Abstract
Purpose
Sacroiliac screw fixation is the method of choice for the definitive treatment of unstable posterior pelvic-ring injuries; however, this technique is demanding and associated with a high risk of iatrogenic neurovascular damage. This study evaluates whether minimally invasive transiliac locked compression plate stabilisation may be an alternative to sacroiliac screw fixation in unstable posterior pelvic-ring injuries.
Methods
We performed a retrospective analysis of patients with unstable pelvic-ring injuries treated with a transiliac locked compression plate at a level I trauma centre. Outcome evaluation was assessed using the Pelvic Outcome Score and analysis of complications, intraoperative fluoroscopic time, and duration of the surgical procedure.
Results
Twenty-one patients were available for follow-up after an average of 30 months. The main findings were as follows: Overall outcome for the Pelvic Outcome Score was excellent in 47.6% (ten patients), good in 19% (four patients), fair in 28.6% (six patients), and poor in 4.8% (one patient). Average operation time was 101 min and intraoperative fluoroscopic time averaged 74.2 s. No iatrogenic neurovascular injuries were observed.
Conclusion
Minimally invasive transiliac locked compression plate stabilisation may be a good alternative to sacral screw fixation because it is quick, safe and associated with a good functional outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Internal fixation is the method of choice for the definitive treatment of unstable posterior pelvic-ring injuries [5, 10, 12, 24]. Currently, percutaneous screw fixation of the sacroiliac (SI) joint seems to be the most promising method [4, 14, 15, 27]. However, SI screw fixation is demanding, and concerns have been raised regarding iatrogenic injuries to neurovascular structures [7]. Furthermore, a substantial number of patients continue to suffer chronic posterior pelvic pain despite near anatomical reductions [18, 19, 25]. Minimally invasive transiliac plate osteosynthesis may be an alternative to SI screw fixation and appears to be biomechanically comparable [1, 29]. We evaluated outcome, complications and surgical and fluoroscopy time for patients treated with transiliac locked compression plate osteosynthesis for posterior pelvic-ring injuries.
Patients and methods
Setting
This was a retrospective analysis of patients with unstable pelvic-ring injuries treated with a transiliac locked compression plate at a level I trauma centre.
Patients
Patient sex and age, mechanism of trauma, associated injuries, severity of injury according to the Hannover Polytrauma Score (PTS), timing of surgical treatment, duration of the surgical procedure, complications and requirement of hardware removal were evaluated.
Fracture classification
Pelvic fractures in this study were classified according to the Arbeitsgemeinschaft für Osteosynthesefragen (Association for the Study of Internal Fixation)/Orthopaedic Trauma Association (AO/OTA) classification.
Follow up and outcome evaluation
The follow-up for this study was performed after an average of 30 (8–59) months. Outcome evaluation was performed with the Pelvic Outcome Score, which consists of clinical, radiological and social integration (Table 1) [19]. Functional outcome, including pain and neurological, urological and sexual deficits was examined. Pelvic radiographs (anterior–posterior, inlet, outlet) were assessed by an experienced orthopaedic trauma surgeon. The ratings of the radiological and clinical results were assessed as one score on a 7-point scale, where the maximum of 7 points represents an excellent result, 6 points good, 5 and 4 points fair and 3 and 2 points poor. The work and social integration section differentiates between good (3 points), fair (2 points) and poor (1 point) outcome.
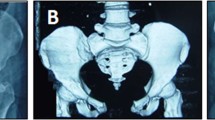
Operative technique and mobilisation
A modified Krappinger technique was used [12]. Briefly, posterior instrumentation of the posterior pelvic ring with transiliac locked plate osteosynthesis was performed with the patient in the prone position. Closed reduction was achieved by traction. Using two short vertical skin incisions above the posterior superior iliac spine, the posterior iliac spine was visualised. A chisel was used to prepare a subfascial tunnel towards the contralateral spine. After bending, the locking compression plate (LCP) was slid into the prepared grooves and through the tunnel and turned axially through 180°. After predrilling, the hole positioned above the iliac crest was fixed with a 4.5-mm cortical screw in each iliac wing (Fig. 1).
Single-shot antibiotic prophylaxis was administered preoperatively, and thromboembolic prophylaxis until full weight bearing was achieved. Partial weight bearing with crutches was allowed immediately after surgery, and full weight bearing was permitted after the sixth postoperative week.
Results
Between September 2002 and August 2006, 23 patients with unstable posterior pelvic injuries (type C) were managed using the technique described above in a level I trauma centre. These included ten women and thirteen men with a mean age of 47.3 (range 18–83) years at the time of injury (Table 2). Six (26%) patients had complex pelvic injuries (two with injuries to the lumbosacral plexus and four with bladder injuries).
