Abstract
Introduction
Hip reconstruction is an established procedure in pediatric patients with neurogenic hip dislocation. An open triradiate cartilage provides the advantage of a high plasticity of the bone which prevents an intraarticular fracture and postoperative adaptation of shape. Some patients with dislocated hips, however, arrive late. A hip reconstruction is still feasible as shown earlier but the long-term risk for osteoarthritis, and recurrence of dislocation, and functional outcome is unknown. It is the aim of our investigation to evaluate long-term clinical and radiological outcomes of hip reconstruction by Dega type pelvic osteotomy performed after fusion of the triradiate epiphyseal cartilage in patients suffering from cerebral palsy.
Material and methods
We retrospectively analyzed 43 hips in 37 patients with a hip reconstruction for correction of hip dislocation or subluxation. In all patients, the triradiate cartilage was fused before surgery. Age at surgery was 15 years and 2 months on average and follow-up time was mean 13 years 5 months.
Results
Mean Kellgren Lawrence score at final follow-up was significantly higher than at preoperative investigation (P < 0.00001). At long-term follow-up 3 of 43 hips had developed pain, and 1 of them required arthroplasty. Reimers´ migration index was stable over the years and was not higher at last follow-up compared to the index observed shortly after surgery (P = 0.857), so was the Sharp angle (P = 0.962). We found no significant reduction in the range of motion of the hip in the sagittal plane.
Conclusion
We noted mild radiological signs of osteoarthritis which possibly occur due to an intraarticular acetabulum fracture during bending down the acetabulum. Nevertheless, hip reconstruction in patients with cerebral palsy and closed triradiate cartilage remains a valuable option as it results in a stable, painless hip for more than a decade.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with neurologic movement disorders such as cerebral palsy hip dislocation is a frequently observed problem. The risk of hip dislocation is known to be associated with higher Gross Motor Function Classification System (GMFCS) levels (levels 4 and 5). Different options for surgical correction have been reported such as isolated femoral varus osteotomy, a hip reconstruction, soft tissue procedures, or salvage procedures such as a valgus osteotomy, hip fusion and proximal femoral resection. Salvage procedures can lead to a reduction of pain, but not often a complete relief of pain. Such procedures are accompanied by numerous complications and should be used only for selected patients [1, 2]. Total hip arthroplasty seems to provide similar results as in matched normal developing population concerning complications, pain relief and function [3]. In normal developing population, a total hip arthroplasty at a young age carries the risk of multiple revision surgeries during a lifetime. Life expectancy in patients with cerebral palsy is still lower than in the average population but has to be considered to be several decades [4,5,6]. It is thus highly probable that revision surgery will be necessary ifor patients with cerebral palsy also, although there is no data in the literature yet. An alternative in pediatric patients is hip reconstruction consisting of a derotation, shortening, and varus osteotomy of the proximal femur and a modified Dega/Pemberton periacetabular osteotomy [7,8,9]. This procedure provides good clinical and radiological results at short- and mid-term follow-up [10]. Ideally, it is done before the closure of the triradiate cartilage since this area is the pivot point of the pelvic osteotomy. In patients with non-fused triradiate growth plate the osteocartilagineous complex provides enough plasticity to prevent an intraarticular acetabular fracture which is considered a risk factor for premature osteoarthritis (OA). In some patients, however, hip dislocation is not recognized, neglected, or surgery is refused by care givers or parents. In these older patients, the mature pelvic bone adds the risk for an acetabular fracture during the modified Dega osteotomy. Consequently, it is advised against such osteotomies in cases with closed triradiate physis [9, 11, 12]. Grudziak et al. stated that in these cases the triradiate cartilage as a hinge for the osteotomy may be replaced by other pivots points as the sciatic notch or the pubic symphysis [13]. Robb and Brunner reported satisfactory short term results for Dega–type osteotomy performed after the closure of the triradiate physis in non-walking patients suffering from severe cerebral palsy [14].
