Abstract
Purpose
The purpose of this study was to determine the outcome of unstable type C pelvic fractures treated with posterior stabilisation and the anterior subcutaneous internal fixator (ASIF).
Methods
Altogether, 36 consecutive patients were treated for unstable type C pelvic ring fractures using posterior stabilisation and ASIF. After a minimum of 18 months, the clinical and radiological outcome was retrospectively investigated.
Results
Overall, three patients (8.3 %) died, and 31 patients (86 %) were available for follow-up after a mean of 4.5 years. Thirty of 31 patients (97 %) showed radiographic bone consolidation of both the posterior and anterior pelvic ring. Only one non-union and two infections due to the anterior device were observed. The total German pelvic outcome score showed an excellent or good rating for 64.5 % of the patients, and a fair or poor for 35.5 %. The SF-12 questionnaire showed a significantly reduced total score for physical and mental health compared to a general reference population.
Conclusions
The ASIF represents an innovative surgical procedure for the treatment of type C pelvic ring fractures. In the medium term, patient satisfaction was high and the complication rate was low, despite the small number of patients. More cases must be investigated before the procedure can be recommended in general, possibly replacing the external fixator for the treatment of pelvic ring fractures in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unstable pelvic fractures are often associated with high-energy trauma, most commonly road traffic accidents and falls from heights. Quite often, such patients suffer from polytrauma [1, 2]. As soon as the pelvic ring fracture has been diagnosed (commonly by polytrauma CT), the surgeon must decide on the specific time and type of repair/stabilisation and/or the pelvic surgery technique. Other factors influencing these decisions are the haemodynamic cardiovascular status, a decision additional injuries, and other necessary measures, particularly with regard to brain and abdominal injuries. In patients with a stable cardiovascular status, a decision as to whether so-called “damage control” should be performed as an initial measure or if “early total care” is required, i.e. the definitive care for all injuries.
Today, a wide range of innovative technologies and implants have become available for the surgical stabilisation of the posterior and anterior pelvic ring. In cases of emergency and haemodynamic instability, the pelvic clamp can provide temporary stabilisation [3, 4], while there are different options for the definitive repair of the posterior pelvic ring (depending on fracture morphology), such as lumbopelvic and iliolumbar support using a system of rods and screws [5], a sacroiliac screw connection [6] or sacral screw and plates osteosyntheses in various configurations [7, 8]. Furthermore, the transiliacal internal fixator (TIFI) represents another stable and minimally invasive option [9, 10]. The external fixator still represents the gold standard for anterior transpubic pelvic fractures [11]. A variety of access points at the iliac crest are available for positioning; however, from a biomechanical point of view supraacetabular fixation represents the most stable connection [12]. Today, minimally invasive options have become available for this procedure, e.g. such as transpubic column screws [13] or interjectional reconstruction plates [14]. In our hospital, the anterior subcutaneous internal fixator (ASIF) has been developed for the stabilisation of unilateral and bilateral, transpubic pelvic fractures, and it has been routinely used since 2004. The first report on its technology, application, and on the initial clinical results was published in 2009 [15]. In the meantime, similar or slightly modified publications from other authors have become available [14, 16]. The objective of this retrospective evaluation of cases was the initial collection of mid- to long-term clinical and radiological data.
Patients and methods
General data collection
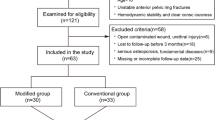
In our hospital, all surgical procedures have been prospectively documented via PC, which allows for the collection of data of specific operations at any time. The inclusion criteria for the initial analysis of this case study included the following: surgery between 1 January 2004 and 31 December 2011 (deadline) and the use of the anterior subcutaneous internal fixator (ASIF) for the management of unstable type C pelvic fractures with transpubic pelvic injuries according to the Tile [17] and AO/OTA classification system. Exclusion criteria were: type A and B pelvic injuries, and type C pelvic injuries with symphysis rupture. These injuries have been routinely stabilised by anterior application of the four-hole LCP reconstruction plates. Other exclusion criteria were: acetabular fractures, injuries of unclear date, insufficiency fractures in elderly patients, and a history of conservatively or surgically treated pelvic injuries. The initial application of an anterior external fixator for “damage control” with subsequent conversion to ASIF was not an exclusion criterion. Based on these inclusion and exclusion criteria, and following an additional evaluation of the diagnostic CT scans, a total of 36 consecutive patients were included. It must be noted that a total of 14 patients who had already been part of the original publication in 2009 [15] have been included in this study, and these were clinically and radiologically followed up once again (with the exception of one patient who had died). Then, the descriptive data for the retrospective study of evidence level 4 such as gender, age, initial Glasgow coma scale (GCS), injury severity score (ISS), blood loss, and potential enhanced measures (such as angioembolisation, surgical procedures), and complications were retrieved from the patient records.
