Abstract
Background
Due to fluctuations in contemporary trends for breast reconstruction, we aimed to perform a comparative analysis to assess postoperative outcomes and complications of immediate implant-based breast reconstruction (IBBR) with tissue expander before and over the course of the COVID-19 pandemic.
Methods
Consecutive adult women undergoing total mastectomy and immediate two-stage IBBR with tissue expanders between September 2018 and May 2021 were included. Two groups were compared: reconstructions performed before COVID-19 (pre-pandemic) and reconstructions performed after the implementation of the COVID-19 policies at our institution. We compared postoperative complications and perioperative outcomes (e.g., length of stay, expander volume, time for definitive implant) between groups.
Results
One hundred fourteen patients representing 192 reconstructions with expanders were included. One-hundred twenty-eight (66.6%) were performed before the COVID-19 pandemic, while 64 (33.3%) were performed during the pandemic. A larger proportion of reconstructions performed during the pre-pandemic era had a prolonged length of stay (≥ 2 days) compared to reconstructions performed during the COVID-19 pandemic (43% versus 9.4%, p < .001). The median time from immediate IBBR to initiate outpatient expansions (22 days [IQR, 15–34]; p = 0.45) and to conclude outpatient expansion was (52 days [IQR, 40–76]; p = 0.85) comparable between groups. The rates of 30-day complications and rates of complications during the expansion period were similar between groups.
Conclusion
Due to adjustments in perioperative management and the implementation of institutional and state recommendations, IBBR with tissue expander during the COVID-19 pandemic exhibited a reduced length of stay compared to pre-pandemic reconstructions without increased morbidity.
Level of evidence: Level IV, Risk/Prognostic
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2020, the COVID-19 pandemic led to a unique disruption in healthcare services and surgical treatment for women diagnosed with breast cancer in the United States and the world [1]. While COVID-19 was announced as a worldwide pandemic by the World Health Organization (WHO), the American College of Surgeons (ACS) issued a series of clinical directives advising the postponement of non-essential surgeries to safeguard the health of patients and healthcare providers, as well as to preserve hospital resources [1, 2].
Breast cancer treatment recommendations were frequently updated in response to the increasing COVID-19 infection rates [1]. During the initial phase of the pandemic, when hospital resources and staff were restricted, a special communication regarding the treatment of breast cancer suggested that suitable patients should proceed with breast-conserving therapy (BCT) instead of mastectomy [1, 3]. For patients who required total mastectomy, reconstructive surgery could be performed if hospital resources permitted [3]. Furthermore, the guidelines of the COVID-19 Pandemic Breast Cancer Consortium limited breast reconstruction to alloplastic procedures only, while postponing autologous reconstruction [3]. These circumspect recommendations were based on the uncertain hazards that COVID-19 posed to cancer patients and emerged from well-thought-out tactics to enhance the provision of surgical care [4, 5]. In this setting, immediate breast reconstruction presented a distinctive surgical difficulty, as it combined the exigency of surgical oncology (the mastectomy) with both a functional and an aesthetic component (the reconstruction) that could be compromised for the sake of patient safety [6, 7].
A recent study evaluating the effects of COVID‐19 on mastectomy and breast reconstruction using the National Surgical Quality Improvement Program (NSQIP) database revealed a significant decline in direct-to-implant reconstruction (20.7% to 18.2%) and an upsurge in tissue expander reconstruction (64.0% to 68.4%) from 2019 to 2020 [1]. Due to these fluctuations in contemporary trends for breast reconstruction, we aimed to perform a comparative analysis to assess postoperative outcomes and complications of immediate implant-based breast reconstruction (IBBR) with tissue expander before and over the course of the COVID-19 pandemic.
Our alternative hypothesis (H1) posited that immediate reconstructions during the COVID-19 pandemic would result in a shorter hospital stay but a longer time to initiate and complete outpatient expansions compared to reconstructions performed during the pre-pandemic era. Additionally, we hypothesized that reconstructions carried out during the COVID-19 pandemic would exhibit a higher rate of complications.
Methods and patients
Institutional Review Board approval at a single large medical center was obtained for this study and a retrospective review of medical records was conducted. Consent was obtained from patients. Consecutive adult women undergoing total mastectomy and immediate two-stage IBBR with tissue expanders between September 2018 and May 2021 were included. Reconstructions performed with direct-to-implant approach, autologous tissue at the time of expander placement (e.g., latissimus dorsi-assisted reconstruction), or delayed device placement were excluded from our study. Patients with metastatic disease or who expressed the desire for autologous reconstruction after tissue expander were excluded (delayed-immediate autologous reconstruction).
