Abstract
Avian influenza virus (AIV) is spreading worldwide and is a serious threat to the health of poultry and humans. In many countries, low pathogenic AIVs, such as H9N2, have become an enormous economic burden on the commercial poultry industry because they cause mild respiratory disease and decrease egg production. A recombinant Lactobacillus plantarum NC8 strain expressing NP-M1-DCpep from H9N2 AIV has been studied in a mouse model. However, it remains unknown whether this L. plantarum strain can induce an immune response and provide protection against H9N2 AIV in chickens. In this study, chickens that were orally vaccinated with NC8-pSIP409-NP-M1-DCpep exhibited significantly increased T cell-mediated immune responses and mucosal sIgA and IgG levels, which provided protection against H9N2 AIV challenge. More importantly, compared with oral administration of NC8-pSIP409-NP-M1-DCpep, intranasal administration induced stronger immune responses and provided effective protection against challenge with the H9N2 virus by reducing body weight loss, lung virus titers, and throat pathology. Taken together, these findings suggest that L. plantarum expressing NP-M1-DCpep has potential as a vaccine to combat H9N2 AIV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Avian influenza, an important infectious disease caused by the avian influenza virus (AIV) (Chu et al. 2016; Wang et al. 2016), not only can cause serious economic losses to the poultry industry (Liu et al. 2015) but is also a threat to human health (Zhang et al. 2016). Based on differences in surface glycoproteins (hemagglutinin (HA) and neuraminidase (NA)), AIVs can be divided into 18 HA and 11 NA subtypes (Tong et al. 2013). First found in the USA in 1966, the AIV H9N2 subtype has since spread worldwide. Several recent studies report the generation of zoonotic influenza viruses, such as the highly pathogenic H7N9 and H10N8 viruses, from H9N2 AIV internal segments (Chen et al. 2014; Gao et al. 2013). Thus far, vaccines are the most effective means of controlling the spread of AIVs. However, given the genetic variation of these viruses, a vaccine based on AIV surface proteins can provide only limited protection (Pu et al. 2015). Nonetheless, inactivated vaccines that induce antibodies may be implemented to control AIV infection.
The nucleoprotein (NP) and matrix proteins (M1) of AIV are the most typical internal conserved proteins and the most promising targets for vaccine development. Berthoud et al. showed that Modified Vaccinia Ankara (MVA) expressing influenza virus conserved internal antigens (NP and M1) can produce T cell responses that cross-protect against heterologous influenza infections (Berthoud et al. 2011). In addition, clinical studies have demonstrated that the use of adenovirus vector expressing influenza virus NP can induce an NP-specific T cell immune response and can provide resistance against heterologous influenza virus infections (Antrobus et al. 2012; Powell et al. 2013). However, few oral vaccines based on the NP and M1 proteins have been reported.
Lactic acid bacteria (LAB) are a class of bacteria that can ferment carbohydrates to generate large amounts of lactic acid (Taniguchi et al. 2004). LAB are regarded as safe food-grade microorganisms by the international community, can survive for a long time in the body, and exert probiotic effects (Garcia-Crespo et al. 2013; Ou et al. 2016). For example, a previous study showed that oral plant Lactobacillus can protect mice against fatal influenza virus infection (Kikuchi et al. 2014), and more recent research shows that sublingual vaccination with Lactobacillus can also produce this antiviral effect in mice (Lee et al. 2013). Furthermore, several studies have shown that LAB are an important tool due to their ability to deliver heterologous proteins (which is useful for genetic engineering) (Lei et al. 2015a; Steidler et al. 2000; Steidler et al. 2003) as well as other advantages, such as ease of cultivation, safety, and lack of toxicity (Nguyen et al. 2011). Importantly, L. plantarum has recently been employed to deliver antigens from pathogens to immunize against infection with those pathogens (Grangette et al. 2001; Liu et al. 2016; Shi et al. 2016; Yang et al. 2016a). Although several investigations have suggested that oral vaccines may be effective, not all attempts have been successful.
Dendritic cells (DCs) have a critical role in priming adaptive immune responses (Mohamadzadeh et al. 2005). One investigation reported that DCs in the lamina propria are able to extend dendrites through the basement membrane and between epithelial cells into the gut lumen of the host (Niess et al. 2005). Depending on the microbial stimulus, DCs can promote the development of unprimed, naive, T cells toward a Th1, Th2, Th17, and/or Treg response or an unpolarized T cell response (Mohamadzadeh et al. 2005). We previously generated L. plantarum expressing NP-M1-DCpep and found that it induced DC activation (specifically T and B cell immune responses in vaccinated mice) and provided protection against challenges with various influenza virus subtypes. Importantly, in an adoptive transfer study, we confirmed that this protection in NC8-pSIP409-NP-M1-DCpep-primed mice was provided only by CD8+ T cells and not by CD4+ T cells (Yang et al. 2016b). In the current study, we tested the level of specific sIgA and lymphocyte proliferation in chickens after oral vaccination with NC8-pSIP409-NP-M1-DCpep. In addition, the protective role of the recombinant L. plantarum against H9N2 AIV infection was evaluated in terms of weight loss, pathological damage, and virus load in challenged chickens.
