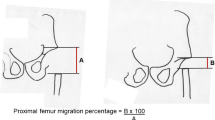
Radiographs were obtained preoperatively, during the immediate postoperative period, and at the most recent follow-up examination. The centration of hip joints was assessed radiographically by using the center–edge (CE) angle described by Wiberg [14] and the acetabular index described by Cornell [1] and Hilgenreiner [15].
The research questionnaire evaluated the modified Barthel index [12], sitting and standing abilities, symmetry of sitting and lying down, and hip joint pain preoperatively, approximately 6 months after surgery, and at the most recent follow-up.
There were some minor postoperative complications. One patient had a small superficial wound dehiscence, one had increased sensitivity to pain for several month, one had a haematoma in the adductor region after adductortenotomy which was healed by conservative antibiotic treatment, and one patient had a small decubitus on the malleolus from the cast. One patient had a moving of a K-wire which had to be removed two months after primary surgery.
Operative procedure
A Salter et al. [16] innominate osteotomy was performed in 25 hips and a Pemberton [17, 18] osteotomy in 39. In 58 hips, intertrochanteric varus derotation and shortening osteotomy [18–20] was performed. Shortening of the femur is an important part of the surgical procedure when a combined pelvic procedure and proximal femoral osteotomy is performed to prevent osteonecrosis of the femoral head. Stasikelis et al. [21] reported incidence of osteonecrosis of up to 46% after surgical hip reconstruction. Additional soft-tissue surgery [19, 22] was performed in 52 hip operations, depending on the individual situation of each patient, and included hip adductors and hip flexors.
For postoperative pain prophylaxis, since 1995, patients received anaesthesia with use of an epidural perfusor for approximately three days. In addition, they received orally administered spasmolytic medicine (baclofen) during the period of immobilization. From our experience patients with spasticity can have pain in the cast due to spasticity. This pain can be relieved by oral baclofen.
Postoperative immobilization was accomplished with a hip spica cast, including both legs in slight abduction for approximately 2 weeks. Afterward, the cast was cut off in shell form and used as a positioning device for the whole day and night. The patients started with a passive mobilization program with hip flexion up to 60°, no abduction, no rotation. This passive mobilization program was adhered to for approximately 4 weeks. This early mobilization program was started to improve the mobility of the hip. Six weeks postoperatively, patients underwent control radiography, the positioning device was removed, physiotherapy was begun, and weight bearing was allowed. Before 1996, each patient had a hip spica cast for 6–8 weeks.
Results
Pain after hip reconstruction
Figure 1 shows the intensity of pain before and after surgery. The patients, or their attendants, quantified their pain on a scale from 0 point (no pain) to 6 points (maximum pain). The number of painless hips was markedly increased after the surgical procedure (P < 0.001). Pain of maximum intensity (5–6 points) was not reported after surgery.
In our patients, 46% (26 hips) reported no pain neither before nor after surgery (Fig. 2). Only one patient who was preoperatively painless reported postoperative pain. This patient had been painless for one year after surgery, and then the pain developed because of subluxation of the hip on the contralateral side.
Among the preoperatively painful hips, 62% (16 hips) were postoperatively completely painless and 35% (nine hips) achieved good improvement regarding pain. We were able to reduce pain for these patients. Preoperatively, most patients experienced pain even when lying or sitting. Postoperative pain occurred primarily when moving the hip. No pain during sitting or lying were reported at the latest follow up. Therefore, even patients with postoperative pain achieved good improvement in their quality of life after surgery.
Functional abilities after surgery
Functional abilities were classified by using sitting (sitting freely, sitting with little assistance, sitting with the aid of a device, bedridden) and standing (standing freely; standing with little assistance, such as holding a rail; standing with moderate assistance, such as a walking frame; standing only with the assistance of one or two persons; no weight bearing) abilities. Symmetry was quantified by the parents or attendants on a scale from 0 (asymmetric) to 3 (good symmetry) points.
