Abstract
Background
Internal hernia is a relatively common postoperative complication after Roux-en-Y gastric bypass (RYGB) procedure. It has been reported that 1–9 % of laparoscopic RYGB patients develop internal herniation through Peterson’s or mesenteric defect. However, a considerable number of patients presenting with possible small bowel obstruction (SBO) after laparoscopic RYGB do not always have internal herniation.
Purpose
The aim of our study was to determine the causes of SBO for patients in which both potential internal hernia spaces were closed at the time of the original operation.
Setting
Academic Practice, USA.
Materials and methods
Of 2,395 patients who underwent laparoscopic RYGB between January 2004 and October 2012, a total of 93 (3.9 %) patients were reoperated for possible SBO at our institution. A retrospective review of a prospectively collected database was performed for all patients.
Results
A total of 93 patients had 105 reoperations in the study period, resulting in a reoperation rate for possible SBO of 3.9 %. The mean time period between the laparoscopic RYGB and the first 93 reoperations was 20.9 ± 18.1 months (range 0–100). Eleven patients required secondary reoperations at a mean period of 20.1 ± 17.7 months (range 0–52) after the first reoperation. Of these 105 reoperations, 29 (27.6 %) showed internal herniation at the mesenteric defect (N = 23), Peterson’s defect (N = 5), and both (N = 1). A total of 50 (47.6 %) reoperations revealed extensive adhesions causing SBO. Of these 50 cases, 12 revealed adhesions at the jejunojejunostomy, causing it to kink and obstruct. Ten (9.5 %) cases showed intussusception of the jejunojejunal anastomosis. Overall, reoperation rate due to internal herniation was 1.1 % in our patient population.
Conclusions
Our findings indicate a 3.9 % reoperation rate for abdominal pain and SBO, and more than 45 % of these patients had symptoms secondary to adhesions. Only 1.1 % of our laparoscopic RYGB patients developed internal herniation after closure of both internal hernia spaces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is an increasingly problematic trend in the worldwide healthcare scene. As obesity and its comorbidities grow at an alarming rate, surgical therapies for the management of obesity have become more commonplace. More than 340,000 bariatric procedures were performed worldwide in 2011. In 2011, there were 47,791 Roux-en-Y gastric bypass (RYGB) procedures performed in the USA and Canada alone [1]. With the conversion from open to a laparoscopic approach for RYGB first reported in 1994 [2], the procedure has become the standard for surgical management of obesity [3]. A well documented complication of laparoscopic RYGB (LRYGB) is internal herniation leading to small bowel obstruction (SBO), with an incidence of between 1 and 9 % [4–9]. It also has been reported that the incidence of internal hernia is greater after LRYGB than after the open approach [10, 11]. Due to difficulties in detecting internal herniation on standard imaging modalities and the potentially catastrophic risk of a missed diagnosis, surgical exploration remains common in any patient with a high clinical suspicion of internal hernia [12]. Consequently, there have been numerous studies investigating permutations of the procedure to reduce internal hernia complications such as closure of Peterson’s defect, closure of the jejunojejunal mesenteric defect, and conversion to an antecolic approach, thus removing the potential retrocolic hernia space [4–8, 12]. In light of previously published internal hernia rates and reported techniques, we present a single surgeon’s, single-institution experience with 2,414 consecutive LRYGB patients.
Materials and methods
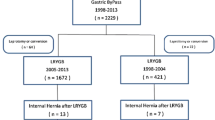
After Institutional Review Board approval, and following Health Insurance Portability and Accountability Act guidelines, the authors performed a retrospective chart review of a prospectively maintained database. This consisted of 2,414 patients who underwent primary LRYGB from 20 January 2004 to 11 October 2012.
LRYGB was performed by one surgeon according to the National Institutes of Health criteria for the management of morbid obesity. All patients underwent a laparoscopic antecolic, antegastric RYGB with routine closure of the Peterson’s defect and placement of a gastric remnant gastrostomy tube. The jejunojejunal mesenteric defect was not closed in the period between 13 March 2006 and 20 November 2010. Postoperatively, patients were followed-up at our office clinic at 1, 3, 6, and 12 months postoperatively and yearly thereafter. When patients presented with nausea, vomiting, or abdominal pain, an upper endoscopy, abdominal ultrasound, abdominal computed tomography (CT) and/or upper gastrointestinal imaging was performed for diagnosis. Patients with identified gall bladder pathology, ulceration, fistula, and strictures were not counted as possible SBO in the present study.