Nineteen of the 23 patients (83%) were polytraumatised (average PTS 30 points). Nine patients sustained additional head trauma, 12 experienced chest trauma, five had abdominal injuries and seven had spinal injuries. Twelve patients had concomitant injuries of the lower extremities or acetabular fractures. Mechanisms of injury included motor-vehicle/pedestrian accidents (61%), fall from a height (35%) and crush injuries (4%). According to the AO classification, 17 patients had a C1, five a C2 and one a C3 injury of the pelvic ring. Average length of hospital stay was 31.7 (range 5–104) days, including the patient who was transferred to a long-term respiratory unit after 104 days. Of 23 patients treated by plating, two were lost to follow-up: one died due to multiple organ failure five days after injury and another could not be assessed due to a persistent comatose state at the time of follow-up.
Pelvic outcome score
An excellent clinical result (4 points) was observed in eleven patients (52.4%), a good clinical result (3 points) in four (19%) and a fair result (2 points) in six patients (28.6%). Both patients with injuries to the lumbar plexus showed full neurological recovery. Seventeen patients (81%) demonstrated good radiological outcomes (3 points) and four (19%) showed fair radiological results (2 points). For the overall pelvic outcome score, the combination of clinical and radiological results showed that ten patients (47.6%) achieved the maximum score of 7 points, which reflects an excellent result; four (19%) showed a good result (6 points), six (28.6%) a fair result (4–5 points) and one (4.8%) a poor result (3 points). The patient with the poor outcome was a polytraumatised patient with an initial PTS of 66 points.
Return to work and reintegration
Fifteen of 21 patients (71.4%) returned to their normal activities of daily living, three (14.3%) were limited at work and three (14.3%) were not able to return to work due to their disabilities. The social status was unchanged from the preinjury status in 19 patients (90.5%). One patient complained of minor restrictions and another patient had major restrictions. Thirteen patients (62%) reported no changes in spare time and sports activities; four (19%) had minor and another four (19%) had major restrictions.
Surgical results
Posterior transiliac locked plate osteosynthesis was carried out after an average of 4.9 (range 0–13) days following trauma. Plate length ranged from seven to 11 holes. In six patients, an additional open reduction with local osteosynthesis of a sacral fracture was carried out. Nine patients required additional ventral stabilisation (six symphyseal plates, three intramedullary screws). In ten patients, the external fixator was maintained for multifragmentary anterior fractures. The average operation time was 101 (range 43–255) min for posterior plate osteosynthesis, including additional open sacral reduction if necessary. In cases of additional anterior osteosynthesis, operation time increased to an average of 193 (range 143–272) min. Intraoperative fluoroscopic time averaged 74.2 (range 30–167) s.
Complications
One superficial wound infection required soft tissue debridement with subsequent uneventful healing. One patient developed a deep pelvic vein thrombosis requiring long-term thromboembolic prophylaxis. Three patients required plate removal for minor discomfort after six, 12 and 14 months respectively. Otherwise, we observed no secondary dislocation or implant failure. Other complications reflected the high percentage of severely injured patients in this population. One patient died from multiple organ failure, and one patient was in persistent coma due to a severe head injury. One patient developed acute respiratory distress syndrome (ARDS) and cholecystitis requiring cholecystectomy.
Discussion
Surgical treatment of posterior unstable pelvic-ring injuries is technically challenging. Various methods of internal stabilisation of unstable posterior pelvic-ring injuries have been described [2, 6, 20, 21, 28]. The most widespread procedure is probably SI screw fixation, offering the possibility of percutaneous minimal invasive screw positioning [4, 6, 14, 15, 27]. Although this procedure may be associated with a short operation time and minimal soft tissue dissection, correct screw positioning in the narrow safe zone of the sacrum is difficult. This is due not only to the high anatomical variability of the sacrum, but—in obese patients, in particular—fluoroscopic guidance is difficult and associated with a high risk of sacral nerve damage. Malpositioning of the screw by as little as 4° can cause damage to neurovascular structures [23], which is reported to be as high as 7.7% [7]. Although the incidence of malpositioned SI screws may be reduced by navigated screw insertion, this technique is still associated with misplaced screws in 1.8% of cases [9, 31]. Furthermore, navigation is an expensive tool not available in every clinic, and results strongly correlate with the surgeon’s experience [11]. In view of these difficulties of SI screw fixation, we investigated outcome, complications, and surgical and fluoroscopic time using a minimally invasive transiliac locked compression plate for posterior pelvic-ring instabilities.