Materials and methods
Reagents and strains
The A/duck/Xuzhou/07/2003(H9N2) virus was stored in our laboratory. L. plantarum strain NC8 (CCUG 61730) has been deposited in the culture collection (University of Göteborg, Sweden). The NC8-pSIP409, NC8-pSIP409-NP-M1-Ctrlpep ,and NC8-pSIP409-NP-M1-DCpep were constructed as published article (Yang et al. 2016b). Recombinant NP and M1 proteins were purified by Yuying Liu. The monoclonal anti-chicken CD3 (clone CT3), anti-chicken CD4 (clone CT4), and anti-chicken CD8 (clone CT8) antibodies were obtained from Southern Biotech (SBA) (San Diego, CA, USA).
Animals and ethics statement
Specific pathogen-free (SPF) white leghorn layer chickens were purchased from Beijing Merial Vital Laboratory Animal Technology Co., Ltd., China. The birds were housed in the SPF Animal Center at Jilin Agricultural University. The protocol for the animal studies was approved by the Animal Care and Ethics Committees of Jilin Agriculture University.
Flow cytometry
Flow cytometry was carried out according to a previously published protocol (Shi et al. 2016). Monoclonal anti-chicken CD3 (clone CT3), anti-chicken CD4 (clone CT4), and anti-chicken CD8 (clone CT8) antibodies were used for staining. Standard flow cytometry detection was performed using a BD LSRFortessa™, and the data were analyzed using FlowJo 7.6.2 software.
T cell stimulatory index
Chicken lymphocyte proliferation in response to rNP and rM1 proteins was assessed as previously described (Shi et al. 2016). Two weeks after the final vaccination, splenic lymphocytes were obtained from all groups of chickens to detect the proliferative response of lymphocytes. The lymphocytes were then plated in 96-well plates at 200 μl per well containing 2 × 105 cells and co-cultured at 37 °C for 68 h in the presence or absence of recombinant NP and M1 proteins at 5 μg/ml final concentration. Four hours before detection, 20 μl of (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) (MTS) was added to the plates, and the cells were incubated at 37 °C for 4 h. The samples were then assessed using a Standard Enzyme reader at 570 nm. The proliferative capacity of chicken lymphocytes was described as the stimulatory index (SI = cpm of stimulated samples/cpm of control samples).
Measurement of antigen-specific antibodies (IgA and IgG)
Bronchoalveolar lavage fluids (BALF) and sera from chicken were collected 2 weeks after the booster vaccination. IgA and IgG specific for NP and M1 BALF or serum were detected by ELISA, as described previously (Haan et al. 2001). In brief, purified NP and M1 antigens at 5 μg/ml were incubated on 96-well plates at 4 °C for 12 h. Serially diluted samples were added for 2 h at room temperature and then incubated with biotin (Biot)-conjugated mouse anti-chicken IgA or IgG at room temperature for 1 h (Southern Biotech). The plates were incubated with horseradish peroxidase (HRP)-conjugated streptavidin at room temperature for 30 min (Southern Biotech). End-point titers were determined as the highest dilution generating an absorbance two times higher than the background for BALF samples and three times higher than the background for serum samples.
Animal immunizations and challenge
Twenty-day-old chickens were randomly divided into seven groups of 15 chickens each, as follows: PBS-non-challenge group, PBS-challenge group, NC8-pSIP409 group, NC8-pSIP409-NP-M1-Ctrlpep group, intranasal NC8-pSIP409-NP-M1-DCpep group, oral NC8-pSIP409-NP-M1-DCpep group, and AIV-inactivated vaccine group. The chickens were vaccinated with recombinant L. plantarum by gavage, and an H9N2-inactivated vaccine (Weike Biotechnology) was injected at 100 μl/chicken as the positive control. Each group of experimental animals was administered 200 μl PBS only or 200 μl PBS containing 109 colony-forming units (CFU) of recombinant L. plantarum at 1, 2, and 3 days. The chickens received a booster vaccination at 14, 15, and 16 days after the initial dosing. Two weeks after the final vaccination, chickens from all groups were anesthetized via intramuscular injection of xylazine (1 mg/kg) and ketamine (20 mg/kg) and inoculated intranasally (i.n.) with 106.5 EID50 of virus-allantoic fluid (contained A/duck/Xuzhou/07/2003) in a 0.1 ml volume. All chickens (n = 8) were observed daily for 10 days for body weight changes and signs of disease. The lungs (n = 4) from infected chickens were removed on day 5 for virus titration in SPF-embryonated chicken eggs.
Histopathological detections
Five days after viral challenge, the throat and lungs from AIV-infected chickens were isolated and fixed with 4% paraformaldehyde for examining pathological changes. The samples were then embedded in paraffin, sectioned, and stained with hematoxylin and eosin (H&E). The samples were scored by blinded pathologists (three independent readers). In brief, alveolitis and peribronchiolar inflammation were blind scored on a scale of 0, 1, 2, 3, 4, or 5 corresponding to none, very mild, mild, moderate, marked, or severe inflammation, respectively (Yang et al. 2016b).
Statistical analysis
All data in this study are presented as geometric mean titers, with the mean being derived from at least three independent experiments. Significance was assessed using unpaired two-tailed t tests and one-way analysis of variance (ANOVA; Tukey’s multiple comparison test).
