Abstract
Gastro-duodenal obstruction encompasses a spectrum of benign and malignant disease. Historically, chronic peptic ulcer disease was the main cause of gastro-duodenal obstruction, whereas now malignant cause with gastric carcinomas for gastric obstruction and pancreatic tumors for duodenal obstruction predominate. This paper reviews the role of CT in diagnosing gastro-duodenal obstruction, its level, its cause by identifying intraluminal, parietal, or extrinsic process, and the presence of complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Acute bowel obstruction may be of mechanical origin and result in preventing normal transit of digested intestinal content. The most common sites of obstruction are the small and large bowels, but 1–2% of cases involve gastro-duodenal obstruction. Bowel obstruction accounts for around 25% of patients admitted to surgery for acute abdominal conditions and about 5–7% of all emergency department visits for abdominal pain. Contrary to small and large bowel obstruction in which the role of CT has been extensively discussed in the literature [1, 2], little has been published on CT findings regarding gastro-duodenal obstruction [3, 4]. The goal of this review is to discuss the contribution of MDCT in the diagnosis of acute gastro-duodenal obstruction on the basis of key CT findings. CT may be of value at different steps in the diagnosis of gastro-duodenal obstruction, to:
-
confirm a mechanical obstruction and differentiate it from gastroparesia
-
determine the level of obstruction
-
determine the cause of obstruction
-
look for ischemic findings
Technical considerations for CT imaging in suspicion of gastro-duodenal obstruction
In the absence of contraindications to iodinated contrast material, CT for suspicion of gastro-duodenal obstruction is performed with intravenous opacification at the portal phase. Although it has been recently shown [5] that unenhanced CT could give additional arguments for ischemia complicating small bowel obstruction by showing spontaneous hyperdensity of the bowel wall [5], this potential advantage has not been investigated in gastro-duodenal obstruction. We do not recommend oral contrast in the investigation of bowel obstruction since it may be an issue in a patient who presents nausea and vomiting, or in the elderly with a risk of inhalation.
Positive diagnosis of gastro-duodenal obstruction
Nausea and vomiting are the cardinal symptoms of gastro-duodenal obstruction, also referred to as gastric outlet obstruction. Patients with this condition may not present with epigastric abdominal pain but, when present, this symptom is generally related to an underlying cause.
Plain abdominal X-rays often highlight a dilated gas-filled stomach without any signs of gas distal to the duodenum. These findings may, however, also be noted in patients presenting with gastroparesis, or so-called delayed gastric emptying, whereby food remains in the stomach for an exceptionally long time. Gastroparesis may be associated with several illnesses, such as diabetes, post-viral syndrome, smooth muscle disorders such as amyloidosis and scleroderma, nervous system diseases, or metabolic disorders, or be the result of stomach or vagus nerve surgery, or medication intake, particularly anticholinergics and narcotics. CT imaging can differentiate gastro-duodenal obstruction from gastroparesia when focusing on a lesion at the junction between a dilated and collapsed bowel. By contrast, the identification of a transition zone without any visible lesion does not enable us to rule out or affirm a gastroparesis. Documented delay in gastric emptying is required for the diagnosis of gastroparesis. Scintigraphic gastric emptying of solids is the standard for the evaluation of gastric emptying and the diagnosis of gastroparesis. The most reliable method and parameter for the diagnosis of gastroparesis is gastric retention of solids at 4 h measured by scintigraphy [6, 7].
Diagnosis of the level of obstruction
Gastric outlet obstruction involves complete or incomplete obstruction of the distal stomach, pylorus, or proximal duodenum [4], preventing the passage of gastric contents into the duodenum, whereas more distal duodenal obstructions reach the second, third, or fourth duodenum. Determining the exact transition zone in gastro-duodenal obstruction is essential for diagnosing the obstruction cause, some of which are linked to specific locations. For instance, volvulus affects the distal stomach, peptic ulcer disease stenosis the pylorus or the proximal duodenum, annular pancreas the second duodenum, and superior mesenteric artery syndrome (SMAS) the third duodenum. Conversely, malignant or inflammatory causes of gastro-duodenal obstruction may affect any part of the stomach or duodenum.
Diagnosis of the cause of obstruction
Malignant lesions and peptic ulcer disease are the primary causes of gastro-duodenal obstruction. However, advances in effective peptic ulcer therapy have reduced the incidence of this disease, which was formerly responsible for most gastro-duodenal obstruction cases. Malignancy has thus become the primary cause [3, 4, 8]. In a setting of gastro-duodenal obstruction in patients over 50 years old, a malignant cause must be systematically sought.
