Abstract
Background
Magnetic resonance imaging (MRI) of the hips is being increasingly used to confirm hip reduction after surgery and spica cast placement for developmental dysplasia of the hip (DDH).
Objective
To review a single institutional experience with post-spica MRI in children undergoing closed or open hip reduction and describe the utility of MRI in directing the need for re-intervention.
Materials and methods
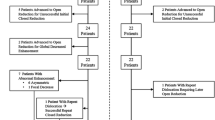
Seventy-four patients (52 female, 22 male) who underwent post-spica hip MRI over a 6-year period were retrospectively reviewed. One hundred and seven hips were included. Data reviewed included age at intervention, gender, type of intervention performed, MRI findings, the need for re-intervention and the interval between interventions. Gender was compared between the closed and open reduction groups via the Fisher exact test. Age at the first procedure was compared via the Wilcoxon rank test. Rates of re-intervention after closed and open reduction were calculated and the reasons for re-intervention were reviewed.
Results
The mean age at the time of the first intervention was 16.4 months (range: 4 to 63 months). Mean age for the closed reduction group was 10.5 months (range: 4–24 months) and for the open reduction group was 23.7 months (range: 5–63 months), which was significant (P-value <0.0001). Of the 52 hips that underwent closed reduction, 16 (31%) needed re-intervention. Of the 55 hips that underwent open reduction, MRI was useful in deciding re-intervention in only 1 (2%). This patient had prior multiple failed closed and open reductions at an outside institute.
Conclusion
Post intervention hip spica MRI is useful in determining the need for re-intervention after closed hip reduction, but its role after open reduction is questionable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developmental dysplasia of the hip (DDH) is related to the abnormal development of the acetabulum and positioning of the femoral head. It consists of a wide range of abnormalities from a hip that is normal on physical exam with a shallow acetabulum to an irreducible hip dislocation [1]. The goal of treatment in these cases is to achieve and maintain concentric reduction of the hip joint to promote congruent acetabular and femoral head development. Treatment is guided by the age at presentation and severity of the disease [1]. In general, at age 0–6 months, treatment usually involves an abduction orthotic device. At age 6–18 months, closed reduction is favored with or without an adductor tenotomy. At age 18 months and older, an open reduction may be necessary with or without a femoral shortening and de-rotation osteotomy and pelvic osteotomy.
After closed and open reduction, the concentric position of the femoral head in the acetabulum is confirmed with intraoperative arthrogram. This is followed by hip spica cast placement. The term spica cast refers to a cast of layers overlapping in a V pattern covering two body parts greatly different in size (the hip and waist in a hip spica cast) and resembling an ear of wheat or barley (spica=spike, ear of corn in Latin). Evaluating satisfactory reduction after cast placement is difficult radiographically, especially in the anteroposterior (AP) direction. MRI has become the preferred technique to evaluate the adequacy of reduction in this setting after reduction and spica placement [2,3,4,5]. If the MRI shows an abnormal position of the femoral head, re-intervention is performed to relocate the hip in the acetabulum. In some cases, re-intervention may be performed if there is evidence of decreased perfusion of the femoral head on post-contrast imaging, although the long-term implications of decreased perfusion in this scenario are unknown. Open reduction is indicated when a concentric closed reduction cannot be achieved or if it can only be achieved with the hip kept in extreme flexion, abduction or internal rotation [6].
The purpose of this study is to review a single institutional experience with post-spica MRI in children undergoing either closed or open hip reduction and describe the utility of MRI in directing re-intervention.