The purpose of this study was to investigate the long-term clinical and radiological outcome of hip reconstructions in patients suffering from hip dislocation or subluxation of the hip due to cerebral palsy who underwent Dega-osteotomy after the fusion of the triradiate growth plate.
Patients and methods
We retrospectively evaluated the outcome of hip reconstruction in patients suffering from cerebral palsy who were operated on by Dega osteotomy after skeletal maturity. Skeletal maturity was defined by the fusion of the triradiate growth plate. This study was approved according to local ethics requirements (EKNZ 22/2007 and amendment PB_2018-00259).
Inclusion criteria comprised a closed triradiate cartilage and physis of the proximal femur on plain radiographs at the time of surgery and a follow-up interval of at least 5 years. A complete chart with clinical findings and pre- and postoperative anteroposterior pelvic X-ray images were mandatory.
We evaluated the degree of OA using Kellgren Lawrence score [15] and the displacement of the femoral head was rated using Reimers migration percentage (MP) [16] by analysis of standardized plain anteroposterior radiographs (Table 1).
Sharps angle was measured on the same radiographs as originally described by Sharp [17]. This method was found to be not inferior to more modern measurement techniques [18]. All radiographs were analyzed by the first and last authors. Hip pain and range of motion (ROM) in the sagittal plane were chosen for primary and secondary outcome parameters. Sagittal ROM was measured in a supine position using the Thomas test [19, 20]. Simultaneously performed soft tissue surgeries were also recorded.
We also assessed the sphericity of the femoral head (Fig. 1). For this purpose, a template with circles was overlaid on the plain hip radiograph to measure femoral head morphology. The largest and the smallest fitting circles were placed over the femoral head and the difference between the radii of these two circles was calculated. Since the contour of the femoral head changes in the plain radiograph with the altered femoral anteversion after derotation osteotomy of the proximal femur we only addressed the postoperative radiographs.
Operative technique
In all patients, a femoral derotation, shortening, and varus osteotomy were performed to achieve a neck-shaft angle of about 120–125 degrees and a physiological femoral anteversion of 15 to 25 degrees. We applied a lateral approach. The pelvic osteotomy and, if necessary, the open reduction were performed via a Smith-Petersen approach [21]. The necessity of an open reduction was evaluated with intraoperative arthrography. In the case of a medial pooling an open reduction with debridement of the acetabulum was performed. The lateral aspect of the ilium was exposed, and the sciatic nerve was protected by a retractor in the sciatic notch. The modified Dega osteotomy consisted of a monocortical osteotomy of the external cortex around the acetabulum down to the posterior column of the acetabulum stopping before the sciatic notch with a swan neck chisel controlled by the use of an image intensifier. It was accomplished by a short bicortical osteotomy at the level of the anterior inferior iliac spine. The acetabular side of the osteotomy was bent down and hinged caudal to provide maximum hip coverage. The resected bone wedge resulting from the femoral shortening was adjusted and interposed in the osteotomy gap. In all of the patients, a postoperative spica cast was applied for an average duration of 3.3 weeks (SD 0.93; range 1 to 6 weeks), depending on bone quality. After cast removal sitting was allowed as soon as 90 degree of hip flexion was achieved easily. In ambulating patients standing and sitting were allowed after 6 weeks when a first plain hip X-ray image showed callus formation and stable implant fitting. The procedure was described in detail by Brunner and Baumann [22].
Demographics
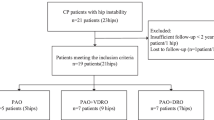
In total, 133 reconstructed hips with closed triradiate cartilage at the time of surgery were retrieved from our database. Overall, 90 hips had to be excluded due to an insufficient follow-up interval (N = 12), other neurologic diseases than cerebral palsy (CP; N = 12) or incomplete chart due to missing radiographs in one of the follow-up periods or missing clinical follow-up data (N = 66). Thus, 43 hips in 37 patients were finally included in the study. Operations were performed between 1989 and 2011 in a single institution. In total, 20 patients were female and 17 male. Mean age at surgery was 15.2 years (SD 2.78; range 9.4–25.1 years), mean follow-up time was 13.4 years (SD 5.7; range 5.1–25.6 years). Table 2 demonstrates the distribution of included hips of each GMFCS level.