As is the case for small and large bowel obstruction [4], systematic evaluation of CT data must also be performed by looking for one of the three major gastro-duodenal obstruction categories: intraluminal, intrinsic, extrinsic, including primary volvulus (Table 1).
Intraluminal causes of gastro-duodenal obstruction
The intraluminal cause of gastro-duodenal obstruction may be a stone, bezoar or, exceptionally, a foreign body or intussuscepted segment of the bowel.
Impaction of a gallstone in the duodenum or stomach via a bilio-enteric fistula may cause gastric outlet obstruction, i.e., Bouveret’s syndrome. CT may show the presence of a bilio-enteric fistula, pneumobilia, and one or several occluding gallstones in the stomach or duodenum [9]. Although such stones are often readily visible on CT, there may be some discrepancy between the diameter of the duodenum and the apparent size of the stone on CT. It is essential to identify air pockets in target areas within the duodenal lumen, as well as the soft tissues surrounding the stone calcifications, or the fat within stones so as to enhance the stone size assessment and to determine the extent to which stones are responsible for the examined duodenal obstruction [9, 10]. Besides Bouveret’s syndrome, a fistula between the gallbladder and the duodenum may lead to a gastro-duodenal obstruction by reactional inflammatory stenosis of the duodenum (Fig. 1).
Duodenal obstruction in a 56-year-old man due to inflammatory stenosis of the duodenum complicating a fistula between the gallbladder and the duodenum. Axial CT image A shows air in the inferior part of the gallbladder (arrow) and the fistula (double arrows) between the gallbladder and the duodenum. Coronal image B shows air in the bile ducts. Axial and coronal CT images show dilatation of the stomach and thickening of the wall of the second portion of the duodenum (arrowhead).
Bezoars may consist of partially digested hair (called trichobezoars), fiber from fruits (particularly persimmons), or vegetables (called phytobezoars), and even hardened blocks of drugs (such as antacids—called pharmacobezoars). They are more common in the stomach, and the small bowel. In a retrospective study of 34 cases of bezoars, only 2 were located in the duodenum [11], and half of this patient group had previously undergone gastric surgery, with gastro-jejunal anastomosis constituting a risk of bezoar obstruction. However, duodenal location is at the risk of gastro-duodenal obstruction. CT may show a focal ovoid or round intraluminal mass with regular margins and heterogenous internal structures with a mottled gas pattern and fatty-content areas.
Foreign bodies are objects swallowed by children or adults, especially mentally challenged adults. These indigestible objects are generally small and pass through the digestive system until they are excreted with stool. However, larger objects may get stuck in the stomach or duodenum and be responsible for a gastro-duodenal obstruction.
Foreign bodies are sometimes swallowed purposely, as when smugglers swallow packets filled with illegal drugs to get through customs. Bowel obstruction may be due to clustering of such packets. In diagnostic imaging of drug trafficking, plain abdominal film (PAF) is the first line investigation. If PAF is normal and drug packing is still suspected, an unenhanced abdomen CT must be performed and it constitutes a fast and accurate modality for the detection of ingested drug-filled packets. Bowel obstruction due to drug-packet ingestion should be carefully considered and promptly treated because of the potentially lethal consequences of transmucosal absorption of the drugs contained in the packets.
Duodenoduodenal intussusception is the most uncommon location of intussusception, probably since masses are seldom detected in the duodenum and this condition is usually due to tumoral lead point, which is more commonly benign (Brunner’s gland hamartoma, papillary adenoma, hyperplastic polyp, carcinoid, duodenal duplication cyst, tubulovillous adenoma) than malignant. In some cases, the lead point may be non-tumoral, e.g., a gastrostomy tube poorly positioned in the duodenum (Fig. 2). Although uncommon, this condition has been well described in the literature [12] and can be evaluated fluoroscopically. CT can readily highlight a collapsed intussusceptum lying within the opacified lumen of the distal intussuscipiens and detect a tumor at the leading point of the intussusceptum. However in some cases, the cause of the intussusception may be difficult to differentiate from the soft-tissue pseudotumor that represents the intussusception itself.
Intrinsic causes of gastro-duodenal obstruction
The intrinsic causes of gastro-duodenal obstruction include parietal causes of obstruction among which cancer predominates, and volvulus.