Clinical data collection
In addition to the regular clinical and radiological follow-up, the patients were contacted by telephone and asked to return to the hospital 18 months after surgery. The clinical data collection started with a survey using the standardised and widely accepted SF-12 questionnaire [18], which the patients received and completed at follow-up.
The SF-12 questionnaire is a short form of the SF-36 questionnaire, which is well accepted for the evaluation of the general health-related quality of life and which has sufficient reliability and validity even in the German version [19]. Using weighted indicator variables—that are created based on the item’s response categories—12 items can be calculated to evaluate the total amount of physical and psychic scales. Higher values represent a higher quality of life. The results of 6,662 samples of the general population serve as a reference for the SF-12 [19].
Furthermore, the so-called “Becken outcome score” (pelvic outcome score) was assessed based on clinical investigations, radiological findings, and a patient survey [20]. This score has been developed and published by the pelvic study group of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie [DGU]) and by the “Osteosynthese International” working group. Three points (min. 1 to max. 3 points) are assigned to the radiological findings, and a maximum of 4 points (min. 1 to max. 4 points) to the clinical findings. The “critical value” for the radiological evaluation is a 5-mm residual posterior displacement or a 15-mm anterior displacement in the pelvic ring defining a poor result (1 point). The clinical results included rating of function, neurological, urological, and sexual deficits. This results in a higher ranking of the subjective status in contrast to the radiological findings. The maximum of 7 represents an excellent result, 6 = good, 5 and 4 points = moderate, 3 or 2 points represent a poor outcome.
Finally, the questionnaire is used to independently assess social reintegration. Three points as a maximum score stands for an unchanged functionality with regard to sports and working, two points represent impairment, and one point stands for trauma-induced withdrawal from sports and working.
The imaging for follow-up purposes included conventional pelvic X-ray, and—if consolidation was unclear—so-called inlet and outlet scans were performed. The evaluation was performed by the primary and secondary author in accordance with the radiological criteria of the so-called “Becken outcome score” (pelvic outcome score) [20].
Surgical technique
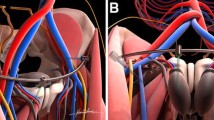
Over the last few years, we have slightly modified and simplified the surgical technique when compared to the original publication [15]. The screws are now directly inserted in a supra-acetabular position, and the single tie rod (with a diameter of 6 mm) is positioned at a slightly larger distance from both parts of the pelvic bone (Fig. 1). However, we still primarily use so-called polyaxial USS pedicle screws (Synthes Spine, Paoli, PA) with a size of 6- or 7-mm diameter and a length of 50–60 mm. The surgical stabilisation of the pelvic ring fracture has principally been performed through a posterior approach: in 20 cases with an open spinopelvic and iliolumbar support using a system of rods and screws, in 12 cases with an iliosacral screw osteosynthesis, in three cases with a plate osteosynthesis (ilium fracture) and in one case with a transiliac internal fixator (TIFI). ASIF placement was performed in a one-stage (31 patients) or two-stage procedure (five patients) with regard to posterior pelvic stabilisation.
Statistics
Statistical analyses have been performed using SPSS for Windows, version 20.0 (SPSS Inc; USA). The normal distribution of metric variables was assessed using Shapiro-Wilks tests. When comparing two independent samples of normal distribution, the t-test was used, and when comparing two independent samples of abnormal distribution, the Mann–Whitney U test was used. Correlation between two parameters has been calculated using the correlation coefficient according to Spearman-Roe. A bilateral significance evaluation was performed for all tests, for which a p-value of < 0.05 was considered statistically significant.