In collaboration with the Monroe County Health Department, the New York State Department of Health, and the Center for Disease Control and Prevention (CDC), the University of Rochester Medical Center established a response to the global COVID-19 outbreak. On February 29th, 2020, at 03:26 AM, a comprehensive policy was provided that outlined procedures concerning the triage, diagnosis, and isolation of suspected COVID-19 patients, and guidance to be used by providers and staff who provided care to or encountered these patients. Patients were extensively counseled about the risk of COVID-19 infection and the different surgical techniques available for breast reconstruction [8]. Two groups were compared: reconstructions performed before COVID-19 (pre-pandemic) and reconstructions performed after the implementation of the COVID-19 policy at our institution.
Patients undergoing mastectomy were offered consultation with plastic surgeons and they were evaluated to determine if they were adequate candidates for reconstruction [9]. The surgical technique for IBBR with expanders has been reported in our previous articles [10,11,12,13,14]. The type of mastectomy (nipple- or skin-sparing) and the decision to perform sentinel lymph node biopsy (SLNB) or axillary lymph node dissection (ALND) depended on the surgical oncologist. The type of incision pattern, regional anesthesia blocks, use of fluorescence imaging for perfusion assessment, incorporation of acellular dermal matrix (ADM) products, number of drains, plane for tissue expander placement, intraoperative volume of the expander, type of filling of the expander (saline/air), and time to start outpatient expansions depended on the reconstructive surgeon’s preference. Drains were removed when output was less than 30-cc over 24 h for 2 consecutive days.
Study variables
We extracted data on the demographic information, comorbidities, American Society of Anesthesiologists (ASA) status, preoperative hematocrit, time of follow-up, indication for surgery, diagnosis and staging of the oncologic disease, neoadjuvant or adjuvant systematic chemotherapy and radiotherapy, type of mastectomy, laterality of the procedure (bilateral/unilateral), incision pattern [15], axillary surgery for cancer staging, weight of mastectomy specimen, surface of tissue expanders or implants, plane of reconstruction (prepectoral/subpectoral) [12], use of ADM or autoderm (inferiorly based dermal flap), filling of tissue expanders (air/saline) [16], and number of drains. Surgical outcomes included the length of stay, estimated blood loss, tissue expander initial intraoperative volume, time to initiate and finish outpatient expansions, final tissue expander volume, and time for expander-to-implant exchange. Data on the size of the definitive implant, procedures for capsule revision during exchange, and fat grafting during exchange or after exchange were also collected.
Relevant complications analyzed in this study included hematoma, return to the operating room (RTOR) for evacuation of hematoma, seroma, periprosthetic infection, infection-related unplanned procedures, wound disruption (e.g., mastectomy flap necrosis, dehiscence), wound disruption-related unplanned interventions (debridement or excision, or device explantation), expander leak, prosthesis displacement, fat necrosis, implant rupture, use of latissimus dorsi flap for reconstruction salvage, and capsular contracture.
Statistical analysis
Each reconstruction was considered an independent research subject for analysis. Thus, a single patient could contribute two sets of data in bilateral cases. Normality was assessed with the Shapiro–Wilk test. Continuous data were analyzed with the t-test or Mann–Whitney test. Normally distributed data were presented as mean ± standard deviation, while non-normal data were presented as median and interquartile range [IQR]. Fisher’s exact test was used to analyze categorical data. Categorical data were presented as frequency and percentage. A p-value < 0.05 was determined to be statistically significant.
Binomial logistic regression analysis was conducted to assess predictors associated with prolonged length of stay (≥ 2 days). Patient-related, oncologic, and surgical variables associated with prolonged length of stay on univariable analysis were incorporated into a multivariable logistic regression model to determine which factors were independent predictors of prolonged length of stay. Goodness-of-fit of the multivariable regression model was estimated with the area under the receiver operating characteristic (ROC) curve. An area under the curve greater than 0.6 implied an acceptable performance of the regression. Statistical analysis was performed using R statistical software, version 4.0.0 (R Core Team, 2020) [17].