All patient data and complications were collected until the time of this review. Data collection included gender, age, body mass index (BMI), reoperations, findings on exploration, and follow-up time. All data for age and BMI are demonstrated as mean ± standard deviation, unless otherwise noted. Statistical analysis was performed using descriptive analysis.
Surgical technique
Laparoscopic Roux-en-Y gastric bypass technique
LRYGB was performed creating a 15–30 cc gastric pouch, with one transverse and four vertical firings of a linear stapler, on average. The jejunum was transected at 40 cm from the ligament of Treitz. Roux limb was measured for 75–150 cm depending on the patient’s BMI, and jejunojejunostomy was created using a linear stapler Echelon Endopath 45 and 60 (Ethicon Endo-surgery, Somerville, NJ, USA). The Roux limb was oriented in an antecolic, antegastric fashion. The Echelon Endopath 45 stapler was inserted in enterotomy and gastrotomy and fired at the 2.5 cm mark, creating the gastrojejunal anastomosis. The opening for the Endopath was closed transversely with the Echelon Endopath 45 and 60 in two applications after advancing the Edlich tube to the jejunum. No buttress material was used in the gastrojejunal anastomosis. The staple line was reinforced with a running stitch of 2-0 Polysorb. The Peterson’s defect and jejunojejunal mesenteric defect were closed using a 2-0 polysorb suture with a 10 mm Endo Stitch (Covidien, Mansfield, MA, USA) when applicable.
Of our 2,414 patients undergoing LRYGB, 13 were converted to an open procedure. One (0.04 %) mortality occurred due to ventricular tachycardia and cardiac arrest 15 days after the procedure.
Results
Of our 2,414 patient population, 18 (0.7 %) patients who were lost to follow-up and one (0.04 %) mortality patient were excluded from the data analysis. Reoperations for possible SBO occurred in 93 patients (3.9 %). Demographics of these patients are shown in Table 1.
Most patients complained of abdominal pain (N = 89), most commonly occurring in the left upper quadrant when identified, as intermittent, sharp, or crampy. Pain in the right upper quadrant, right lower quadrant, and left lower quadrant was reported in other patients. Of these patients, five also complained of nausea and vomiting at presentation. Four patients had major complaints of nausea and vomiting, with or without concurrent abdominal pain. Mean time elapsed from LRYGB to presentation was 20.9 ± 18.1 months (range 3 days–100 months). Nine (9.6 %) patients presented with abdominal pain within 30 days after the primary procedure.
Reasons for reoperations
These 93 patients required a total of 105 reoperations. Of the first 93 reoperations due to possible SBO, 45 (48.4 %) cases were related to adhesions (Fig. 1). Severe adhesion was the reason for SBO in 28 (30.1 %) reoperations, 11 (11.8 %) reoperations found adhesions causing kinking of the jejunojejunal anastomosis, and six (6.5 %) cases showed bands of adhesions resulting in SBO.
Internal herniation was identified as the reason for SBO in 26 (28.0 %) cases. Herniation through the mesenteric defect was more common, resulting in 20 (21.5 %) cases, while herniation through the Peterson’s defect only occurred in five (5.4 %) cases. One (1.1 %) case showed herniation through both defects.
A total of 10 (10.8 %) cases showed jejunojejunal intussusception, which was treated with release of intussusception with or without plication. Two (2.2 %) cases showed herniation through the opening of the omentum as the cause of SBO. Incisional hernia and diverticulitis were identified as the reason for SBO in one case each. This one patient with incisional hernia required small bowel resection. In eight (8.6 %) cases, no signs of SBO were identified.
Out of 67 cases without internal herniation, nine mesenteric defects and seven Peterson’s defects were closed as they were found to be open without evidence of internal herniation. All reoperations were done laparoscopically, except in three patients (3.2 %). One patient with incisional hernia, one with diverticulitis and one with severe adhesions were converted to open procedures.
Reasons for additional reoperations
Of these 93 patients, 11 (11.7 %) required additional 12 reoperations for possible SBO at a mean period of 20.1 ± 17.7 months (range 6 days–52 months) following the first reoperation. A descriptions of first and subsequent reoperations in these patients are shown in Fig. 2. Three out of five patients who were identified as having SBO due to adhesions were found to have mesenteric internal herniation at the second reoperations. One patient with extensive adhesions at her first reoperation underwent lysis of adhesions, small bowel resection, and revision of jejunojejunal anastomosis at the second reoperation.