Materials and methods
This HIPAA-compliant retrospective study was approved by our institutional review board with waiver of informed consent. A search for all hip spica MRI studies at our institute between January 2011 and June 2016 was performed using the search function of our electronic reporting system. All MRI studies post spica that were performed on the same day after closed or open hip reduction were included. Patients undergoing MRI at a later date from intervention/surgery were excluded. Seventy-four patients with a total of 104 MRIs were identified. Thirty patients of the 74 patients had two MRIs. Fourteen patients had two MRIs sequentially for bilateral DDH, with each side undergoing reduction on a separate day. Sixteen patients had a second MRI when undergoing open reduction after an initial failed closed reduction. A total of 111 individual hips that underwent intervention were evaluated in these 104 MRIs. Seven patients had bilateral hip dislocation corrected at the same time and hence had only one immediate post-spica MRI. Fifty-six hips underwent closed reduction and 55 hips underwent open reduction. All patients with open reduction had osteotomy. All patients with closed reduction had intraoperative arthrograms. Using intraoperative arthrogram after open reduction was not universal and depends on surgeon preference at our institute.
All MRIs of the hips post spica in our department were performed on either an Ingenia 1.5-T, Achieva 1.5-T or Achieva 3-T (Philips, Best, The Netherlands) platform. Of 49 MRIs for 56 hips that underwent closed reduction, 5 MRIs (10%) included sedation. After open reduction, patients do not get any additional anesthesia with the MRI performed immediately following surgery. Our departmental protocol for MRI of the hips post spica includes coronal and axial proton-density (PD) sequences with fat saturation. After closed reduction, additional post-contrast coronal and axial T1-weighted images with fat saturation were performed to evaluate femoral head perfusion (Table 1). After open reduction, coronal and axial PD sequences are performed without fat saturation to avoid susceptibility artifact from implants related to subtrochanteric osteotomy interfering with optimal visualization of the hips.
Contrast material is not used after open reduction. The orthopedic surgeons order the study “without contrast” if open reduction is planned. Since the open reduction group did not receive intravenous contrast material and impaired perfusion was not a criterion for re-intervention in this group, we excluded cases in the closed reduction group that needed re-intervention based on abnormal perfusion of the femoral head to avoid this confounding variable. Of 56 hips that underwent closed reduction, 4 were excluded because re-intervention was due to impaired perfusion of femoral head and not related to abnormal positioning.
The hips were evaluated for concentric reduction by a pediatric radiologist (S.P.J.) with 10 years’ experience. Concentric reduction was defined as the femoral head directed to the triradiate cartilage with good anterior and posterior coverage, without asymmetrical joint space widening. The presence of subluxation or dislocation was noted. The radiologist was blinded to the original MRI report. It was not possible to blind the radiologist to the type of surgery (open or closed reduction) due to postoperative changes on the images indicating the type of surgery. Also, MRIs after closed and open reduction were “with” and “without” intravenous contrast material, respectively, further precluding blinding to the type of surgery. The findings were compared to the original MRI report. Although we traditionally report additional findings including the position and morphology of the labrum or the thickening of ligamentum teres at our institute, this does not affect management as long as the hip is concentrically reduced. The labrum was not evaluated for the purpose of this study.
The age of the patient at the first intervention, gender, the type of intervention performed, MRI findings, the need for re-intervention and the interval between the MRI and intervention were recorded in these cases. The reason for re-intervention in each case was also documented.
Statistical analysis
Percentages of females (or males) in the closed and open reduction groups were compared via the Fisher exact test. The age at the first procedure was compared via the Wilcoxon rank test. Re-interventions were analyzed based on each reduction as a unique event irrespective of prior procedures. Comparisons between closed and open reduction groups were performed via the Fisher exact test. The rates of re-intervention after closed and open reductions were calculated and reasons for re-intervention were reviewed. P<0.05 was defined as statistically significant.
Results
The patient cohort included 22 (30%) males and 52 (70%) females. Overall, the mean age at the time of first intervention was 16.4 months (range: 4 to 63 months). The mean age for the closed reduction group was 10.5 months (range: 4–24 months) and for the open reduction group was 23.7 months (range: 5–63 months). The difference was statistically significant (Table 2).