Results
Patient characteristics
Descriptive data collection for 22 male and 14 female patients showed a mean age of 45.2 years ± 3.29 SD (range 17–95 years) at the time of surgery. The predominant mechanism of injury was a high energy trauma from a motorcycle crash (16 cases) and a fall from heights (11 cases). No one had gunshot wounds and no one had an open pelvic fracture.
Injury severity resulted in a mean ISS of 25.17 points ± 1.72 SD; mean GCS was 13.6 points. A total of 14/36 patients (38.9 %) were intubated immediately at the accident site or secondarily in the emergency trauma room at the latest.
Overall, 9/36 patients (25 %) were unstable in the emergency trauma room, requiring mass transfusion (more than ten units of red blood cell packs) and 18/36 patients (50 %) received more than five blood units within 24 hours. On the other hand, no one required angioembolisation for the control of bleeding.
Preoperative CT scans—which were performed in all cases—showed a posterior unilateral and complete sacral injury in 25/36 cases (type C1.3 injury), and an additional contralateral incomplete sacral injury in two cases (type C2), and a complete bilateral sacral disruption in seven cases (type C3.3). There was one case each of a C1.1 and C3.2 injury according to the Tile classification [17]. In 16/36 patients (44.4 %) the anterior pelvic ring showed a unilateral and otherwise bilateral transpubic and complete pelvic ring damage.
In 21/36 cases (58.3 %) the stabilisation of the pelvic ring was carried out primarily within 24 hours following trauma, and secondarily in all other cases within a period of 18 days.
No complications were documented with regard to ASIF application; in particular, no intra-abdominal injuries have been observed in relation to the subcutaneous insertion of the horizontal rod, and no misplacement requiring intervention of the 36 pairs of screws. Intraoperative conversion to another procedure was not required in any of the cases. Subsequent radiological follow-up showed no cases of implant failure, such as breakage of the horizontal connections or loosening of the connectors between the rods, screws, and connecting clamps.
No patient died intraoperatively or within 48 hours due to volume-depletion shock. However, 3/36 patients (8.3 %) died on the fourth, eighth and 41st day postoperatively. Multi-organ failure was the cause of death in all of the three cases, and there was no case of death induced by volume depletion.
The total infection rate for the ASIF was 5.6 % (2/36 patients). During the postoperative follow-up, one female patient had an infection at the entry side of both screws, which required complete premature removal of the fixator on day 27. After that, Escherichia coli was detected and the infection healed completely. In another patient, Staphylococcus aureus was detected and surgical revision (including irrigation at the entry site of the screw) and additional antibiotic treatment was administered, resulting in healing with the fixator in situ.
At follow up, the ASIF was removed in 30 patients after a mean period of 9.4 months (range 27 days to 40.2 months) postoperatively (three patients died, three patients have had no implant removal to date). No complications have been documented in association with the elective implant removal. This procedure was performed in combination with other surgical measures (such as additional implant removal, primarily of the posterior implants) in 22/30 patients (73.3 %).
Mean hospital stay was 26.6 days ± 3.37 SD (range 10–97 days), including a mean period of intensive care treatment of 8.56 days ± 1.59 SD (range 0–41 days).
It was finally possible to follow up 31 of 36 patients (86.1 %; three deceased, two addresses unknown) over a mean period of 53.48 months ± 5.1 SD (range 18–101 months) clinically and radiologically.
Radiological outcome
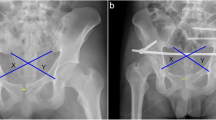
Overall, 30/31 patients (96.8 %) showed radiologically confirmed consolidation of the pelvic fracture. There was only one female patient who showed non-union malalignment in both the posterior and anterior pelvic region, representing the worst in this study (Figs. 2a, b). Postoperative infection and loosening of the posterior iliolumbar instrumentation were observed in this patient in addition to a so-called non-compliance. This patient was a 41-year-old woman with schizophrenia and alcohol abuse, where the pelvic fracture was caused by jumping out the window during a suicide attempt. At the time of follow-up, the patient refused surgical revision. In contrast, Figs. 3a and b show the imaging findings with excellent outcome.