Results
Effects of recombinant L. plantarum on specific T cell responses
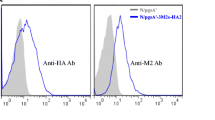
NC8-pSIP409-NP-M1-DCpep was constructed as previously described; AIV antigens were synthesized and confirmed previously (Yang et al. 2016b). To investigate whether NC8-pSIP409-NP-M1-DCpep can trigger a T cell response, chickens were vaccinated with recombinant L. plantarum via various routes (Fig. 1b). Two weeks after booster vaccination, splenocytes were isolated, and T cells were detected by flow cytometry (Fig. 2a). In the oral administration groups, the results showed a higher frequency of CD3+CD4+ and CD3+CD8+ T cells in the spleens of chickens vaccinated with NC8-pSIP409-NP-M1-DCpep than in the control groups (Fig. 2b, c). In addition, the chickens that were vaccinated with the inactivated H9N2 vaccine had a higher frequency of CD3+CD4+ T cells, as opposed to CD3+CD8+ T cells, than the other groups (Fig. 2b, c). Interestingly, a significantly higher frequency of CD3+CD8+ T cells was observed in the intranasally vaccinated NC8-pSIP409-NP-M1-DCpep chickens than in the orally vaccinated group (Fig. 2c).
The immunization scheme for chickens. Chickens were grouped as described in the “Materials and methods” section and orally or nasally vaccinated with a priming immunization on days 1, 2, and 3 and with a booster immunization on days 14, 15, and 16. Samples from the trachea and serum were obtained on day 30 after the first priming immunization, and all chickens were challenged with AIV (106.0 EID50) on day 14 after booster immunization. Five days after the challenge experiments, samples from the lungs were obtained to evaluate the pathology and virus titer
Recombinant L. plantarum elicited T cell responses in the spleen of vaccinated chickens. a Gating strategy for CD3+CD4+ or CD3+CD8+ T cells. The frequencies of CD3+CD4+ T cell subsets (b) and CD3+CD8+ T cell subsets (c) in the spleens of vaccinated chickens were analyzed by flow cytometry. The immunization approaches are displayed at the top. Data are presented as the means ± S.E.M of triplicate tests (n = 3 chickens in each group), and the statistical significance of differences between groups was assessed by one-way ANOVA (# P < 0.05, *P < 0.05, **P < 0.01, and ***P < 0.001)
To further determine whether NC8-pSIP409-NP-M1-DCpep can induce specific T cell responses, antigen-specific T lymphocyte responses in chickens were detected 2 weeks after oral vaccination. The results showed a notably higher T cell proliferative response in chickens orally vaccinated with NC8-pSIP409-NP-M1-DCpep than in chickens orally vaccinated with NC8-pSIP409-NP-M1-Ctrlpep (Fig. 3). In addition, we also found that intranasal vaccination with NC8-pSIP409-NP-M1-DCpep induced a stronger T cell proliferative response than did oral vaccination (Fig. 3). These results demonstrate that oral or intranasal immunization with recombinant L. plantarum can elicit specific T cell-mediated immune responses.
Antigen-specific lymphocyte response following vaccination in chickens. Splenocytes from the chickens in all groups were isolated 2 weeks after last booster vaccination and co-cultured with 5 μg/ml of purified NP and M1 antigens for 72 h. The immunization approaches are displayed at the top. Data are expressed as the means ± S.E.M of triplicate tests (n = 3 chickens in each group), and the statistical significance of differences between groups was assessed by one-way ANOVA (# P < 0.05,*P < 0.05, **P < 0.01, and ***P < 0.001)
Effects of recombinant L. plantarum on specific sIgA antibody
Three-week-old chickens were vaccinated by oral or intranasal administration of recombinant L. plantarum. To explore whether NC8-pSIP409-NP-M1-DCpep can elicit an antigen-specific mucosal immune response, specific sIgA in BALF from vaccinated chickens was assessed by ELISA at 2 weeks after the final immunization. The data indicated a higher sIgA titer in chickens that had been orally vaccinated with NC8-pSIP409-NP-M1-DCpep and inactivated H9N2 vaccine than in other groups using the same immunization route (Fig. 4). However, a higher titer of specific IgA in BALF was induced by intranasal immunization with NC8-pSIP409-NP-M1-DCpep than by oral immunization. These results suggest that a stronger mucosal immune response occurred when the chickens were intranasally immunized with NC8-pSIP409-NP-M1-DCpep.
NP-M1-specific IgA titers in the BALF after immunization. Samples from the chickens in all groups were obtained 2 weeks after last booster vaccination, and specific IgA titers were detected using purified NP and M1 antigens. Data are presented as the means ± S.E.M of triplicate tests (n = 3 chickens in each group), and the statistical significance of differences between groups was assessed by one-way ANOVA (# P < 0.05,*P < 0.05, **P < 0.01, and ***P < 0.001)
Effects of recombinant L. plantarum on specific IgG antibody
We used indirect ELISA to detect antigen-specific IgG in serum at 2 weeks after the final vaccination. The results showed that NC8-pSIP409-NP-M1-DCpep significantly enhanced the antigen-specific serum IgG titer compared with the NC8-pSIP409 group and NC8-pSIP409-NP-M1-Ctrlpep group, but there were no significant differences between the intranasal NC8-pSIP409-NP-M1-DCpep group and the inactivated H9N2 vaccine group (or the oral NC8-pSIP409-NP-M1-DCpep group) (Fig. 5). In addition, a significantly higher antigen-specific serum IgG titer was found in the NC8-pSIP409-NP-M1-Ctrlpep group compared to the NC8-pSIP409 or PBS group (Fig. 5).