Parietal causes
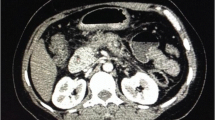
Malignant gastric outlet obstructions primarily occur in the antropyloric area. Advanced gastric neoplasia is the main cause, while metastatic cancer or adjacent malignancies (bile duct cancer, gallbladder cancer) are less common causes [8]. Obstruction may be due to gastric neoplasias, including adenocarcinomas and to a lesser extent carcinoid tumors, whereas lymphomas [13] or gastro-intestinal stromal tumors are seldom responsible for tumoral obstructions [14]. Advanced gastric adenocarcinomas can also be involved in obstruction. These are highlighted on CT as large, segmental, or diffuse areas of wall thickening with irregular lobulation (Fig. 3), often with ulceration. Otherwise they may present as large, polypoid fungating lesions [15].
In contrast to malignant obstructions of the stomach, malignant obstructions of the duodenum are mainly located at the level of the first and second duodenum and mostly due to invasion of the duodenum by a pancreatic cancer, which constitutes the most common cause of malignant gastro-duodenal obstruction. The mechanism of digestive obstruction in pancreatic cancer as well as in gallbladder cancer is twofold: a tumoral invasion of the digestive wall or an extrinsic compression of the digestive lumen. Duodenal obstructions encountered in advanced stages of pancreatic cancer are seldom present at the time of diagnosis, as shown in a study where it was encountered in only 3/76 consecutive patients with pancreatic cancer at the time of diagnosis [16]. Duodenal invasion is not an unresectability criterion, but it is sometimes associated with unresectability criteria such as vascular invasion or liver metastasis, which may be clearly shown by CT.
Exceptionally, some benign tumors may be responsible for bowel obstruction due to compression by the tumor, this rare complication being mainly related to the tumor size (Fig. 4). In peritoneal carcinomatosis, gastric and duodenal invasion may be associated. Gastro-duodenal obstruction was detected in 11 patients (2.5%) screened in a study on gastro-duodenal obstruction imaging features in a series of 438 patients with ovarian cancer. Otherwise 5 cases showed predominant gastric body involvement and 6 presented with gastric outlet and duodenum involvement (Fig. 5) [17].
Duodenal obstruction due to duodenal metastasis in a 56-year-old woman with a stage-4 ovary cancer complicated by peritoneal carcinomatosis. Axial A and coronal B images show thickening of the third portion of the duodenum wall due to serous metastasis from an ovarian cancer. Note also peritoneal carcinomatosis in the greater omentum.
Contrary to cancer, for which invasion of the duodenal wall is generally the obstruction mechanism, the extent of severe pancreatitis may lead to gastro-duodenal obstruction by two different mechanisms: direct damage of the duodenal wall by an inflammatory or a fibrotic reaction or compression by pseudocysts. The mechanism of obstruction may thus be parietal or extrinsic. CT may highlight inflammatory thickening of the wall of the second duodenum associated with signs of acute pancreatitis, which must be highly localized. Paraduodenal pancreatitis is a specific type of focal pancreatitis focused within the pancreaticoduodenal groove and, on CT or MR images combines thickening, infiltration, and cystic structures in the duodenal wall. Although classical, duodenal stenosis with gastro-duodenal obstruction is quite uncommon in clinical practice.
Like acute pancreatitis, cholecystitis can cause inflammatory thickening of the duodenal wall and be responsible for obstruction.
Patients with duodenal obstruction in a chronic pancreatitis setting often have associated pancreatic and biliary duct dilatation. The incidence of obstruction is reported to be about 1% in patients with chronic pancreatitis [18]. The increased risk of pancreatic cancer in patients with chronic pancreatitis ranged from 14.4 to 26.7-fold in a 10-year follow-up study [19], and differential diagnosis between cancer and pseudotumoral forms of chronic pancreatitis, which account for about 20% of chronic pancreatitis cases, is very difficult. Hence, cancer should be suspected when there is a change in the clinical symptomatology and detected signs of gastro-duodenal obstruction in patients with chronic pancreatitis (Fig. 6).
Duodenal obstruction in a 52-year-old man with known chronic pancreatitis. Axial A and sagittal B images show findings of chronic pancreatitis with parietal infiltration of the first and second duodenal wall (arrow). Pancreaticoduodenectomy revealed a cancer of the head of the pancreas with tumoral extension to the duodenal wall.