a A 41-year-old female patient. Postoperative radiograph of the pelvis shows posterior stabilisation of a bilateral transforaminal sacral fracture. Stabilisation of the bilateral anterior pelvic ring fracture was performed by anterior subcutaneous internal fixator (ASIF). b Same patient as Fig. 2a. Radiograph of the pelvis 41 months postoperatively. Worst case in this series with non-union and pelvic displacement after infection
a A 58-year-old female patient. Postoperative radiograph of the pelvis shows posterior stabilisation of a transforaminal sacral fracture on the right side with screws, and the bilateral complete anterior pelvic ring fracture treated with anterior subcutaneous internal fixator (ASIF). b Same patient as Fig. 3a. Radiological outcome 21 months postoperatively. Excellent outcome in this series
At the time of follow-up (58, 33, and 18 months postoperatively), the ASIF was still in situ in three patients without showing any radiological signs of implant loosening (Fig. 4) and without causing any complaints. This is why the patients still refused implant removal. Furthermore, heterotopic ossifications were found in the radiological findings of five patients (bilaterally) and four patients (unilaterally), respectively, at the supra-acetabular entry points. None of these cases was associated with clinical symptoms at the time of follow-up.
Clinical outcome
The SF-12 score showed a total score for physical health of 43.44 ± 1.97 SD and a total score for mental health of 45.80 ± 1.94 SD. The reference values of a normal population for physical and for mental health were 48.22 ± 8.7 SD and 51.41 ± 8.5 SD [19].
In summary, the physical and mental quality of life in the SF-12 score of the 31 patients was significantly worse (p < 0.05) than in the general reference population.
The results of the “Becken outcome score” are shown in Table 1. In this regard, the total score of radiological and clinical findings showed good or very good results in 64.5 % of the cases.
No statistically significant factors influencing the clinical outcome (SF-12 and pelvic score) were detected and the distribution of the possible independent variables and parameters was dichotomous (Table 2).
Furthermore, 15 patients (48.4 %) and 11 patients (35.5 %) reintegrated without and with restrictions, respectively. Five patients (16.1 %) had to withdraw from sports and work following the pelvic fracture.
Moreover, the results of the physical and mental summary measures of the SF-12 were evaluated with regard to their correlation to the German pelvic outcome score. However, only a low correlation (r = 0.479; Pearson or Spearman’s rho) between the physical summary measure and the total pelvic outcome score was found.
Finally, 6/31 patients (19.4 %) reported persistent symptoms from the lateral femoral cutaneous nerve (unilateral in four and bilateral in two cases) at the time of follow-up. Considering the surgical access for the screw placement, it is likely that these symptoms trace back to this. These symptoms were persistent but not significantly physically disturbing and manifested exclusively as hypaesthesia, not as allodynia, hyperpathy, or causalgia.
Discussion
This retrospective study with evidence level 4 is the first to deliver mid- to long-term clinical and radiological results with regard to the surgical treatment of patients with unstable pelvic fractures, who received posterior osteosynthesis and an additional minimally invasive treatment for the stabilisation of transpubic pelvic injuries by ASIF. Therefore, the following discussion mainly takes into account this innovative ASIF procedure and its advantages and disadvantages rather than the management of an unstable pelvic injury itself, in accordance with the Advanced Trauma Life Support guidelines.
At first, it should be noted that our descriptive data (such as age, gender, accident cause, initial GCS and ISS scores) do not show essential differences when compared to other study populations in which the outcome after pelvic fractures has been evaluated [7, 8, 10, 21]. With regard to the technique and application, we would like to refer to our original paper published in 2009 [15], even though we have slightly modified the procedure over the last few years in such a way that the screws are now placed in the supra-acetabular position (Fig. 1), which facilitates the application. In addition, this eliminates the need for intraoperative fluoroscopic guidance (assuming sufficient experience of the surgeon), although we sometimes still use fluoroscopic guidance for didactic reasons.
It must be highlighted that the insertion of both screws and horizontal rod (which requires initial shaping and shortening) and the placement in the patient’s fat tissue is more time-consuming than the application of a supra-acetabular external fixator, which has been the so-called gold standard up to now. Nevertheless the learning curve is steep, and the time from incision to suturing should not be longer than 30–60 minutes. In our study, we did not see any disadvantages in this regard, even in patients with critical and haemodynamic circulatory instability. No patient died from haemorrhagic shock within the first 48 hours, and there were only two referred patients who were treated with an external fixator for this reason. Moreover, this procedure allows for conversion at a later point in time, which we performed in both of these two patients without any complications. Furthermore, recent studies have shown that the level of concomitant injuries (particularly of concomitant cerebral trauma) determines the mortality rate and outcome, rather than the severity of the pelvic injury itself [21, 22].