NP-M1-specific IgG titers in the serum after immunization. Serum from chickens in all groups was obtained 2 weeks after the booster vaccination, and specific IgG titers were detected using purified NP and M1 antigens. Data are shown as the means ± S.E.M of triplicate tests (n = 3∼5 chickens in each group), and the statistical significance of differences between groups was assessed by one-way ANOVA (*P < 0.05 and ***P < 0.001)
Evaluation of recombinant L. plantarum-induced protection
Chickens were vaccinated with recombinant L. plantarum in accordance with the prime-boost procedure (Fig. 1b). To evaluate whether NC8-pSIP409-NP-M1-DCpep provided protective immunity against the H9N2 subtype of AIV, the chickens were infected with 105 EID50 A/duck/Xuzhou/07/2003 (H9N2) 2 weeks after the final vaccination. Our results indicated body weight increases slowly in the inactivated H9N2 vaccine group after infection with AIV (Fig. 6a). However, chickens that had been vaccinated orally with NC8-pSIP409-NP-M1-DCpep lost significantly less weight than those vaccinated with NC8-pSIP409-NP-M1-Ctrlpep, NC8-pSIP409, or PBS, as measured on days 5 and 6 after challenge with H9N2 AIV (Fig. 6b). As expected, chickens vaccinated intranasally with NC8-pSIP409-NP-M1-DCpep lost less weight than orally vaccinated chickens, as measured on day 6 after challenge (Fig. 6b).
Vaccination of chickens with recombinant NC8-pSIP409-NP-M1-DCpep provided protection against AIV infection (106.0 EID50). a, b Weight loss (%) of the chickens (n = 8 chickens in each group) in all groups after challenge. c Five days after challenge with AIV, the lungs (n = 4 chickens in each group) were obtained, and titers were assessed by TCID50. The results are expressed as the means ± S.E.M of triplicate tests, and the statistical significance of differences between groups was assessed by one-way ANOVA (# P < 0.05,*P < 0.05, **P < 0.01, and ***P < 0.001)
In addition, the virus titer in the lungs of vaccinated chickens was also measured on day 5 after challenge with H9N2 AIV, and chickens that had been vaccinated orally with NC8-pSIP409-NP-M1-DCpep had lower virus titers than those vaccinated with NC8-pSIP409-NP-M1-Ctrlpep, NC8-pSIP409, or PBS (Fig. 6c). We also found that chickens vaccinated intranasally with NC8-pSIP409-NP-M1-DCpep showed a much lower virus titer in the lungs after AIV challenge than the oral NC8-pSIP409-NP-M1-DCpep group (Fig. 6c). These data suggested that L. plantarum expressing NP-M1-DCpep can provide protection against H9N2 AIV infection.
Protection against tissue pathology in chickens vaccinated with recombinant L. plantarum
Two weeks after the final vaccination, the chickens were challenged with AIV, and the lungs and throat tissue were isolated at 5 days after challenge to examine the pathology. As shown in Fig. 7, the lungs from the NC8-pSIP409 and PBS groups displayed the following: terminal bronchioles with epithelial shedding, increased mucus, blood, lymphatic cells, and blood vessels; hyperemia; and obvious lymphocyte infiltration around blood vessels. The lungs of chickens orally vaccinated with NC8-pSIP409-NP-M1-Ctrlpep exhibited terminal bronchiolar epithelial shedding, and although the typical phenomenon of lymphocytic infiltration was not present, blood vessel gap shed clearly widened (Fig. 7a, b). In contrast, the lungs of chickens vaccinated with the inactivated H9N2 vaccine and the oral and intranasal NC8-pSIP409-NP-M1-DCpep groups did not show obvious inflammatory cell infiltration or other visible pathological damage (Fig. 7a, b).
Vaccination of chickens with recombinant NC8-pSIP409-NP-M1-DCpep provided protection against lung damage due to AIV infection (106.0 EID50). a Five days after challenge with AIV, the lungs were obtained and evaluated by histopathological analysis. Sections were stained with HE; magnification at ×100. Scale bar, 10 μm. b The histopathological scores for lung sections from H9N2-infected chickens. Lung sections were scored by an observer blinded to the chicken identity for lung inflammation on a scale from 0 to 5. The results are expressed as the means ± S.E.M of triplicate tests, and the statistical significance of differences between groups was assessed by one-way ANOVA (**P < 0.01 and ***P < 0.001)
To determine whether recombinant L. plantarum can reduce the observed throat pathology, all groups were challenged with AIV at 2 weeks after the final vaccination, and throats were isolated 5 days later. The data showed mucosal bleeding and epithelial necrosis in the PBS and NC8-pSIP409 groups (Fig. 8). Interestingly, the throats from AIV-challenged chickens that had been vaccinated orally with NC8-pSIP409-NP-M1-DCpep exhibited minimal damage, in contrast to those of the NC8-pSIP409-NP-M1-Ctrlpep group (Fig. 8a, b). In addition, we also found less inflammation in the intranasal NC8-pSIP409-NP-M1-DCpep group compared to the oral NC8-pSIP409-NP-M1-DCpep group (Fig. 8a, b).