Standing abilities remained unchanged in 72% (41 hips), were improved in 16% (9 hips), and were reduced in 12% (7 hips). The changes were not statistically significant (P = 0.18). Sitting abilities remained unchanged in 77% (44 hips), were improved in 14% (8 hips), and were reduced in 9% (5 hips). The changes were not statistically significant (P = 0.16). Good improvement was observed in the symmetry of lying (32%, 17 hips, P = 0.17) (Fig. 3) and sitting (40%, 21 hips, P = 0.03) (Fig. 4). Evaluation of the mean Barthel index for all patients showed a mean preoperative value of 15.1 points, with a mean improvement of 3.8 points after surgery.
Changes for patients without weight bearing
Nineteen patients were without preoperative weight bearing. Most had no free sitting abilities and required a sitting device. Good amelioration of hip pain was observed. Among eleven patients who experienced pain preoperatively, 64% (7 patients) were completely painless and 36% (4 patients) achieved good improvement regarding their pain. Symmetry of lying was improved in 35% (6 patients), and symmetry of sitting was improved in 43% (7 patients).
Evaluation of the modified Barthel index (range, 0–100 points) for these patients resulted in a very low mean average value of 6.7 points and improvement to 9.3 points after surgery. The parents and attendants reported good improvement regarding pain and general condition but only moderate changes for transfers and care giving.
Patients who were painless preoperatively but were unable to bear weight were kept painless and experienced no reluxation of the hips. Their daily living activities remained unchanged. The contentedness of the parents of these patients was significantly lower than the mean average value.
Changes for patients with weight bearing
Preoperatively, 26 patients were able to bear weight and had standing abilities that ranged from standing with the assistance of a person to free standing abilities. All preoperatively painless patients in this group remained painless. Six (60%) of ten patients who experienced pain preoperatively were free from pain after surgery, three (30%) experienced good improvement regarding pain, and one had a painless period of one year after surgery with increasing pain afterward. Evaluation of this case showed no orthopaedic reason for the increasing pain.
The mean Barthel index for these patients increased from 20.7 points preoperatively to 25.4 points postoperatively. Few changes were achieved for transfer and care giving, but some patients in this group achieved good improvement in their activities of daily living (including communication, social behavior, and mobility) after surgery.
The preoperatively painless patients who could bear weight remained painless. The good sitting and standing abilities in this group were mainly preserved and, in some cases, improved.
Radiographic findings
Radiographs were obtained before surgery, during the postoperative period, and at the most recent follow-up visit. We evaluated the center-edge angle as presented by Wiberg [14] and the acetabular index as presented by Cornell [1] and Hilgenreiner [15]. In two patients (3 hips), the acetabular index at follow-up was not determinable. The triradiate cartilage was completely ossified so that the line of Hilgenreiner could not be drawn on the radiograph.
Of 66 hip reconstructions, 63 follow-up radiographs were available, with a mean follow-up duration of 4 years 10 months (range, 11 months to 11 years 10 months). The results are shown in Table 1.
Figure 5 shows the improvement of the CE angle. Preoperatively, most patients had a negative CE angle. The mean postoperative CE angle was 25.9°. At the most recent follow-up, 45 hips (69%) had good coverage of the hip joint with a CE angle of more than 20°. Seventeen patients (26%) had a subluxation with CE angles between 20° and 0°, and one patient had a dislocation with a CE angle of −10°. This patient never had good coverage of the hip joint, and the postoperative radiograph showed a CE angle of −20°.
Figure 6 shows the improvement of the acetabular index. Preoperatively, most patients (84%, 49 hips) had an acetabular index of more than 20°. The acetabular index was improved to less than 20° in 40 hips (67%). The mean acetabular index changed from 30.2° preoperatively to 17.1° at the most recent follow up (P < 0.001).
Comparison of CE angle with intensity of pain showed that all luxated hips with a CE angle more negative than −50° resulted in severe pain. For subluxated and luxated hips up to −50° CE angle, no correlation between CE angle and intensity of pain was shown. In our patients, no correlation was shown between the preoperative intensity of pain and the postoperative improvement of pain.