Gastro-duodenal obstruction secondary to peptic ulcer disease has shown a significant decline in incidence since the discovery of Helicobacter pylori and proton pump inhibitors, and this disorder accounts for approximately 2% of ulcer-related complications [20]. In 80% of cases, the obstruction is due to a duodenal ulcer, with outlet obstruction due to a gastric ulcer being very uncommon. Differential diagnosis between obstruction related to peptic ulcer disease and gastroparesis may be complicated when the stenosis is short and thus hard to identify on CT. In some cases, CT reveals a direct ulcer finding with a focal defect in the duodenal wall enhancement (Fig. 7).
Gastric outlet obstruction is seldom caused by gastritis despite the high prevalence of this disease. Thickened gastric folds and wall thickening with soft-tissue attenuation may be noted on CT. Gastro-duodenal obstruction is regularly caused by eosinophilic gastroenteritis, often with gastric, duodenal, and esophageal involvement [21]. The site of obstruction is often the second or third duodenum, with duodenal wall thickening.
Severe gastritis may be due to corrosive substance ingestion, causing fibrous scarring and leading to antral narrowing and in turn gastric outlet obstruction.
Duodenal Crohn’s disease is rare, with an estimated incidence of 1% to 2% among Crohn’s disease patients. When present, about 60% of patients have continuous disease that involves the antrum, pylorus, and proximal duodenum [22].
Intramural hematomas essentially affect the second and third part of the duodenum. Predisposing factors include blunt trauma, anticoagulant therapy, Henoch–Schonlein purpura, and blood dyscrasias. These entities usually occur during childhood in a traumatic context, such as bike falls with direct abdominal trauma on handlebars or child abuse (by epigastric direct blow). CT spontaneously shows hyperdense wall thickening of the second and third part of the duodenum responsible for a gastric dilatation (Fig. 8). Intramural hematomas are usually managed conservatively although a surgical intervention may be needed in the case of an associated perforation or ischemia.
Duodenal obstruction due post-traumatic hematoma of the second portion of the duodenum in a 20-year-old man. Coronal images before (A) and after (B) intravenous contrast show dilatation of the stomach and spontaneous hyperdense thickening of the duodenal wall. The duodenal lumen (arrow) is better seen after contrast.
With the advent of surgery for morbid obesity, post-operative stenosis has become one of the most common causes of gastric obstruction. The reported incidence of obstruction is as high as 4% [23]. Obstruction may occur at several locations and be due to several mechanisms, depending on the type of surgical procedure. In gastric bypass, potential sites of obstruction include gastrojejunostomy or jejunojejunostomy sites, the mesocolic window and behind the Roux limb (Peterson’s space). In an early post-operative setting, obstruction could result from iatrogenic stenosis secondary to overzealous suturing, but is often due to severe but spontaneously resolving edema. In the late post-operative setting, obstruction may result from internal hernias, adhesions or, in cases of a gastro-duodenal obstruction, may be the consequence of stricture located at the gastro-jejunal anastomosis. The stenosis is better diagnosed by contrast fluoroscopy study than by CT [24]. In sleeve gastrectomy, stenosis is quite uncommon and occurs at the distal part of the gastric tube. In adjustable gastric banding, obstruction may result from a too tight band or from a distal band slippage with the band surrounding the lower gastric fundus body or even antrum. Abdominal plain film, scout of CT image or coronal reformatting may show an abnormal position of the band which is located more inferiorly than usual and has a transverse orientation [25] (Fig. 9).
Volvulus
Volvulus seldom occurs in the stomach. Acute gastric volvulus is typically noted in an acute clinical setting, in patients presenting with sudden intense epigastric pain and vomiting, followed by retching without the ability to vomit, and the inability to pass a nasogastric tube in the stomach. Three categories of volvulus are defined according to their axes of rotation. In the organoaxial form, the stomach rotates along its long axis and is often associated with paraesophageal and diaphragmatic hernia. In the mesenteroaxial form, the stomach rotates along its short axis, with subsequent displacement of the antrum at or above the gastroesophageal junction [26]. The third and most uncommon form of gastric volvulus associates rotation in both the organoaxial and mesenteroaxial planes. A recent study [27] has shown that an antropyloric transition point without any abnormality at the transition zone with the location of the antrum at the same level or higher than the fundus (Fig. 10) had a high sensitivity for diagnosing gastric volvulus and that the presence of both findings had 100% sensitivity and specificity for this diagnosis.