Statistics
Since the range of follow-up was long we grouped the follow-up results in findings obtained at 5 year intervals (period A: 1–5 years, period B: 6–10 years, period C: 11–15 years, period D: more than 16 years) to demonstrate the course of the development of OA and MP. Table 3 demonstrates length of follow-up of patients. In each period the radiographs were evaluated concerning the degree of OA and the MP. The ROM was evaluated before surgery and at the last follow-up, and pain was evaluated at last follow-up. The Kolmogorov–Smirnov test was used to check normal distribution of data. For comparison of the Kellgren Lawrence score, the MP, the ROM and sphericity of the femoral head a two-tailed paired t test was used in normally distributed data. In not normally distributed data the Mann–Whitney U test was used. The 95% confidence interval (CI) was calculated additionally. For comparison of pre- and postoperative GMFCS levels the Wilcoxon rank-sum test was applied. Logistic regression was used to calculate correlations. The cutoff for significance was defined as P < 0.05 (Fig. 2).
Results
Osteoarthritis
Mean Kellgren Lawrence score was 0.88 out of 4 (SD 0.59; range 0–3) preoperatively. This was mainly due to the deformity of the femoral head which occurred already in the dislocation process preoperatively. In period A Kellgren Lawrence score increased to 1.50 (SD 0.78; range 0–3), in period B to 1.86 (SD 0.75; range 0–3) and in period C to 2.0 (SD 0.87; range 0–4). In period D it was 1.75 (SD 0.68; range 0–4). Calculating the score at last follow-up of each patient Kellgren Lawrence score was 1.95 out of 4 (SD 0.79; range 0–4). There was a statistically significant difference between the Kellgren Lawrence score obtained preoperatively and at the score obtained at last follow-up (score 1.07 points; CI 0.75–1.39). The difference between the scores in the follow-up period A compared to the last follow-up period D, however, did not differ significantly (score 0.45 points; CI 0.05–0.85) (Fig. 3) (P = 0.232). In 7 of 43 hips an intraarticular fracture of the acetabulum was visible on the postoperative X-ray. Median Kellgren Lawrence score of these 7 hips was 2.0 (SD 0.58; range 1–3).
Migration percentage
Mean MP was 64.76% (SD 23.6; range 15–100%) preoperatively. In follow-up period A it was reduced to 4.63% (SD 7.70%; range 0–30%). We found a stable course over time with a MP of 5.13% (SD 8.12%; range 0–30%) in period B, 6.11% (SD 9.94%; range 0–30%) in period C and 6.88% (SD 9.30%; range 0–30%) in period D. At last follow-up of each patient MP was 5.70% (SD 8.56%; range 0–30%). There was a significant change between preoperative MP and MP in period A (59.1%; CI 52.4–67.8%) (P < 0.00001) but no significant increase of MP between follow-up period A und last follow-up in period D (1.07%; CI − 2.5–4.6%) (Fig. 4) (P = 0.857).
Sharp angle
Mean preoperative Sharp angle was 51.3° (SD 6.3°; range 38–66°), in follow-up period A it reduced to 32.8° (SD 7.3°; range 21–50°), in period B it remained at 32.8° (SD 6.8°; range 21–49°), in period C it stayed at 32.6° (SD 7.0°; range 24–47°) and increased to 33.75° (SD 6.2°; range 23–40°) in period D. There was a significant reduction between preoperatively measured mean Sharp angle and mean Sharp angle observed at first follow-up (18.5°; CI 15.7–21.5°) (P < 0.00001). We noted no significant loss of correction between first and last follow-up (0.1°; CI − 2.9–3.1°) (P = 0.962) (Fig. 5). The maximum deterioration of Sharp angle we observed in one hip was 9 degrees over a period of 10 years.
Summary of the results of each period concerning OA, MP and Sharp angle are presented in Table 4.