Results
Characteristics of subjects
One hundred fourteen patients representing 192 reconstructions with expanders were included (Table 1). One-hundred twenty-eight (66.6%) were performed before the COVID-19 pandemic, while 64 (33.3%) were performed during the pandemic. The average age between groups was similar (52.8 years versus 52.094 years, p = 0.68). Most reconstructions were performed in White/Caucasian (75%) and Black/African American patients (18.8%, p = 0.22). A similar proportion of reconstructions were performed in obese patients in the pre-pandemic group and COVID-19 group (25% versus 39.1%, p = 0.064). The proportions of reconstructions performed in former smokers (35.9% versus 39.1%) and current smokers (3.1% versus 0%, p = 0.46) were comparable between groups.
The rates of different comorbidities among patients were similar between cohorts showing no statistical significance. A higher proportion of reconstructions in the COVID-19 group were performed in patients ASA 3 (39.1% versus 22.7%) and ASA 4 (1.6% versus 0%, p = 0.034) compared to reconstructions in the pre-pandemic group. Due to the inherent temporal consideration of the study methodology, a lengthier follow-up was present in the pre-pandemic group compared to the COVID-19 group (30.262 months versus 15.852 months, p < 0.001).
Oncologic data
Oncologic data on diagnosis and staging are reported in Table 2. The rate of pre-mastectomy radiotherapy was similar between groups (2.3% versus 0.0%, p = 0.55). Nonetheless, the rate of reconstructions performed in patients receiving neoadjuvant chemotherapy was significantly higher during the COVID-19 pandemic group compared to the pre-pandemic period (31.3% versus 11.7%, p = 0.001). The rate of reconstructions that received adjuvant radiotherapy was similar between groups (14.1% versus 16.4%, p = 0.83). Likewise, the rate of reconstructions performed in patients receiving adjuvant chemotherapy was also comparable between groups (21.9% versus 21.1%, p = 1.00).
Surgical characteristics
Most reconstructions were performed as bilateral procedures (79.7% versus 83.6%, p = 0.549) and were performed following skin-sparing mastectomy (87.5% versus 76.6%, p = 0.085). Near half of the reconstructions were performed with concomitant nerve blocks (pre-pandemic, 57.8; COVID-19, 56.3%; p = 0.88). A larger proportion of reconstructions performed during the COVID-19 pandemic had a wise pattern for mastectomy incisions (42.2% versus 23.4%, p < 0.001). A similar proportion of reconstructions had SLNBs in the pre-pandemic group (44.5%) compared to the COVID-19 group (43.8%). Similarly, the proportion of cases that had ALND were comparable between the pre-pandemic and COVID-19 group (7% versus 10.9%, p = 0.64) (Table 3).
Fluorescence imaging for mastectomy flap perfusion assessment was conducted in a similar proportion of cases in the pre-pandemic and COVID-19 group (70.3% versus 76.6%, p = 0.39). A larger proportion of reconstructions performed in the COVID-19 group received smooth tissue expanders compared to reconstruction in the pre-pandemic group (100% versus 68.8%, p < 0.001). Also, a larger proportion of tissue expanders were placed in the prepectoral plane in the COVID-19 group compared to the pre-pandemic group (73.4% versus 49.2%, p = 0.001). ADMs were used to a greater extent during the COVID-19 pandemic (100% versus 89.8%, p = 0.005).
Surgical outcomes
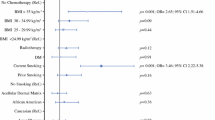
The median estimated blood loss was higher in reconstructions performed during the COVID-19 pandemic (175 ml [IQR, 100–232.5] versus 150 ml [IQR, 100–200]; p = 0.047). A larger proportion of reconstructions performed during the pre-pandemic era had a prolonged length of stay (≥ 2 days) compared to reconstructions performed during the COVID-19 pandemic (43% versus 9.4%, p < 0.001) (Fig. 1). The median volume for intraoperative filling of the tissue expanders was comparable between groups (240 ml versus 250 ml; p = 0.958) (Table 4). The median time from immediate breast reconstruction to start outpatient expansions was also similar between groups (22 days versus 23 days; p = 0.45). The median time for drain removal was lengthier in the pre-pandemic group compared to the COVID-19 group (13.5 days [IQR, 11–17] versus 12.5 days [IQR, 8–15]; p = 0.005). The median time from tissue expander placement to the last outpatient expansion was 52 days (IQR, 40–76; p = 0.85), while the median time for TE-to-implant exchange was 147 days (IQR, 104.5–203; p = 0.249).