Histopathological examination of throats in chickens challenged with AIV (106.0 EID50). a Five days after challenge with AIV, throats were obtained and evaluated by histopathological analysis. Sections were stained with HE; magnification at ×100. Scale bar, 10 μm. b The histopathological scores for throat sections from H9N2-infected chickens. Throat sections were scored by an observer blinded to the chicken identity for throat inflammation on a scale from 0 to 5. The results are expressed as the means ± S.E.M of triplicate tests, and the statistical significance of differences between groups was assessed by one-way ANOVA (**P < 0.01 and ***P < 0.001)
Discussion
The main purpose of this study was to build on a previous study that evaluated the function of immunization with recombinant L. plantarum expressing NP-M1-DCpep, the results of which suggested that recombinant L. plantarum expressing NP-M1-DCpep can induce specific T cell immune responses and confer cross-protection against different subtypes of influenza virus in mice (Yang et al. 2016b). Several reports by Lei et al. indicated that chickens immunized with recombinant Lactococcus lactis have improved mucosal IgA responses and cellular immune responses as well as neutralizing antibody responses; in fact, these responses resulted in complete protection against H5N1 AIV infection (Lei et al. 2015b; Lei et al. 2015c). Our data in the present study showed that oral or intranasal vaccination of chickens with recombinant L. plantarum expressing NP-M1-DCpep also enhanced mucosal IgA responses and cellular immune responses and provided a protective immune response against AIV challenge.
Although existing vaccines based on AIV surface antigens induce antibodies against AIV challenge, previous investigations by our laboratory and others show that specific T cell immune responses are also induced in most patients and animals immunized with these vaccines, helping to provide protective immunity against pathogen infection (Berthoud et al. 2011; Yang et al. 2016b). Another study reported that mice vaccinated with purified M1 antigen and chitosan had strong cellular immune responses and were protected against infection with various subtypes of influenza virus (Sui et al. 2010). In addition, it has been reported that oral administration of recombinant hemagglutinin-expressing Lactobacillus spp. to mice enhances the antigen-specific splenic lymphocyte proliferative reaction and IL-4 levels but not IFN-γ levels (Wang et al. 2012). However, our data in this study found that chickens vaccinated with NC8-pSIP409-NP-M1-DCpep had a higher frequency of CD3+CD4+ and CD3+CD8+ T cells and a higher T cell proliferative response than the control groups. Hence, the conserved antigen from AIV can induce specific T cell immune responses and provide cross-protection against AIV infection (Yang et al. 2016b). Our next study will evaluate whether recombinant L. plantarum expressing NP-M1-DCpep can elicit protective immunity against challenge with other subtypes of AIV, including H5N1 and H7N9.
AIV first infects the epithelial cells of the respiratory tract of the host, resulting in serious pathological reactions in the host during infection. The sIgA secreted at the mucosal site can play an important role in clearing pathogens, such as AIV. Several studies have found that animals developed a higher level of sIgA after oral administration of Lactobacillus gasseri SBT2055 or heat-killed Lactobacillus pentosus b240, providing efficient protection against influenza virus challenge, though the exact mechanisms are not clear (Kiso et al. 2013; Nakayama et al. 2014). In addition, our published data revealed significant titers of specific sIgA developed in mice after oral administration of recombinant L. plantarum expressing HA or NP-M1-DCpep (Shi et al. 2014; Yang et al. 2016b). In the present study, our results showed that chickens vaccinated with recombinant L. plantarum expressing NP-M1-DCpep had higher sIgA titers in BALF than the control groups. These results suggested that specific sIgA elicited by recombinant L. plantarum may play a major function in inhibiting AIV replication, leading to reduced titers in the lungs and pathological damage to the lungs and throat.
The route of immunization has a primary role in the induction of protective immune responses against challenge by pathogenic microorganisms. Previous research has shown that mice sublingually vaccinated with Lactobacillus can develop effective protection from infection by influenza virus (Lee et al. 2013). In addition, a recent study indicated that strong mucosal and humoral immunity is induced in ferrets vaccinated intranasally with recombinant Lactococcus lactis and that this immunity provided effective protection against H5N1 AIV infection (Lei et al. 2015a). In our study, strong immune responses were elicited in intranasally immunized chickens, and our results are in accordance with other studies suggesting that intranasal administration confers better protection for birds infected with AIV than does oral vaccination (Li et al. 2015). Hence, to reduce the required manpower and material resources, intranasal immunization is very suitable for domestic pets, whereas oral immunization is suitable for large-scale poultry breeding.
There are different principles of vaccine design, and several studies have reported that different types of vaccines or adjuvants can trigger different immune responses. Inactivated vaccines induce a humoral immune response against pathogens, whereas recombinant replication-deficient adenovirus or MVA elicit a strong cellular immune response to provide efficient protection against an influenza virus challenge (Lambe et al. 2013). In addition, virus-like particle (VLP)-based vaccines can induce robust cross-reactive CD8+ T cell responses, which are advantageous against challenge with homologous influenza viruses (Schotsaert et al. 2016). A previous study showed that mRNA-based vaccines also triggered B and T cell-dependent protective effects that target multiple antigens to provide cross-protective immunity (Petsch et al. 2012). Furthermore, oral recombinant L. plantarum has been shown to enhance the expression of co-stimulatory molecules or the secretion of several cytokines that regulate the function of DCs (Christensen et al. 2002; Meijerink et al. 2010; Yang et al. 2016b). Several investigations have found that oral vaccines can induce Tregs, which play important roles in regulating the pathological damage in the lungs of infected animals due to excessive immune responses (Kathania et al. 2013; Lee et al. 2013).
In conclusion, the present study showed that DCpep targeting conserved influenza virus NP-M1 antigens and expressed by L. plantarum provided protection against AIV infection by increasing adaptive immune responses. Oral immunization resulted in notable increases in T cell responses and specific IgG and sIgA secretion and protection against viral challenge in vivo. In addition, these results suggested that intranasal immunization with NC8-pSIP409-NP-M1-DCpep results in a strong immune response in chickens, with more effective protection against AIV infection than oral immunization. The approach of using a non-traditional vaccine is a new strategy for the prevention and control of the spread of AIV.