Sphericity
In the first postoperative radiograph mean difference of the smallest fitting to the largest fitting circle was 13.14% (SD 10.16%; range 0–40.7%). At last follow-up the difference was 11.95% (SD 5.66%; range 2.1–22.4%). The difference of 1.19% (CI − 3.79–6.22%) was not statistically significant (P = 0.49).
Function
We evaluated the passive sagittal ROM in flexion and extension of the hip joint. The mean maximum flexion of the hip assessed preoperatively was 107° (SD 16.8°; range 70–140°) compared to 96° postoperatively (SD 21.7°; range 30–130°)10.8° (CI 2.2–19.5°) (P = 0.01).
The mean extension deficit decreased from 19° (SD 16.3°; range 0–60°) to 4° (SD 6.4°; range 0–30°) (CI 9.3–20.3°) (P < 0.0001).
Sagittal ROM of the hip joint was 91° (SD 24.3°; range 40–120°) preoperatively, and 92° (SD 22.2°; range 30–120°) postoperatively, resulting in an increase of ROM of 1° (CI − 9.4–11.9°). Although flexion decreased there was no significant change in the ROM since the extension deficit decreased (P = 0.82).
In 3 of 43 (7%) hips pain was a problem at last follow-up. One of the patients suffering from hip pain underwent arthroplasty 12.4 years after the hip reconstruction, which solved the pain problem. In the other two patients, pain was only mild and did not affect daily life. Of the 7 hips with a visible postoperative intraarticular acetabular fracture only one suffered from pain. The patient who underwent arthroplasty had no visible fracture of the acetabulum on plain radiograph. In total, 4 patients deteriorated in GMFCS level, whereas 7 improved.
Discussion
The modified Dega osteotomy has become a standard procedure in patients with neurologic hip dislocation. It reliably produces good results in patients with an open triradiate cartilage [10]. Our study showed that Dega osteotomy applied after the closure of the triradiate cartilage still resulted in stable and in most cases pain-free hips at the long run.
Average Kellgren Lawrence score preoperatively was 0.86, mainly due to femoral head deformity. After surgery the degree of OA increased slowly, ending up at a stable value at follow-up of 10–15 years and more. To the best of our knowledge, OA was never assessed in patients after hip reconstruction performed after physeal closure of the triradiate cartilage. The impact of hip OA on quality of life in patients with neurologic movement disorders is not known. The risk of hip dislocation rises with increasing GMFCS levels and decreased functionality. Our thesis is that especially in non-ambulatory patients with neurologic hip dislocation the acetabular bone may be flexible enough due to osteoporosis caused by inactivity to allow bending of the cortical bone even after closure of the triradiate cartilage similar as in children. Most of the patients needing hip reconstruction thus have limited ambulatory capacity which might result in a lower load on the hip joints making radiological OA clinically less important than in a normal developing population with higher functional demands. As an example, in one tetraplegic patient (GMFCS level IV) a hip reconstruction was performed on the right side only, whereas on the left, also subluxated side, the patient refused surgery. 16.5 years later the reconstructed hip was free of pain despite signs of OA but good function while on the opposite side with less signs of OA an arthroplasty was necessary due to immobilizing pain (for radiographs of this patient see Fig. 6).
In our patients, an intraarticular fracture of the acetabulum visible on plain radiograph seemed to increase the severity of OA but not the intensity and frequency of pain. It was of low relevance for the clinical outcome. We are aware that most of our patients were not able to communicate and the presence of pain could only be estimated and reported by caregivers. Nevertheless, the pain was not an obvious problem for these patients in daily life. Due to the difficult evaluation of the pain we abandoned to use any kind of measurement scale to grade pain intensity, but considered only presence or absence of pain. Inan et al. reported in a mid-term follow-up investigation (mean follow-up of 3.3 years) 78% painless hips after hip reconstruction performed after closure of the triradiate physis [23]. Miller et al. reported 82% painless hips after a mean follow-up interval of 33 months in children who were operated before the closure of the triradiate physis [24]. Our result with 93.0% pain-free hips after a mean follow-up interval of 13.4 years compares well to these findings.