For assessing the results of the surgery the functional status of the patient was much more reliable than the amount of preoperative dislocation and subluxation. Sixty-nine percent of dislocated hips were GMFCS level 5. For the subluxated hips 40% were GMFCS level 4 and 32% were GMFCS level 5.
Discussion
The literature presents extensive discussion regarding the painfulness of neurogenic hip dislocation [19] and decisions regarding hip reconstruction. Based on our experience, most dislocated hips are painful. In some patients, the hip is painful during the process of dislocation and pain disappears when the hip is fully dislocated (personal experience).
In nonambulatory patients, the pain results in limited sitting abilities and even lost sitting abilities. In those cases in which the pain disappeared after years, the patients had meanwhile lost their quality of life for years. Because of the painfulness of motion, the patients are not able to tolerate physiotherapy, with the result of aggravation of muscle shortening and joint contracture.
On the other hand, parents of patients without weight bearing who do not experience pain are not satisfied after the operation, because no obvious benefit has been achieved. All were kept free from pain, but no improvement was shown in functional abilities. These patients maintained their functional levels but did not achieve increased potential for motor development. In these patients we are very careful with the indication for surgery and wait till the hip becomes painful or the patient experiences problems due to the dislocated hip, for example windblown deformity or sitting problems.
In ambulatory patients, a dislocated hip results in diminished standing and walking abilities. If this condition remains untreated, the patients can permanently lose their functional abilities. Only one patient in our study experienced aggravation of hip pain with diminished functional abilities after surgery. This was caused by painful hip dislocation on the contralateral side. The good functional abilities of the other patients in this group were preserved.
For patients with painful hip dislocation, the decision for surgical treatment is not very difficult. We achieved reduction of pain in all our patients. These patients experienced a marked improvement in their quality of life.
In patients with good functional abilities, their abilities could be preserved and, in some cases, improved. For these patients, hip reconstruction should be considered when progressive subluxation is present and the patient is older than six years. In younger patients, prophylaxis should begin with botulinum toxin type A [23, 24] or multilevel surgery with lengthening of the adductors, rectus femoris, and iliopsoas muscles [22]. If hip reconstruction is performed only when painful hip dislocation is present in these patients, loss of sitting and standing abilities is a risk.
In one group of patients, the indication for surgery should be very restrictive. This group consists of patients with subluxated hip joints who are free from pain and who do not have any tendency to weight bearing. In these cases, surgery should be carefully prepared and discussed with parents and physiotherapists. The optimal age for surgery in this group is approximately 12 years. In older patients, the rehabilitation process takes much longer.
Because of the higher incidence of redislocation in patients with acetabular dysplasia a combined pelvic and femoral procedure should be performed [26].
To achieve good compliance, families should be advised that the rehabilitation process requires several months after hip reconstruction. Stasikelis et al. [25] reported that the average rehabilitation required to reach the preoperative functional level after femoral osteotomy was seven to ten months. This is in accordance with our experience.
The modified Barthel Index shows very low values and low postoperative variability in this severe disabled group of patients. We have to consider that most of our patients belong to levels 4 and 5 of the GMFCS. These patients usually have low levels of self confidence. Therefore this index is not reliable for documenting small changes in patients with severe forms of cerebral palsy, but the index is useful for quantifying the severity of the disability.
Changes in quality of life after hip reconstruction in patients with cerebral palsy are mainly a result of reduced hip pain and improved motion of the hip joint. Functional abilities can be preserved and, in some cases, improved.