References
Antrobus RD, Lillie PJ, Berthoud TK, Spencer AJ, McLaren JE, Ladell K, Lambe T, Milicic A, Price DA, Hill AV, Gilbert SC (2012) A T cell-inducing influenza vaccine for the elderly: safety and immunogenicity of MVA-NP+M1 in adults aged over 50 years. PLoS One 7(10):e48322. doi:10.1371/journal.pone.0048322
Berthoud TK, Hamill M, Lillie PJ, Hwenda L, Collins KA, Ewer KJ, Milicic A, Poyntz HC, Lambe T, Fletcher HA (2011) Potent CD8+ T-cell immunogenicity in humans of a novel heterosubtypic influenza A vaccine, MVA-NP+M1. Clin Infect Dis 52(1):1–7
Chen H, Yuan H, Gao R, Zhang J, Wang D, Xiong Y, Fan G, Yang F, Li X, Zhou J, Zou S, Yang L, Chen T, Dong L, Bo H, Zhao X, Zhang Y, Lan Y, Bai T, Dong J, Li Q, Wang S, Zhang Y, Li H, Gong T, Shi Y, Ni X, Li J, Zhou J, Fan J, Wu J, Zhou X, Hu M, Wan J, Yang W, Li D, Wu G, Feng Z, Gao GF, Wang Y, Jin Q, Liu M, Shu Y (2014) Clinical and epidemiological characteristics of a fatal case of avian influenza A H10N8 virus infection: a descriptive study. Lancet 383(9918):714–721. doi:10.1016/s0140-6736(14)60111-2
Christensen HR, Frokiaer H, Pestka JJ (2002) Lactobacilli differentially modulate expression of cytokines and maturation surface markers in murine dendritic cells. J Immunol 168(1):171–178
Chu J, Zhang Q, Zhang T, Han E, Zhao P, Khan A, He C, Wu Y (2016) Chlamydia psittaci infection increases mortality of avian influenza virus H9N2 by suppressing host immune response. Sci Rep 6:29421. doi:10.1038/srep29421
Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Li X, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Zhang Y, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y (2013) Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med 368(20):1888–1897. doi:10.1056/NEJMoa1304459
Garcia-Crespo KE, Chan CC, Gabryszewski SJ, Percopo CM, Rigaux P, Dyer KD, Domachowske JB, Rosenberg HF (2013) Lactobacillus priming of the respiratory tract: heterologous immunity and protection against lethal pneumovirus infection. Antivir Res 97(3):270–279. doi:10.1016/j.antiviral.2012.12.022
Grangette C, Muller-Alouf H, Goudercourt D, Geoffroy MC, Turneer M, Mercenier A (2001) Mucosal immune responses and protection against tetanus toxin after intranasal immunization with recombinant Lactobacillus plantarum. Infect Immun 69(3):1547–1553. doi:10.1128/iai.69.3.1547-1553.2001
Haan L, Verweij WR, Holtrop M, Brands R, van Scharrenburg GJ, Palache AM, Agsteribbe E, Wilschut J (2001) Nasal or intramuscular immunization of mice with influenza subunit antigen and the B subunit of Escherichia coli heat-labile toxin induces IgA- or IgG-mediated protective mucosal immunity. Vaccine 19(20–22):2898–2907
Kathania M, Zadeh M, Lightfoot YL, Roman RM, Sahay B, Abbott JR, Mohamadzadeh M (2013) Colonic immune stimulation by targeted oral vaccine. PLoS One 8(1):e55143. doi:10.1371/journal.pone.0055143
Kikuchi Y, Kunitoh-Asari A, Hayakawa K, Imai S, Kasuya K, Abe K, Adachi Y, Fukudome S, Takahashi Y, Hachimura S (2014) Oral administration of Lactobacillus plantarum strain AYA enhances IgA secretion and provides survival protection against influenza virus infection in mice. PLoS One 9(1):e86416. doi:10.1371/journal.pone.0086416
Kiso M, Takano R, Sakabe S, Katsura H, Shinya K, Uraki R, Watanabe S, Saito H, Toba M, Kohda N, Kawaoka Y (2013) Protective efficacy of orally administered, heat-killed Lactobacillus pentosus b240 against influenza a virus. Sci Rep 3:1563. doi:10.1038/srep01563
Lambe T, Carey JB, Li Y, Spencer AJ, van Laarhoven A, Mullarkey CE, Vrdoljak A, Moore AC, Gilbert SC (2013) Immunity against heterosubtypic influenza virus induced by adenovirus and MVA expressing nucleoprotein and matrix protein-1. Sci Rep 3:1443. doi:10.1038/srep01443
Lee YN, Youn HN, Kwon JH, Lee DH, Park JK, Yuk SS, Erdene-Ochir TO, Kim KT, Lee JB, Park SY, Choi IS, Song CS (2013) Sublingual administration of Lactobacillus rhamnosus affects respiratory immune responses and facilitates protection against influenza virus infection in mice. Antivir Res 98(2):284–290. doi:10.1016/j.antiviral.2013.03.013
Lei H, Peng X, Ouyang J, Zhao D, Jiao H, Shu H, Ge X (2015a) Intranasal immunization of recombinant Lactococcus lactis induces protection against H5N1 virus in ferrets. Virus Res 196:56–59. doi:10.1016/j.virusres.2014.11.009