MP was stable over many years indicating that re-dislocation was a minor problem in this population. However, we are aware of the low number of patients in our cohort which makes a comparison to patients with a hip reconstruction while the triradiate cartilage is still visible on plain X-ray images unreliable.
Since the triradiate cartilage was closed in all of our patients, we measured the Sharp angle instead of the AC angle which is commonly used in pediatric patients to measure the acetabular coverage of the femoral head. Sharp angle was stable postoperatively in physiological ranges. Only one patient showed a deterioration of more than 3 degree between the first and last follow-up, thus we conclude that with this surgical technique a stable Sharp angle can be achieved even if the triradiate physis is no longer visible on plain X-ray images at the time of hip reconstruction.
We are aware that the measurement of the sphericity of the femoral head on plain radiographs is of limited value because we obtained images in a single plane and not three dimensionally. In the 1980s and 1990s a preoperative CT scan with 3D reconstruction which is established as a standard nowadays was not available in most patients. We also did not perform CT scans postoperatively on a regular basis to limit exposure to radiation, because at this time no low-dose CT scans were available. Since femoral anteversion and valgus were changed with surgery we decided to compare the first postoperative plain hip X-ray image to the last available radiographic image of the hip since the contour of the femoral head in plain radiographs might change with the change of the femoral geometry. Mean deviation of the two measured circles was not different, nevertheless the standard deviation and the range differed. Preoperatively the standard deviation and the maximum amount of deviation was higher, indicating that preoperatively the femoral head was either in a quite round shape or very deformed while postoperatively the shape was adapted better to the shape of the acetabulum. However, our results indicate that a major reshaping of the femoral head after relocation can not be expected.
The passive sagittal ROM of the hip joint did not change significantly between the preoperative functional state to the values obtained at last follow-up. The preoperative extension deficit decreased while maximum flexion decreased also. Since mean flexion was still more than 90 degrees at last follow-up this decrease was without functional importance. Sitting in a wheelchair was still possible while lying in supine position in bed was achieved easier due to the decreased hip extension deficit. Besides the sagittal ROM the range of abduction of the hip was of importance in patients suffering from cerebral palsy.
Unfortunately, since our data were not collected in a prospective way, we were unable to provide ROM measurements of abduction which represents a limitation of this study.
In about 50% of our patients, a Mustard iliopsoas transfer [25] was performed. We gave up this procedure during the study period due to increased risk for posterior re-dislocation of the femoral head. The procedure, however, did not influence OA or MP. A possible explanation for the unchanged MP is the posterior direction of re-dislocation which is poorly depicted by the MP.
Study limitations
Our study was underpowered hindering us to conduct in depth statistical analyses. This was a retrospective study, only [26,27,28].
For calculation of possible confounders which might influence the development of OA or an increased MP the number of included patients was too small to get meaningful results.
Most of our patients were not able to communicate and the presence of pain could only be estimated and reported by caregivers.
The MP only addresses the laterally directed component of the dislocation and thus may underestimate the number of re-dislocations especially in the Mustard patients. The surgical technique has changed in the last 30 years, with angular stable implants instead of blade plates the need of postoperative casting has decreased. Also, the number of open reductions decreased since the hip subluxation or luxation is detected earlier nowadays due to more awareness and patients with closed physis are operated less often. So we do not know if the results can be transferred to today’s patients.
Intraarticular fractures may be difficult to detect if they are not displaced, and in a plane parallel to the film. Thus, the number may be higher.
The number of the excluded patients is high but resulted from the requirements for a long follow-up period and loss of follow-up and data. This might compromise our results. The ROM was evaluated before surgery and at last follow-up, and pain was evaluated at the last follow-up, only. One plane ROM was evaluated, there were no control group e.g. in children with other hip condictions.
Strength of study
We were able to follow 37 patients over more than 13 years, and present results which had not been described in the literature until now.