All patients who had mesenteric internal hernia repaired at their first reoperation did not have further complications with internal herniation. However, one patient still showed opening of the mesenteric defect, which was closed again at the second reoperation. One patient from this group required a third reoperation 57 months following the second reoperation for possible SBO, which only showed extensive adhesions. All second and third reoperations were performed laparoscopically, except in two patients (16.7 %) who underwent extensive lysis of adhesions and were converted to an open procedure in their second reoperations.
All patients with reoperations did well after treatment at a mean follow-up of 36.5 ± 22.3 months (range 1–105 months). No mortality occurred after the reoperation.
Discussion
Our findings indicate an overall reoperative rate for possible SBO of 3.9 % in our population of 2,395 patients. Of those who needed reoperation for possible SBO, an average of 1.1 reoperations were required (105 reoperations in 93 patients). When the causes of SBO are delineated from intraoperative findings, the rate of internal hernia is 1.1 versus 1.9 % for SBO due to adhesions. Our rate is on the lower side when compared with the rate of 1–9 % for internal hernia previously published [4–7, 13, 14].
It has commonly been accepted that SBO after RYGB is an internal hernia until proven otherwise, usually in the form of operative exploration [13, 15]. However, in our patient population, 48.4 % of the first reoperations for SBO found adhesions to be the cause without the presence of an internal hernia, while 28.0 % had internal hernia as a finding. The occurrence of internal herniation was greatly lower than that in a published data by Rogula et al. [16], which reported 40.9 % internal hernia versus 34.1 % adhesions. The study by Rogula et al. [16] was weakened by their conversion from a retrocolic, retrogastric to an antecolic, antegastric approach during the study period. Our operations were all performed by the same surgeon at a single institution with the same antegastric, antecolic approach. This is one of the strengths of our study and reduces the chance of a difference in technique or postoperative management confounding the data. We routinely closed the Peterson’s defect, and our results show a significantly low number of internal herniation through the Peterson’s defect (N = 5) when compared with that of mesenteric defect (N = 20). We did not close the mesenteric defect from March 2006 to November 2011, and believe this had an impact on the number of patients with mesenteric internal herniation. Of note, we have had no patients with mesenteric internal hernia since we started closing the mesenteric defect in November 2011. Steele et al. [7] reported that the antecolic antegastric approach with closure of internal defects led to fewer internal hernias than the retrocolic retrogastric approach. Our data not only support that, but also show that we can decrease the chances of internal hernia by closing the defect in the antecolic antegastric approach.
It has been previously reported that a running closure of the mesenteric defect with non-absorbable suture has led to a decline in internal hernia rates [4, 6, 7]. Our technique was to use a 2-0 Polysorb, which has a reported tensile strength of 80 % at 2 weeks and 30 % at 3 weeks. The aim of closing the defects was to create natural adhesions between the two divided areas of mesentery and not to mechanically hold the edges together long term. When we look at our low number of internal herniation through Peterson’s defect, we believe the absorbable suture was enough to create natural adhesions.
Al Harakeh [11] named obstruction at the jejunojejunostomy as the second most common cause of SBO following antecolic LRYGB, at a rate of 1.8 % [17]. In our study population, the frequency of this complication was lower, at 0.5 %. It was also interesting to find ten cases of jejunojejunal intussusception. Intussusception is a rare but devastating complication when not diagnosed promptly [18, 19]. We believe that, when patients present with possible SBO, intussusception should be considered for differential diagnosis. We would also like to note that no patient required small bowel resection among those with internal herniation, while one patient with extensive adhesion and one with incisional hernia did. Out study demonstrates various other reasons for SBO following LRYGB, most of which can be safely managed laparoscopically. A lower frequency of internal herniation did not necessarily mean fewer reoperations, as extensive adhesion can be the more common reason for SBO, and the treatment for SBO following RYGB is surgical.
The weakness of our study is that it is a retrospective review. Also, we were only able to gather reoperation information carried out at our institution. Of note, our bariatric surgeon performed general surgical procedures, including diagnostic laparoscopy and cholecystectomy, on our patients who needed them after the bariatric procedure [20]. Furthermore, the patients in the later portion of our data collection would still be within the average period of reoperation, potentially confounding our data and leading to an under-reporting of internal hernia and SBO rates. Nevertheless, we believe that a large enough number of patients were included in this study to validate our results.
Conclusions
Our retrospective review of 2,395 consecutive LRYGB cases reveals a rate of 3.9 % reoperation for SBO. Internal hernia accounted for 28.0 % of these reoperations, while adhesions accounted for 48.4 %. Our rate of internal hernia with routine closure of Peterson’s defect in antecolic, antegastric technique was 1.1 %.