In our cohort, 71.4% of patients had an excellent or good functional outcome at follow-up. Similar results were reported by Krappinger et al. after transiliac pelvic stabilisation with a reconstruction plate [12]. This is in line with the functional outcome reported after SI screw fixation. Lindahl and Hirvensalo reported 83% of patients having excellent or good results following SI screw fixation [13], and Cole et al. reported 70.6% of patients with none or only minor functional deficits [5]. As reported by Lindahl and Hirvensalo, post-traumatic pain appeared to be the main driver for the majority of fair results, which accords with our patient population [13]. Critics of SI screw fixation argue that ankylosis of the SI joint may contribute to functional impairment. Although the importance of SI joint ankylosis on functional outcome is not quite certain [16, 30], joint ankylosis can be avoided with posterior plating. Nonetheless, transiliac plate fixation with SI joint sparing in our study was not associated with a better functional outcome compared with SI screw fixation. Thus, joint ankylosis may be of minor importance.
Eighty-one percent of our patients had excellent/good radiological results, 19% showed fair radiological results. Lindahl and Hirvensalo reported excellent/good radiological results in 90% of patients managed with SI screw fixation [13]. Seventy-two percent of our patients returned to their previous work without restrictions, 14.3% were handicapped at work and 14.3% had not returned to work upon follow-up. Nineteen percent felt major restrictions in their free time activity. These results were slightly better than those reported by Tornetta and Matta in a cohort of operatively treated unstable posterior-ring disruptions [24]. Cole et al. reported that 55% of formerly full-time employed patients with unstable posterior-ring injuries managed with SI screw fixation had returned to their previous work without restrictions. Krappinger et al. reported that 39.1% of patients had completely reintegrated [12].
We observed no screw or plate malpositioning and no loss of reduction. This may represent the major advantage of this technique. Transiliac insertion of an LCP results in a low-profile plate that is not technically difficult to insert. Screw placement for plate application is safely located within in the ilium without risk of neurological or vascular compromise. In contrast, SI screw positioning is demanding, and screw malpositioning may be associated with neurovascular injuries and loss of reduction in up to 7.7% of patients [7]. Lindahl and Hirvensalo reported loss of reduction in 6% and screw malpositioning in 2% of patients [13]. According to Routt et al., 8.8% of sacral screw fixations failed [22]. Van Bosch et al. showed that SI screws caused neurological complaints in up to 8% of patients due to screw malpositioning [26]. Krappinger et al. using the same technique as described in this study, also reported no malpositioning of screws or plates; however, they observed a loss of reduction in 8.7% and an implant failure in 13% of their patients [12]. We feel that a locking mechanism of the plate/screws may be helpful in reducing the incidence of secondary displacement.
Percutaneous SI screw fixation is not only advocated as a minimally invasive positioning technique but for short operation times. Lindahl and Hirvensalo report a mean operation time of 98 min for posterior pelvic-ring stabilisation with two SI screws [13]. Similar results were reported by Nork et al. (48 min per screw) and Cole et al. (45 min per screw) [17]. Thus, minimally invasive posterior plating in our series was as quick (average 101 min) as SI screw fixation. Interestingly, our intraoperative fluoroscopic time (average 74.2 s) was lower than reported by Routt et al. and Nork et al., who reported 126 seconds of fluoroscopic time for each SI screw, thus 252 seconds for two SI screws [22].
The value of this study may be limited by its retrospective design, the lack of a control group and the relatively small number of patients. Further, interpretation of the functional outcome in this severely injured patient population may be biased by neurological and other concomitant injuries. Nonetheless, we think that posterior percutaneous plate osteosynthesis may be a good alternative to sacral screw fixation in patients with posterior pelvic-ring instability. It may be of special value for vertically unstable sacral fractures where a high incidence of loss of reduction and iatrogenic nerve injury secondary to fracture compression was found with SI screws [3, 8]. Further, we feel that this technique may be advantageous in osteoporotic bone due to the locking mechanism of the plate/screws.
Conclusion
Our data suggests that plate osteosynthesis may be a safe, quick and stable alternative to SI screw fixation. The low risk of iatrogenic neurovascular injuries and low fluoroscopic time associated with this technique are promising; however, further studies are required to test its use for bilateral posterior instability and osteoporotic bone in which SI screw stability is limited.