Organoaxial gastric volvulus in a 75-year-old woman. Coronal slice at the arterial phase on the thorax (A) and at the portal phase on the abdomen B show a paraesophageal hernia, the fundus (star) at a lower level than the antrum and the antropyloric transition zone (arrow) at the distal part of the antrum without any mass or bowel thickening.
Extrinsic causes of gastro-duodenal obstruction
Annular pancreas—an uncommon congenital abnormality—is usually asymptomatic, but may cause pancreatitis or duodenal obstruction. Clinical findings of gastro-duodenal obstruction were found to be present in 21% of the 42 patients with annular pancreas included in a retrospective study [28]. An incomplete or complete annular pancreas may be associated with gastric outlet obstruction. When pancreatic tissue is found posterolateral to the second duodenum, it has high sensitivity and specificity for the diagnosis of annular pancreas, whereas the presence of pancreatic tissue anterolateral to the duodenum is significantly less specific. A complete ring of pancreatic tissue surrounding the second part of the duodenum diagnoses a complete annular pancreas, whereas a crocodile jaw appearance of pancreatic tissue anterior and posterior to the duodenum is highly suggestive of incomplete annular pancreas [29]. MRI is superior to CT in showing the annular duct or identifying associated pancreatic abnormalities such as pancreas divisum [28].
SMAS involves superior mesenteric artery compression of the third duodenum. It is responsible for subacute or recurrent forms of obstruction, with a typical relief of obstruction in a prone, knee–chest, or left lateral decubitus position. CT shows dilatation of the stomach and of the first and second duodenum, with a decrease in the superior mesenteric artery–aorta distance and angle [29]. An aortomesenteric distance <8 mm and an angle <22° would be suggestive of this disorder. However, caution is needed when using these measurements as diagnostic cut-off because the superior mesenteric artery is often anterolateral relative to the aorta, and 3D reconstructions provide more accurate assessment than sagittal reformatting. The presence of a Nutcracker phenomenon consecutive to compression of the left renal vein is an ancillary finding for diagnosing SMAS. Moreover, fluoroscopic upper gastro-intestinal imaging may provide additional arguments by showing that the obstruction of the duodenum is relieved by a change in position, especially in left lateral decubitus. Ultimately, it should be kept in mind that CT can be suggestive of the disorder but, even when CT findings are present it must be interpreted in the context of the patient’s symptoms, given the rarity of the disorder [30].
Diagnosis of complication
Gastro-duodenal obstruction complications generally depend on the cause of the obstruction rather than being associated with stomach dilatation. In gastric volvulus, there is a high risk of gastric ischemia and perforation along with peritonitis or mediastinitis if patients diagnosed with this disorder are not operated promptly. In cases of gastric dilatation, gastric or portal pneumatosis may be identified but it is not specific to ischemia. These findings may be noted in patients presenting with gastroparesis due to gastric dilatation, but the symptoms generally resolve when a nasogastric tube is inserted in the stomach [4]. By contrast, the presence of fat stranding or of fluid in contact with the stomach constitutes arguments for ischemia in the setting of gastric pneumatosis.