References
Buchwald H, Oien DM (2013) Metabolic/bariatric surgery worldwide 2011. Obes Surg 23:427–436
Wittgrove AC, Clark GW, Tremblay LJ (1994) Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg 4:353–357
Samuel I, Mason EE, Renguist KE, Huang YH, Zimmerman MB, Jamal M (2006) Bariatric surgery trends: an 18-year report from the international bariatric surgery registry. Am J Surg 192:657–662
Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux-en-Y gastric bypass: incidence, treatment and prevention. Obes Surg 13:350–354
Schneider C, Cobb W, Scott J, Carbonell A, Myers K, Bour E (2011) Rapid excess weight loss following laparoscopic gastric bypass leads to increased risk of internal hernia. Surg Endosc 25:1594–1598
Carmody B, DeMaria EJ, Jamal M, Johnson J, Carbonell A, Kellum J, Maher J (2005) Internal hernia after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 1:543–548
Steele KE, Prokopowicz GP, Magnuson T, Lidor A, Schweitzer M (2008) Laparoscopic antecolic Roux-en-Y gastric bypass with closure of internal defects leads to fewer internal hernias than the retrocolic approach. Surg Endosc 22:2056–2061
Cho M, Pinto D, Carrodeguas L, Lascano C, Soto F, Whipple O, Simpfendorfer C, Gonzalvo JP, Zundel N, Szomstein S, Rosenthal RJ (2006) Frequency and management of internal hernias after laparoscopic antecolic antegastric Roux-en-Y gastric bypass without division of the small bowel mesentery or closure of mesenteric defects: review of 1400 consecutive cases. Surg Obes Relat Dis 2:87–91
Santo MA, Pajecki D, Riccioppo D, Cleva R, Kawamoto F, Cecconello I (2013) Early complications in bariatric surgery: incidence, diagnosis and treatment. Arq Gastroenterol 50:50–55
Garza E Jr, Kuhn J, Arnold D, Nicholson W, Reddy S, McCarthy T (2004) Internal hernia after laparoscopic Roux-en-Y gastric bypass. Am J Surg 188:796–800
Al Harakeh AB (2011) Complications of laparoscopic Roux-en-Y gastric bypass. Surg Clin North Am 91:1225–1237
Griffith PS, Birch DW, Sharma AM, Karmali S (2012) Managing complications associated with laparoscopic Roux-en-Y gastric bypass for morbid obesity. Can J Surg 55:329–336
Champion JK, Williams M (2003) Small bowel obstruction and internal hernias after laparoscopic Roux-en-Y gastric bypass. Obes Surg 13:596–600
Felsher J, Brodsky J, Brody F (2003) Small bowel obstruction after laparoscopic Roux-en-Y gastric bypass. Surgery 134:501–505
Capella RF, Iannace VA, Capella JF (2006) Bowel obstruction after open and laparoscopic gastric bypass surgery for morbid obesity. J Am Coll Surg 203:328–335
Rogula T, Yenumula PR, Schauer PR (2007) A complication of Roux-en-Y gastric bypass: intestinal obstruction. Surg Endosc 21:1914–1918
Lewis CE, Jensen C, Tejirian T, Dutson E, Mehran A (2009) Early jejunojejunostomy obstruction after laparoscopic gastric bypass: case series and treatment algorithm. Surg Obes Relat Dis 5:203–207
Daellenbach L, Suter M (2011) Jejunojejunal intussusception after Roux-en-Y gastric bypass: a review. Obes Surg 21:253–263
Simper SC, Erzinger JM, McKinlay RD, Smith SC (2010) Laparoscopic reversal of gastric bypass with sleeve gastrectomy for treatment of recurrent retrograde intussusception and Roux stasis syndrome. Surg Obes Relat Dis 6:684–688
Moon RC, Teixeira AF, DuCoin C, Varnadore S, Jawad MA (2013) Comparison of cholecystectomy incidences after Roux-en-Y gastric bypass, sleeve gastrectomy and gastric banding. Surg Obes Relat Dis. doi:10.1016/j.soard.2013.04.019
Disclosures
Muhammad Jawad and Andre Teixeira are consultants of Ethicon Endo-surgery. Luke Elms, Sheila Varnadore, and Rena Moon have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elms, L., Moon, R.C., Varnadore, S. et al. Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2,395 cases at a single institution. Surg Endosc 28, 1624–1628 (2014). https://doi.org/10.1007/s00464-013-3361-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3361-1