There was complete agreement regarding hip reduction between the MRI report and the blinded reviewer. Of the 52 hips undergoing closed reduction, 16 (31%) needed re-intervention. Eight (15%) of these were immediate re-interventions due to abnormal positioning of the femoral head on the post-spica hip MRI (Fig. 1) and 8 (15%) were delayed re-interventions (Table 3). In patients requiring immediate re-intervention due to abnormal positioning of the femoral head, none was suspected based on intraoperative imaging. Delayed re-interventions were those cases that had optimal reduction on the immediate post-spica MRI. Failed reduction was detected on routine follow-up radiograph evaluation in seven of these patients. In one patient, failed reduction was detected on a follow-up post-spica hip MRI obtained because of difficult surgery and the resultant increased risk for re-dislocation.
A 7-month old girl with developmental dysplasia of the hip post closed reduction with adductor tenotomy. Anteroposterior views of intraoperative arthrogram (a) and post-spica cast placement (b) shows satisfactory alignment. Coronal (c) and axial (d) proton density sequences with fat saturation show posterior dislocation of the unossified right femoral head
Of 55 hips that underwent open reduction, 3 (5%) needed re-intervention. In one case post-open reduction that required re-intervention, the lateral displacement of the femoral head was already demonstrated on the AP intraoperative radiograph after spica cast placement (Fig. 2). MRI confirmed what was already known on the intraoperative fluoroscopic images. The second case was a teratologic hip dislocation in which a failed reduction was known at surgery, but post-spica MRI was ordered to evaluate the hip anatomy. In these two patients, MRI was not necessary to diagnose the inadequate reduction and need for re-intervention. The third patient was a challenging case with two prior failed closed reductions and an additional failed open reduction at an outside institute. The intraoperative fluoroscopic images at the time of open reduction revision with femoral and pelvic osteotomies suggested that the hip was properly located, but the post-spica MRI revealed the hip to be posteriorly dislocated. The post-spica hip MRI led to re-intervention in only 1 case (2%) after open reduction, also in a challenging case with prior multiple failed reductions. The difference in an immediate re-intervention rate based on post-spica MRI after closed and open reductions was not statistically significant (Table 3), but it is clinically significant as noted above.
A 12-month-old girl with developmental dysplasia of the hip post open reduction with subtrochanteric osteotomy. Anteroposterior view after spica cast placement (a) shows lateral displacement of the unossified right femoral head when compared to the left. This is confirmed on the coronal proton density MRI (b)
Discussion
Our study demonstrated that if a surgeon elected to perform a closed reduction to treat DDH, post-spica MRI was more likely to play a role in identifying failed reduction and the need for re-intervention whereas in those patients who underwent an open reduction, post-spica MRI played little role other than confirming what the surgeon already knew operatively except in one challenging case.
MRI is increasingly becoming a routine imaging practice to confirm the postsurgical reduction of DDH due to its lack of ionizing radiation, superior soft-tissue delineation, multiplanar characterization of hip location and the ability for the study to be performed without additional sedation [7, 8]. MRI offers excellent visualization of soft tissue and cartilaginous structures, such as the capital femoral epiphysis, allowing accurate assessment of the adequacy of reduction regardless of the presence of an ossific nucleus [9]. The role of post-spica MRI is to identify potential failures of reduction or poor femoral head perfusion after closed reduction of DDH and this has been established in the literature in several prior studies [3, 4, 6, 10,11,12]. The long-term implications of poor femoral head perfusion after reduction are unknown. With a closed reduction, the hip often needs excessive abduction to maintain the reduction and the hip is under tension from surrounding soft-tissue structures, both of which are believed to predispose a patient to impaired perfusion of the femoral head. These factors are not an issue after an open reduction. At our institute, this is the primary reason for using intravenous contrast material only after a closed reduction and not after an open reduction. At our institution, MRI is being used to confirm postsurgical reduction after every open reduction as well. This has not been well described in the literature compared with the impact of post-spica MRI in the setting of closed reduction treatment of DDH. To our knowledge, there are no large studies evaluating how post-spica MRI impacts postoperative care of either closed or open reduction treatments of DDH.