Conclusion
In spite of the risk of an intraarticular fracture of the acetabulum with later osteoarthritis of the hip joint, hip reconstruction in patients suffering from neurogenic hip displacement performed after fusion of the triradiate cartilage is a valuable option to achieve stable and pain-free hips for many years in the majority of patients.
Abbreviations
- CP:
-
Cerebral palsy
- GMFCS:
-
Gross Motor Function Classification System
- OA:
-
Osteoarthritis
- MP:
-
Reimers migration percentage
- ROM:
-
Range of motion
References
Kolman SE, Ruzbarsky JJ, Spiegel DA, Baldwin KD (2016) Salvage options in the cerebral palsy hip: a systematic review. J Pediatr Orthop 36(6):645–650. https://doi.org/10.1097/BPO.0000000000000501 (PMID: 25887836)
Hwang JH, Varte L, Kim HW, Lee DH, Park H (2016) Salvage procedures for the painful chronically dislocated hip in cerebral palsy. Bone Joint J 98-B(1):137–143. https://doi.org/10.1302/0301-620X.98B1.35202 (PMID: 26733527)
Houdek MT, Watts CD, Wyles CC, Trousdale RT, Milbrandt TA, Taunton MJ (2017) Total hip arthroplasty in patients with cerebral palsy: a cohort study matched to patients with osteoarthritis. J Bone Joint Surg Am 99(6):488–493. https://doi.org/10.2106/JBJS.16.00528 (PMID: 28291181)
Strauss D, Brooks J, Rosenbloom L, Shavelle R (2008) Life expectancy in cerebral palsy: an update. Dev Med Child Neurol 50(7):487–493. https://doi.org/10.1111/j.1469-8749.2008.03000.x (PMID: 18611196)
Brooks JC, Strauss DJ, Shavelle RM, Tran LM, Rosenbloom L, Wu YW (2014) Recent trends in cerebral palsy survival. Part I: period and cohort effects. Dev Med Child Neurol 56(11):1059–1064. https://doi.org/10.1111/dmcn.12520 (Epub 2014 Jun 26. PMID: 24966011)
Brooks JC, Strauss DJ, Shavelle RM, Tran LM, Rosenbloom L, Wu YW (2014) Recent trends in cerebral palsy survival. Part II: individual survival prognosis. Dev Med Child Neurol 56(11):1065–1071. https://doi.org/10.1111/dmcn.12519 (Epub 2014 Jul 12. PMID: 25041081)
Dega W (1974) Osteotomia trans-iliakalna w leczeniu wrodzonej dysplazji biodra [transiliac osteotomy in the treatment of congenital hip dysplasia]. Chir Narzadow Ruchu Ortop Pol 39(5):601–613 (Polish. PMID: 4422569)
Pemberton PA (1965) Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg Am 47:65–86 (PMID: 14256975)
Mubarak SJ, Valencia FG, Wenger DR (1992) One-stage correction of the spastic dislocated hip. Use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg Am 74(9):1347–1357 (PMID: 1429790)
Rutz E, Vavken P, Camathias C, Haase C, Jünemann S, Brunner R (2015) Long-term results and outcome predictors in one-stage hip reconstruction in children with cerebral palsy. J Bone Joint Surg Am 97(6):500–506. https://doi.org/10.2106/JBJS.N.00676 (PMID: 25788307)
McNerney NP, Mubarak SJ, Wenger DR (2000) One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop 20(1):93–103 (PMID: 10641697)
Reichel H, Hein W (1996) Dega acetabuloplasty combined with intertrochanteric osteotomies. Clin Orthop Relat Res 323:234–242. https://doi.org/10.1097/00003086-199602000-00032 (PMID: 8625586)
Grudziak JS, Ward WT (2001) Dega osteotomy for the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am 83(6):845–854. https://doi.org/10.2106/00004623-200106000-00005 (PMID: 11407792)
Robb JE, Brunner R (2006) A Dega-type osteotomy after closure of the triradiate cartilage in non-walking patients with severe cerebral palsy. J Bone Joint Surg Br 88(7):933–937. https://doi.org/10.1302/0301-620X.88B7.17506 (PMID: 16798999)