Lei H, Peng X, Ouyang J, Zhao D, Jiao H, Shu H, Ge X (2015b) Protective immunity against influenza H5N1 virus challenge in chickens by oral administration of recombinant Lactococcus lactis expressing neuraminidase. BMC Vet Res 11:85. doi:10.1186/s12917-015-0399-4
Lei H, Peng X, Shu H, Zhao D (2015c) Intranasal immunization with live recombinant Lactococcus lactis combined with heat-labile toxin B subunit protects chickens from highly pathogenic avian influenza H5N1 virus. J Med Virol 87(1):39–44. doi:10.1002/jmv.23983
Li R, Chowdhury MY, Kim JH, Kim TH, Pathinayake P, Koo WS, Park ME, Yoon JE, Roh JB, Hong SP, Sung MH, Lee JS, Kim CJ (2015) Mucosally administered Lactobacillus surface-displayed influenza antigens (sM2 and HA2) with cholera toxin subunit A1 (CTA1) induce broadly protective immune responses against divergent influenza subtypes. Vet Microbiol 179(3–4):250–263. doi:10.1016/j.vetmic.2015.07.020
Liu M, Li X, Yuan H, Zhou J, Wu J, Bo H, Xia W, Xiong Y, Yang L, Gao R, Guo J, Huang W, Zhang Y, Zhao X, Zou X, Chen T, Wang D, Li Q, Wang S, Chen S, Hu M, Ni X, Gong T, Shi Y, Li J, Zhou J, Cai J, Xiao Z, Zhang W, Sun J, Li D, Wu G, Feng Z, Wang Y, Chen H, Shu Y (2015) Genetic diversity of avian influenza A (H10N8) virus in live poultry markets and its association with human infections in China. Sci Rep 5:7632. doi:10.1038/srep07632
Liu YY, Yang WT, Shi SH, Li YJ, Zhao L, Shi CW, Zhou FY, Jiang YL, Hu JT, Gu W, Yang GL, Wang CF (2016) Immunogenicity of recombinant Lactobacillus plantarum NC8 expressing goose parvovirus VP2 gene in BALB/c mice. J Vet Sci (in press)
Meijerink M, van Hemert S, Taverne N, Wels M, de Vos P, Bron PA, Savelkoul HF, van Bilsen J, Kleerebezem M, Wells JM (2010) Identification of genetic loci in Lactobacillus plantarum that modulate the immune response of dendritic cells using comparative genome hybridization. PLoS One 5(5):e10632. doi:10.1371/journal.pone.0010632
Mohamadzadeh M, Olson S, Kalina WV, Ruthel G, Demmin GL, Warfield KL, Bavari S, Klaenhammer TR (2005) Lactobacilli activate human dendritic cells that skew T cells toward T helper 1 polarization. PNAS 102(8):2880–2855. doi:10.1073/pnas.0500098102
Nakayama Y, Moriya T, Sakai F, Ikeda N, Shiozaki T, Hosoya T, Nakagawa H, Miyazaki T (2014) Oral administration of Lactobacillus gasseri SBT2055 is effective for preventing influenza in mice. Sci Rep 4:4638. doi:10.1038/srep04638
Nguyen TT, Mathiesen G, Fredriksen L, Kittl R, Nguyen TH, Eijsink VG, Haltrich D, Peterbauer CK (2011) A food-grade system for inducible gene expression in Lactobacillus plantarum using an alanine racemase-encoding selection marker. J Agric Food Chem 59(10):5617–5624. doi:10.1021/jf104755r
Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, Vyas JM, Boes M, Ploegh HL, Fox JG, Littman DR, Reinecker HC (2005) CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307(5707):254–258. doi:10.1126/science.1102901
Ou B, Yang Y, Tham WL, Chen L, Guo J, Zhu G (2016) Genetic engineering of probiotic Escherichia coli Nissle 1917 for clinical application. Applied microbiol biotechnol 100(20):8693–8699. doi:10.1007/s00253-016-7829-5
Petsch B, Schnee M, Vogel AB, Lange E, Hoffmann B, Voss D, Schlake T, Thess A, Kallen KJ, Stitz L, Kramps T (2012) Protective efficacy of in vitro synthesized, specific mRNA vaccines against influenza A virus infection. Nat Biotechnol 30(12):1210–1216. doi:10.1038/nbt.2436
Powell TJ, Peng Y, Berthoud TK, Blais ME, Lillie PJ, Hill AV, Rowland-Jones SL, McMichael AJ, Gilbert SC, Dong T (2013) Examination of influenza specific T cell responses after influenza virus challenge in individuals vaccinated with MVA-NP+M1 vaccine. PLoS One 8(5):e62778. doi:10.1371/journal.pone.0062778
Pu J, Wang S, Yin Y, Zhang G, Carter RA, Wang J, Xu G, Sun H, Wang M, Wen C, Wei Y, Wang D, Zhu B, Lemmon G, Jiao Y, Duan S, Wang Q, Du Q, Sun M, Bao J, Sun Y, Zhao J, Zhang H, Wu G, Liu J, Webster RG (2015) Evolution of the H9N2 influenza genotype that facilitated the genesis of the novel H7N9 virus. PNAS 112(2):548–553. doi:10.1073/pnas.1422456112
Schotsaert M, Ysenbaert T, Smet A, Schepens B, Vanderschaeghe D, Stegalkina S, Vogel TU, Callewaert N, Fiers W, Saelens X (2016) Long-lasting cross-protection against influenza A by neuraminidase and M2e-based immunization strategies. Sci Rep 6:24402. doi:10.1038/srep24402