References
Herlinger H, Rubesin SE (1994) Obstruction. In: Gore RM, Levine MS, Laufer I (eds) Textbook of gastrointestinal radiology. Philadelphia: Saunders, pp 931–966
Mullan CP, Siewert B, Eisenberg RL (2012) Small bowel obstruction. AJR Am J Roentgenol 198:105–117
Jaka H, Mchembe MD, Rambau PF, Chalya PL (2013) Gastric outlet obstruction at Bugando Medical centre in northwestern Tanzania: a prospective review of 184 cases. BMC Surg 13:41
Taourel P, Hoa D, Bruel JM (2011) Bowel obstruction. In: Taourel P (ed) CT of the acute abdomen. Berlin: Springer, pp 273–308
Geffroy Y, Boulay-Coletta I, Jullès MC, et al. (2014) Increased unenhanced bowel-wall attenuation at multidetector CT is highly specific of ischemia complicating small-bowel obstruction. Radiology 270:159–167
Camilleri M, Parkman HP, Shafi MA, et al. (2013) Clinical guideline: management of gastroparesis. Am J Gastroenterol 108:18–37 (quiz 38)
Abell TL, Camilleri M, Donohoe K, et al. (2008) Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol 103:753–763
Park KB, Do YS, Kang WK, et al. (2001) Malignant obstruction of gastric outlet and duodenum: palliation with flexible covered metallic stents. Radiology 219:679–683
Brennan GB, Rosenberg RD, Arora S (2004) Bouveret syndrome. Radiographics 24:1171–1175
Gan S, Roy-Choudhury S, Agrawal S, et al. (2008) More than meets the eye: subtle but important CT findings in Bouveret’s syndrome. AJR Am J Roentgenol 191:182–185
Erzurumlu K, Malazgirt Z, Bektas A, et al. (2005) Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol 11:1813–1817
Otjen JP, Iyer RS, Phillips GS (2012) Usual and unusual causes of pediatric gastric outlet obstruction. Pediatr Radiol 42:728–737
Buyn JH, Ha HK, Kim AY, et al. (2003) CT findings in peripheral T-cell lymphoma involving the gastrointestinal tract. Radiology 227:59–67
Sandrasegaran K, Rajesh A, Rushing DA, et al. (2005) Gastrointestinal stromal tumors: CT and MRI findings. Eur Radiol 15:1407–1414
Ba-Salamah A, Prokop M, Uffmann M, et al. (2003) Dedicated multidetector CT of the stomach: spectrum of diseases. Radiographics 23:625–644
Valls C, Andía E, Sanchez A, et al. (2002) Dual-phase helical CT of pancreatic adenocarcinoma: assessment of resectability before surgery. AJR Am J Roentgenol 178:821–826
Spencer JA, Crosse BA, Mannion RA, et al. (2000) Gastroduodenal obstruction from ovarian cancer: imaging features and clinical outcome. Clin Radiol 55:264–272
Vijungco JD, Prinz RA (2003) Management of biliary and duodenal complications of chronic pancreatitis. World J Surg 27:1258–1270
Tellez-Avila FI, Villalobos-Garita A, Giovannini M, et al. (2014) Follow-up of patients with pseudotumoral chronic pancreatitis: outcome and surveillance. World J Gastreoenterol 20:8612–8616
Appasani S, Kochhar S, Nagi B, Gupta V, Kochhar R (2011) Benign gastric outlet obstruction—spectrum and management. Trop Gastroenterol 32:259–266
Sheikh RA, Prindiville TP, Pecha RE, Ruebner BH (2009) Unusual presentations of eosinophilic gastroenteritis: case series and review of literature. World J Gastroenterol 15:2156–2161
Nugent FW, Roy MA (1989) Duodenal Crohn’s disease: an analysis of 89 cases. Am J Gastroenterol 84:249–254
Elms L, Moon RC, Varnadore S, Teixeira AF, Jawad MA (2014) Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2395 cases at a single institution. Surg Endosc 28:1624–1628
Sonavane SK, Menias CO, Kantawala KP, et al. (2012) Laparoscopic adjustable gastric banding: what radiologists need to know. Radiographics 32:1161–1178
Chandler RC, Srinivas G, Chintapalli KN, Schwesinger WH, Prasad SR (2008) Imaging in bariatric surgery: a guide to postsurgical anatomy and common complications. AJR Am J Roentgenol 190:122–135
Peterson CM, Anderson JS, Hara AK, et al. (2009) Volvulus of the gastrointestinal tract: appearances at multimodality imaging. Radiographics 29:1281–1293
Millet I, Orliac C, Alili C, Guillon F, Taourel P (2014) Computed tomography findings of acute gastric volvulus. Eur Radiol 24:3115–3122
Sandrasegaran K, Patel A, Fogel EL, Zyromski NJ, Pitt HA (2009) Annular pancreas in adults. AJR Am J Roentgenol 193:455–460
Unal B, Aktaş A, Kemal G, et al. (2005) Superior mesenteric artery syndrome: CT and ultrasonography findings. Diagn Interv Radiol 11:90–95
Raman SP, Neyman EG, Horton KM, Eckhauser FE, Fishman EK (2012) Superior mesenteric artery syndrome: spectrum of CT findings with multiplanar reconstructions and 3-D imaging. Abdom Imaging 37:1079–1088
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Millet, I., Doyon, F.C., Pages, E. et al. CT of gastro-duodenal obstruction. Abdom Imaging 40, 3265–3273 (2015). https://doi.org/10.1007/s00261-015-0497-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-015-0497-6