A total of 8.33 % (3/36) of the patients of our study population died postoperatively due to multiorgan failure. Thus, the mortality rate was almost identical when compared with other publications [21]; on the other hand, none of our patients had open pelvic fractures or gunshot injuries, which are also associated with a significantly high mortality rate [23].
Biomechanical testing of the ASIF (using a fixed human pelvic model) has not been performed so far. Although, biomechanical evaluations of an almost identical rod and screws system at the posterior pelvic ring showed sufficient stability [9] and with regard to our latest clinical data, we see no actual need for this. From a clinical point of view, no fracture of the horizontal rod (titanium alloy; 6-mm diameter) or no loosening of the connection between the rod and the polyaxial screw and sheath, has been detected to date. Moreover, the system has been successfully used in spinal surgery for many years, as well as for the stabilisation of the posterior pelvic ring [10].
Postoperative follow-up and extensive investigations have shown non-union only in one female patient, and radiological and clinical loosening of both anterior screws in another patient (in which infection and loosening of the posterior osteosynthesis were also found). Therefore, we see a clear advantage for the internal procedure when compared to external application with regard to consolidation on the one hand, and the possible non-union rate, on the other. Furthermore, we had only two infections in our population, which supports our point of view and has been substantiated by a recent study [14].
Additionally, it should be mentioned that the subcutaneous and internal application of the horizontal rod implies the risk of damaging abdominal structures, particularly in the presence of existing hernias. Nevertheless, we have not seen any complications (neither fat tissue necrosis requiring revision nor bleeding) in almost ten years of using this technique, even in obese patients.
Surprisingly, heterotopic ossifications were found in the radiological findings of five patients (bilaterally) and four patients (unilaterally) at the supra-acetabular entry points. None of these cases were associated with clinical symptoms up to now. Based on these new discoveries, we have started to prescribe an oral NSAID for two weeks postoperatively. So far, we have no results with regard to a possible reduction of such ossifications due to this measure. Finally, the clinical findings showed that the ASIF has been well accepted by the patients. Premature implant removal on day 27 was required in only one female patient (Fig. 2a, b) due to infection.
The ideal time for ASIF removal has not yet been identified. In our study population, the apparatus was removed after a mean postoperative period of 9.4 months. No complications have been observed in relation to this issue. The ASIF should remain in situ for at least 12 weeks (whenever possible) until bony consolidation is achieved. This is not completely in accordance with other studies, where the external fixator is removed after a period of only a few weeks [20].
We have not observed any disadvantages, particularly no clinical signs of loosening, when the fixator remains in situ for longer periods. In ten patients, the ASIF remained in situ for at least 12 months; in three patients, the implant has remained in situ up to now without causing any symptoms (Fig. 4). Based on this experience, we generally recommend implant removal within an interval between 12 weeks and 12 months, possibly in combination with another procedure such as an additional implant removal, performed as an elective procedure.
As expected, the clinical data of the thorough follow-up of 31 patients (after a mean period of 4.5 years post surgery), including the German pelvic outcome score and SF-12 questionnaire, showed restrictions in quality of life but equivalent or better results when compared to other external and internal osteosynthesis techniques [7, 10, 20, 24]. Nevertheless, these data have less clinical importance, due to the heterogeneity of the study population, the use of different clinical outcome scores and the retrospective analysis. Statistically significant influence factors (Table 2) with regard to the clinical outcome have not been identified, possibly due to the small sample size.
All in all, the ASIF represents an innovative surgical procedure for the treatment of type C pelvic ring fractures. In the medium and long term, patient satisfaction was high and complication rates were low, despite the small number of cases. When compared with the conventional external fixator, the procedure generally requires surgical implant removal; however, this can often be carried out in an elective procedure within another scheduled operation. More cases must be investigated before the procedure can be recommended in general, possibly replacing the external fixator for the treatment of such injuries in the future.