We found a relatively large percentage of cases (31%) that underwent closed reduction requiring re-intervention compared with only 2% when open reduction was performed. Eight (50%) of the 16 closed reduction hips requiring re-intervention were well located on post-spica MRI and had delayed failed reduction needing re-intervention. There is better intraoperative control of femoral head and acetabular location in children who require open reduction, as well as the ease of fluoroscopically identifying the ossifying femoral head in older patients compared with the younger patients who underwent closed reduction. These two factors likely contributed to the low re-intervention rate in patients who underwent open reduction compared with those who underwent closed reduction. Therefore, the role of post-spica MRI remains critical in children who require closed reduction to treat DDH, but its role is questionable in those who undergo open treatment of DDH. With rising health care costs, utilization of imaging is under the scanner. Radiologists need to ensure optimal use of imaging that positively affects patient management. Our study raises doubts about the routine use of post-spica hip MRI after open reduction in DDH. This needs to be further evaluated with larger studies across institutions.
There are limitations to this study. One, this is a retrospective review in a single institute leading to selection bias. Two, this study focused on re-intervention related solely to incongruent femoral head position post spica, irrespective of the cause. We did not evaluate other factors including inversion of the labrum in well reduced hips, which may have surgical implications in some institutions.
Conclusion
Post-spica hip MRI is useful in determining the need for re-intervention after closed hip reduction, but its role after open reduction is questionable. Larger studies will be needed to evaluate this prior to changing practice patterns across institutions.
References
Nemeth BA, Narotam V (2012) Developmental dysplasia of the hip. Pediatr Rev 33:553–561
Johnson ND, Wood BP, Jackman KV (1998) Complex infantile and congenital hip dislocation: assessment with MR imaging. Radiology 168:151–156
Bos C, Bloem J (1989) Treatment of dislocation of the hip, detected in early childhood, based on magnetic resonance imaging. J Bone Joint Surg Am 71-A:1523–1529
Jaramillo D, Villegas-Medina OL, Doty DK et al (1996) Gadolinium-enhanced MR imaging demonstrates abduction-caused hip ischemia and its reversal in piglets. AJR Am J Roentgenol 166:879–887
Jaremko JL, Wang CC, Dulai S (2014) Reliability of indices measured on infant hip MRI at time of spica cast application for dysplasia. Hip Int 24:405–416
Bulut M, Gurger M, Belhan O et al (2013) Management of developmental dysplasia of the hip in less than 24 months old children. Indian J Orthop 47:578–584
Desai AA, Martus JE, Schoenecker J, Kan JH (2011) Spica MRI after closed reduction for developmental dysplasia of the hip. Pediatr Radiol 41:525–529
Rosenbaum DG, Servaes S, Bogner EA et al (2016) MR imaging in postreduction assessment of developmental dysplasia of the hip: goals and obstacles. Radiographics 36:840–854
Duffy CM, Taylor FN, Coleman L et al (2002) Magnetic resonance imaging evaluation of surgical management in developmental dysplasia of the hip in childhood. J Pediatr Orthop 22:92–100
Jaramillo D, Villegas-Medina O, Laor T et al (1998) Gadolinium enhanced MR imaging of pediatric patients after reduction of dysplastic hips: assessment of femoral head position, factors impeding reduction, and femoral head ischemia. AJR Am J Roentgenol 170:1633–1637
Tiderius C, Jaramillo D, Connolly S et al (2009) Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report. J Pediatr Orthop 29:14–20
Laor T, Roy DR, Mehlman CT (2000) Limited magnetic resonance imaging examination after surgical reduction of developmental dysplasia of the hip. J Pediatr Orthop 20:572–574
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. J. Herman Kan has received royalties from Elsevier and Springer and a stipend from the National Institutes of Health as a grant reviewer.
Rights and permissions
About this article
Cite this article
Jadhav, S.P., More, S.R., Shenava, V. et al. Utility of immediate postoperative hip MRI in developmental hip dysplasia: closed vs. open reduction. Pediatr Radiol 48, 1096–1100 (2018). https://doi.org/10.1007/s00247-018-4143-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4143-7