References
Cornell MS (1995) The hip in cerebral palsy. Dev Med Child Neurol 37:3–18
Fabry G, MacEwen GD, Shands AR Jr (1973) Torsion of femur. A follow up study in normal and abnormal conditions. J Bone Joint Surg Am 55:1726–1138
Massie WK, Howorth MB (1950) Congenital dislocation of the hip. Part I. Method of grading results. J Bone Joint Surg Am 32:519–531
Laplaza FJ, Root L, Tassanawipas A, Glasser DB (1993) Femoral torsion and neck-shaft angles in cerebral palsy. J Pediatr Orthop 13:192–199
Heimkes B, Stotz S, Heid T (1992) Pathogenesis and prevention of spastic hip dislocation [in German]. Z Orthop Ihre Grenzgeb 130:413–418
Siffert RS (1981) Patterns of deformity of the developing hip. Clin Orthop Relat Res 160:14–29
Samilson RL, Tsou P, Aamoth G, Green WM (1972) Dislocation and subluxation of the hip in cerebral palsy. J Bone Joint Surg Am 54:863–873
Vidal J, Deguillaume P, Vidal M (1985) The anatomy of the dysplastic hip in cerebral palsy related to prognosis and treatment. Int Orthop 9:105–110
World Health Organization (1993) International classification of impairments, disabilities and handicaps. World Health Organization, Geneva
World Health Organization: international classification of functioning and disability. ICIDH-2. Available at http://www.who.int/ (last accessed, 18 July, 2005)
Ketelaar M, Vermeer A, Helders PJ (1998) Functional motor abilities of children with cerebral palsy. A systematic literature review of assessment measures. Clin Rehabil 12:369–380
Shah S, Vanclay F, Cooper B (1989) Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol 42:703–709
Mahoney FI, Barthel DW (1965) Functional evaluation. The Barthel index. Md State Med J 14:61–65
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand 83[Suppl 58]:1–135
Hilgenreiner H (1925) Early diagnosis and treatment of developmental dysplasia of the hip [in German]. Med Klin 21:1385–1425
Salter RB, Hansson G, Thompson GH (1984) Innominate osteotomy in the management of residual congenital subluxation of the hip in young adults. Clin Orthop Relat Res 182:53–68
Pemberton PA (1965) Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg Am 47:65–86
Gordon JE, Capelli AM, Strecker WB, Delgado ED, Schoenecker PL (1996) Pemberton pelvic osteotomy and varus rotational osteotomy in the treatment of acetabular dysplasia in patients who have static encephalopathy. J Bone Joint Surg Am 78:1863–1871
Brunner R, Baumann JU (1994) Clinical benefit of reconstruction of dislocated or subluxated hip joints in patients with spastic cerebral palsy. J Pediatr Orthop 14:290–294
Root L, Laplaza FJ, Brourman SN, Angel DH (1995) The severely unstable hip in cerebral palsy. Treatment with open reduction, pelvic osteotomy, and femoral osteotomy with shortening. J Bone Joint Surg Am 77:703–712
Stasikelis PJ, Ridgeway SR, Pugh LI, Allen BL Jr (2001) Epiphyseal changes after proximal femoral osteotomy. J Pediatr Orthop B 10:25–29
Miller F, Cardoso Dias R, Dabney KW, Lipton GE, Triana M (1997) Soft-tissue release for spastic hip subluxation in cerebral palsy. J Pediatr Orthop 17:571–584
Gormley ME, Gaebler-Spira D, Delgado MR (2001) Use of botulinum toxin type A in pediatric patients with cerebral palsy. A three-center retrospective chart review. J Child Neurol 16:113–118
Koman LA, Mooney JF 3rd, Smith B, Goodman A, Mulvaney T (1993) Management of cerebral palsy with botulinum-A toxin. Preliminary investigation. J Pediatr Orthop 13:489–495
Stasikelis PJ, Davids JR, Johnson BH, Jacobs JM (2003) Rehabilitation after femoral osteotomy in cerebral palsy. J Pediatr Orthop B 12:311–314
Noonan KJ, Walker TL, Kayes KJ, Feinberg J (2001) Varus derotation osteotomy for the treatment of hip subluxation and dislocation in cerebral palsy. Statistical analysis in 73 hips. J Pediatr Orthop B 10:279–286
Morris C, Bartlett D (2004) Gross Motor Function Classification System: impact and utility. Dev Med Child Neurol 46(1):60–65
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Krebs, A., Strobl, W.M. & Grill, F. Neurogenic hip dislocation in cerebral palsy: quality of life and results after hip reconstruction. J Child Orthop 2, 125–131 (2008). https://doi.org/10.1007/s11832-008-0080-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11832-008-0080-6