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502. https://doi.org/10.1136/ard.16.4.494.PMID:13498604 (PMCID:PMC1006995)
Reimers J (1979) Stabiliteten af børns hofteled bedømt ved ét røntgenfoto [stability of the hip-joint in children assessed by X-ray photograph]. Ugeskr Laeger 141(4):231–233 (Danish. PMID: 760297)
Sharp IK (1961) Acetabular dysplasia. J Bone Joint Surg Br 43-B(2):268–272
Agus H, Biçimoglu A, Omeroglu H, Tümer Y (2002) How should the acetabular angle of sharp be measured on a pelvic radiograph? J Pediatr Orthop 22(2):228–231 (PMID: 11856937)
Clarkson M (2000) The hip. Chapter 6 in musculoskeletal assessment: joint range of motion and manual muscle strength, 3rd edn. Williams and Wilkins, Philadelphia, Lippincott
Farrell G, McGrath F, Hogan B, Logan M, Denvir K, O’Connell B, Irwin E, Gissane C, Wilson F (2016) 95% prevalence of abnormality on hip MRI in elite academy level rugby union: a clinical and imaging study of hip disorders. J Sci Med Sport 19(11):893–897. https://doi.org/10.1016/j.jsams.2016.01.005 (Epub 2016 Feb 8 PMID: 26897392)
Smith-Petersen MN (1949) Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am 31A(1):40–46 (PMID: 18122877)
Brunner R, Baumann JU (2000) Open reduction of hip dislocation in children with cerebral palsy. Orthop Traumatol 8(1):22–36
Inan M, Gabos PG, Domzalski M, Miller F, Dabney KW (2007) Incomplete transiliac osteotomy in skeletally mature adolescents with cerebral palsy. Clin Orthop Relat Res 462:169–174. https://doi.org/10.1097/BLO.0b013e318124fdca (PMID: 17563700)
Miller F, Girardi H, Lipton G, Ponzio R, Klaumann M, Dabney KW (1997) Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop 17(5):592–602. https://doi.org/10.1097/00004694-199709000-00005 (PMID: 9591996)
Mustard WT (1952) Iliopsoas transfer for weakness of the hip abductors; a preliminary report. J Bone Joint Surg Am 24 A(3):647–650 (PMID: 14946216)
Visscher R, Hasler N, Freslier M, Singh NB, Taylor WR, Brunner R, Rutz E (2021) Long-term follow-up after multilevel surgery in cerebral palsy. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03797-0 (Online ahead of print)
Tomaszewski R, Rutz E, Mayr J, Dajka J (2020) Surgical treatment of benign lesions and pathologic fractures of the proximal femur in children. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03687-x (Online ahead of print)
Vogel-Tgetgel ND, Kläusler M, Brunner R, Camathias C, Rutz E (2020) Short-term outcome of double-shelled braces in neuromuscular scoliosis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03600-6 (Online ahead of print)
Hägglund G, Lauge-Pedersen H, Wagner P (2007) Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord 26(8):101. https://doi.org/10.1186/1471-2474-8-101.PMID:17963501;PMCID:PMC2194677
Terjesen T (2012) The natural history of hip development in cerebral palsy. Dev Med Child Neurol 54(10):951–957. https://doi.org/10.1111/j.1469-8749.2012.04385.x (Epub 2012 Aug 13 PMID: 22881288)
Acknowledgements
Dr. Erich Rutz, MD, was supported by the Bob Dickens Fellowship in Pediatric Orthopedics, University of Melbourne, Australia
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Ethical approval was given by the “Ethikkommission Nordwest- und Zentralschweiz” (EKNZ) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schlemmer, T., Brunner, R., Speth, B. et al. Hip reconstruction in closed triradiate cartilage: long-term outcomes in patients with cerebral palsy. Arch Orthop Trauma Surg 142, 3667–3674 (2022). https://doi.org/10.1007/s00402-021-03970-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03970-5