Shi SH, Yang WT, Yang GL, Cong YL, Huang HB, Wang Q, Cai RP, Ye LP, Hu JT, Zhou JY, Wang CF, Li Y (2014) Immunoprotection against influenza virus H9N2 by the oral administration of recombinant Lactobacillus plantarum NC8 expressing hemagglutinin in BALB/c mice. Virology 464-465:166–1676. doi:10.1016/j.virol.2014.07.011
Shi SH, Yang WT, Yang GL, Zhang XK, Liu YY, Zhang LJ, Ye LP, Hu JT, Xing X, Qi C, Li Y, Wang CF (2016) Lactobacillus plantarum vaccine vector expressing hemagglutinin provides protection against H9N2 challenge infection. Virus Res 211:46–57. doi:10.1016/j.virusres.2015.09.005
Steidler L, Hans W, Schotte L, Neirynck S, Obermeier F, Falk W, Fiers W, Remaut E (2000) Treatment of murine colitis by Lactococcus lactis secreting interleukin-10. Science 289(5483):1352–1355
Steidler L, Neirynck S, Huyghebaert N, Snoeck V, Vermeire A, Goddeeris B, Cox E, Remon JP, Remaut E (2003) Biological containment of genetically modified Lactococcus lactis for intestinal delivery of human interleukin 10. Nat Biotechnol 21(7):785–789. doi:10.1038/nbt840
Sui Z, Chen Q, Fang F, Zheng M, Chen Z (2010) Cross-protection against influenza virus infection by intranasal administration of M1-based vaccine with chitosan as an adjuvant. Vaccine 28(48):7690–7698. doi:10.1016/j.vaccine.2010.09.019
Taniguchi M, Tokunaga T, Horiuchi K, Hoshino K, Sakai K, Tanaka T (2004) Production of L-lactic acid from a mixture of xylose and glucose by co-cultivation of lactic acid bacteria. Appl Microbio Biotechnol 66(2):160–165. doi:10.1007/s00253-004-1671-x
Tong S, Zhu X, Li Y, Shi M, Zhang J, Bourgeois M, Yang H, Chen X, Recuenco S, Gomez J, Chen LM, Johnson A, Tao Y, Dreyfus C, Yu W, McBride R, Carney PJ, Gilbert AT, Chang J, Guo Z, Davis CT, Paulson JC, Stevens J, Rupprecht CE, Holmes EC, Wilson IA, Donis RO (2013) New world bats harbor diverse influenza A viruses. PLoS Pathog 9(10):e1003657. doi:10.1371/journal.ppat.1003657
Wang H, Zhang Z, Chen Z, Zhang Y, Lv Q, An X, Tong Y, Carr MJ, Sun S, Shi W (2016) High genetic diversity and frequent genetic reassortment of avian influenza A(H9N2) viruses along the East Asian-Australian migratory flyway. Infect Genet Evol 39:325–329. doi:10.1016/j.meegid.2016.02.013
Wang Z, Yu Q, Gao J, Yang Q (2012) Mucosal and systemic immune responses induced by recombinant Lactobacillus spp. expressing the hemagglutinin of the avian influenza virus H5N1. Clin Vaccine Immunol 19(2):174–179. doi:10.1128/cvi.05618-11
Yang WT, Yang GL, Wang Q, Huang HB, Jiang YL, Shi CW, Wang JZ, Huang KY, Jin YB, Wang CF (2016a) Protective efficacy of Fc targeting conserved influenza virus M2e antigen expressed by Lactobacillus plantarum. Antivir Res 138:9–21. doi:10.1016/j.antiviral.2016.11.025
Yang WT, Shi SH, Yang GL, Jiang YL, Zhao L, Li Y, Wang CF (2016b) Cross-protective efficacy of dendritic cells targeting conserved influenza virus antigen expressed by Lactobacillus plantarum. Sci Rep 6:39665. doi:10.1038/srep39665
Zhang R, Chen T, Ou X, Liu R, Yang Y, Ye W, Chen J, Yao D, Sun B, Zhang X, Zhou J, Sun Y, Chen F, Wang SP (2016) Clinical, epidemiological and virological characteristics of the first detected human case of avian influenza A (H5N6) virus. Infect Genet Evol 40:236–2342. doi:10.1016/j.meegid.2016.03.010
Acknowledgments
This work was supported by the National High-Tech R&D Program of China (863 program) (2013AA102806), National Natural Science Foundation of China (31272541, 31272552, 31672528, 31602092), Science and Technology Development Program of Jilin Province (20160519011JH), Special Funds for Industrial Innovation of Jilin Province (2016C063) and the Doctoral Project sponsored by the Scientific Research Foundation of Jilin Agricultural University of China (201601).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests.
Ethical approval
All applicable international and national guidelines for the care and use of animals were followed.
Rights and permissions
About this article
Cite this article
Yang, WT., Yang, GL., Shi, SH. et al. Protection of chickens against H9N2 avian influenza virus challenge with recombinant Lactobacillus plantarum expressing conserved antigens. Appl Microbiol Biotechnol 101, 4593–4603 (2017). https://doi.org/10.1007/s00253-017-8230-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00253-017-8230-8