References
Albert MJ, Miller ME, MacNaughton M et al (1993) Posterior pelvic fixation using a transiliac 4.5-mm reconstruction plate: a clinical and biomechanical study. J Orthop Trauma 7:226–232
Atlihan D, Bozkurt M, Turanli S et al (2004) Anatomy of the posterior iliac crest as a reference to sacral bar insertion. Clin Orthop Relat Res 141:145
Beaule PE, Antoniades J, Matta JM (2006) Trans-sacral fixation for failed posterior fixation of the pelvic ring. Arch Orthop Trauma Surg 126:49–52
Carlson DA, Scheid DK, Maar DC et al (2000) Safe placement of S1 and S2 iliosacral screws: the "vestibule" concept. J Orthop Trauma 14:264–269
Cole JD, Blum DA, Ansel LJ (1996) Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res 160:179
Comstock CP, van der Meulen MC, Goodman SB (1996) Biomechanical comparison of posterior internal fixation techniques for unstable pelvic fractures. J Orthop Trauma 10:517–522
Giannoudis PV, Tzioupis CC, Pape HC et al (2007) Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br 89:145–154
Griffin DR, Starr AJ, Reinert CM et al (2003) Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma 17:399–405
Grossterlinden L, Rueger J, Catala-Lehnen P et al (2010) Factors influencing the accuracy of iliosacral screw placement in trauma patients. Int Orthop [Epub ahead of print] (doi:10.1007/s00264-010-1092-7)
Keating JF, Werier J, Blachut P et al (1999) Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma 13:107–113
Konrad G, Zwingmann J, Kotter E et al (2010) Variability of the screw position after 3D-navigated sacroiliac screw fixation. Influence of the surgeon's experience with the navigation technique. Unfallchirurg 113:29–35
Krappinger D, Larndorfer R, Struve P et al (2007) Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma 21:595–602
Lindahl J, Hirvensalo E (2005) Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop 76:667–678
Moed BR, Fissel BA, Jasey G (2007) Percutaneous transiliac pelvic fracture fixation: cadaver feasibility study and preliminary clinical results. J Trauma 62:357–364
Moed BR, Geer BL (2006) S2 iliosacral screw fixation for disruptions of the posterior pelvic ring: a report of 49 cases. J Orthop Trauma 20:378–383
Mullis BH, Sagi HC (2008) Minimum 1-year follow-up for patients with vertical shear sacroiliac joint dislocations treated with iliosacral screws: does joint ankylosis or anatomic reduction contribute to functional outcome? J Orthop Trauma 22:293–298
Nork SE, Jones CB, Harding SP et al (2001) Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 15:238–246
Oliver CW, Twaddle B, Agel J et al (1996) Outcome after pelvic ring fractures: evaluation using the medical outcomes short form SF-36. Injury 27:635–641
Pohlemann T, Gansslen A, Schellwald O et al (1996) Outcome after pelvic ring injuries. Injury 27(Suppl 2):B31–B38
Pohlemann T, Gansslen A, Tscherne H (2000) Fracture of the sacrum. Unfallchirurg 103:769–786
Reilly MC, Bono CM, Litkouhi B et al (2003) The effect of sacral fracture malreduction on the safe placement of iliosacral screws. J Orthop Trauma 17:88–94
Routt ML Jr, Simonian PT, Mills WJ (1997) Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma 11:584–589
Templeman D, Schmidt A, Freese J et al (1996) Proximity of iliosacral screws to neurovascular structures after internal fixation. Clin Orthop Relat Res 194:198
Tornetta P III, Matta JM (1996) Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res 186:193
van den Bosch EW, Van der KR, Hogervorst M et al (1999) Functional outcome of internal fixation for pelvic ring fractures. J Trauma 47:365–371
van den Bosch EW, van Zwienen CM, van Vugt AB (2002) Fluoroscopic positioning of sacroiliac screws in 88 patients. J Trauma 53:44–48
van Zwienen CM, van den Bosch EW, Snijders CJ et al (2004) Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma 18:589–595
Vanderschot P, Meuleman C, Lefevre A et al (2001) Trans iliac-sacral-iliac bar stabilisation to treat bilateral lesions of the sacro-iliac joint or sacrum: anatomical considerations and clinical experience. Injury 32:587–592
Yinger K, Scalise J, Olson SA et al (2003) Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma 17:481–487
Yucel N, Lefering R, Tjardes T et al (2004) Is implant removal after percutaneous iliosacral screw fixation of unstable posterior pelvic ring disruptions indicated? Unfallchirurg 107:468–474
Zwingmann J, Konrad G, Mehlhorn AT et al (2010) Percutaneous iliosacral screw insertion: malpositioning and revision rate of screws with regards to application technique (navigated vs. Conventional). J Trauma 69:1501–1506
Authors contributions
TH performed all operations, IH and PK collected and analysed data, HR, TH, RS and PK prepared the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kobbe, P., Hockertz, I., Sellei, R.M. et al. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. International Orthopaedics (SICOT) 36, 159–164 (2012). https://doi.org/10.1007/s00264-011-1279-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1279-6