References
Black EA, Lawson CM, Smith S et al (2011) Open pelvic fractures: The University of Tennessee Medical Center At Knoxville experience over ten years. Iowa Orthop J 31:193–198
Davarinos N, Ellanti P, Morris S et al (2012) Epidemiology of pelvic and acetabular trauma in a Dublin tertiary hospital: a 10-year experience. Ir J Med Sci 181:243–246
Grotz MR, Allami MK, Harwood P et al (2005) Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury 36:1–13
Ganz R, Krushell RJ, Jakob RP et al (1991) The antishock pelvic clamp. Clin Orthop 267:71–78
Nothofer W, Thonke N, Neugebauer R (2004) Treatment for unstable sacral fracture in pelvic ring disruptions with dorsal sacrum distantly anchored ORIF (DSDO). Unfallchirurg 107:118–127
Rysavy M, Pavelka T, Khayarin M et al (2010) Iliosacral screw fixation of the unstable pelvic ring injuries. Acta Chir Orthop Traumatol Cech 77:209–214
Kobbe P, Hockertz I, Sellei RM et al (2012) Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop 36:159–164
Suzuki T, Hak DJ, Ziran BH et al (2009) Outcome and complications of posterior transiliac plating for vertically unstable sacral fractures. Injury 40:405–409
Dienstknecht T, Berner A, Lenich A et al (2011) Biomechanical analysis of a transiliac internal fixator. Int Orthop 35:1863–1868
Dienstknecht T, Berner A, Lenich A et al (2011) A minimally invasive stabilizing system for dorsal pelvic ring injuries. Clin Orthop Relat Res 496:3209–3217
Tscherne H, Pohlemann T (1998) Unfallchirurgie. Becken und Acetabulum. Springer-Verlag, Berlin, Heidelberg, New York
Kim WY, Hearn TC, Seleem O et al (1999) Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res 4:237–244
Gänsslen A, Krettek C (2006) Retrograde transpubic screw fixation of transpubic instabilities. Oper Orthop Traumatol 18:330–340
Cole PA, Gauger EM, Anavian J (2012) Anterior pelvic external fixator versus subcutaneous internal fixator in the treatment of anterior ring pelvic fractures. J Orthop Trauma 26:269–277
Kuttner M, Klaiber A, Lorenz T et al (2009) The pelvic subcutaneous cross-over internal fixator. Unfallchirurg 112:661–669
Vaidya R, Colen R, Vigdorchik J et al (2012) Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 26:1–8
Tile M (1996) Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg 4:143–151
Gandek B, Ware JE, Aaronson NK et al (1998) Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 51:1171–1178
Maurischat C, Morfeld M, Kohlmann T, Bullinger M (2004) Lebensqualität. Nützlichkeit und Psychometrie des Health Survey SF-36/SF-12 in der medizinischen Rehabilitation. Pabst Science Publishers, Lengerich
Pohlemann T, Gänsslen A, Schellwald O et al (1996) Outcome evaluation after unstable injuries of the pelvic ring. Unfallchirurg 99:249–259
Lunsjo K, Tadros A, Hauggaard A et al (2007) Associated injuries and not fracture instability predict mortality in pelvic fractures: a prospective study of 100 patients. J Trauma 62:687–691
Parreira JG, Coimbra R, Rasslan S et al (2000) The role of associated injuries on outcome of blunt trauma sustaining pelvic fractures. Injury 31:677–682
Brenneman FD, Katyal D, Boulanger BR et al (1997) Long-term outcomes in open pelvic fractures. J Trauma 42:773–77723
Dienstknecht T, Pfeifer R, Horst K et al (2013) The long-term clinical outcome after pelvic ring injuries. Bone Joint J 95:548–553
Conflict of interest
No outside funding was received in support of this research or in the preparation of this article.
None of the authors has received financial or any other support relevant to the implant used in this study or in this study’s preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Müller, F.J., Stosiek, W., Zellner, M. et al. The anterior subcutaneous internal fixator (ASIF) for unstable pelvic ring fractures. Clinical and radiological mid-term results. International Orthopaedics (SICOT) 37, 2239–2245 (2013). https://doi.org/10.1007/s00264-013-2032-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2032-0