Comparison for length of stay, time for drain removal, time for first outpatient expansion, and time to finish outpatient expansions between groups. Each box represents the 25th to 75th percentile for duration or time in days. The error bars represent the shortest and longest operative time associated with each box plot
Multivariable analysis
We evaluated the factors associated with prolonged length of stay after immediate breast reconstruction with expanders (≥ 2 days) (Supplemental Material 1). On univariable analysis, older age (OR 0.969, p = 0.027), reconstructions performed during COVID-19 (OR 0.137, p < 0.001), and using ADMs (OR 0.031, p = 0.001) were associated with reduced odds of prolonged length of stay. On the other hand, reconstructions performed in Black/African American versus White/Caucasians (OR 3.0, p = 0.004) or other races/ethnicities versus White/Caucasians (OR 4.2, p = 0.019), bilateral versus unilateral reconstructions (OR 3.18, p = 0.0237), larger mastectomy specimen weights (OR 1.001, p = 0.008), increased volume of estimated blood loss (OR 1.004, p = 0.017), and using textured versus smooth tissue expanders (OR 3.541, p < 0.001) were associated with increased odds of prolonged length of stay.
On multivariable analysis, a large volume of estimated blood loss (OR 1.005, 95%CI 1.001 to 1.008; p = 0.006) was independently associated with prolonged length of stay. Conversely, using ADMs (OR 0.051, 95%CI 0.006 to 0.462; p = 0.008) or performing reconstruction during COVID-19 versus pre-pandemic era (OR 0.138, 95%CI 0.048 to 0.394; p = 0.0002) were independently associated with reduced odds of prolonged length of stay (Table 5). The area under the curve was estimated to be 0.808 for the regression model (Fig. 2).
Tissue expander complications
The overall 30-day morbidity and the rates of all 30-day complications following immediate tissue expander placement were similar between groups (Table 6). Even after adjusting for several possible confounders, the impact of the COVID-19 pandemic on the rate of 30-day complications was not significant (Supplemental Material 2). The rates of all complications evaluated during the whole period of tissue expansion were comparable between groups (Table 7). The rates of seroma (25.8% versus 18.8%, p = 0.36), hematoma (7% versus 4.7%, p = 6.3%), periprosthetic infection (14.8% versus 12.5%, p = 0.82), fat necrosis (1.6% versus 0.0%, p = 0.55), wound disruption (18% versus 17.2%, p = 1.00), unplanned debridement procedure for wound disruption (10.9% versus 10.9%, p = 1.00), capsular contracture (2.3% versus 1.6%, p = 1.00), use of latissimus dorsi flap for reconstruction salvage (4.7% versus 0.0%, p = 0.18), and abandonment of IBBR (5.5% versus 7.8%, p = 0.53) were similar between groups.
Tissue expander-to-implant exchange
At the time of chart review, one-hundred twenty reconstructions of the pre-pandemic group and fifty-nine of the COVID-19 group successfully underwent tissue expander-to-implant exchange (Table 8). The rates of reconstructions that underwent capsulotomy (66.7% versus 47.5%), partial capsulectomy (8.3% versus 11.9%), and total capsulectomy (1.7% versus 0.0%, p = 0.39) at the time of exchange were comparable between the pre-pandemic and COVID-19 group. The mean size of the definitive implant was 515.5 ± 140.3 cc in the pre-pandemic group, and 520.4 ± 141.8 cc in the COVID-19 group (p = 0.82). Most definitive implants had a smooth surface (98.3% versus 100%, p = 1.00). Simultaneous fat grafting at the time of exchange was performed in almost half of the reconstructions (57.5% versus 54.2%, p = 0.749). The volume of autologous fat simultaneously injected during exchange was similar between groups (90 ml [IQR, 70–115] versus 108.5 ml [IQR, 57.5–121.25]; p = 0.91).
Fat grafting after exchange was performed in 15.6% of the reconstructions (p = 0.62). Most had one session of fat grafting (14.5%) while only 1.1% of the cases had two sessions of fat grafting. The median volume of autologous fat delivered after expander-to-implant exchange was similar between the pre-pandemic and COVID-19 group (122.7 ± 71 versus 122.9 ± 61, p = 0.993). Finally, the rates of all complications evaluated after exchanging the expanders for definitive implants were similar between groups (Supplemental Material 3).
Discussion
The objective of this research study was to assess the extent to which the COVID-19 pandemic affected breast cancer surgical treatment and immediate reconstruction with tissue expanders at a particular institution in New York State [18]. Our study demonstrated that IBBR during the COVID-19 pandemic exhibited comparable 30-day morbidity and a similar overall rate of complications compared to data from the pre-pandemic era. Due to the implementation of different policies to preserve healthcare resources for hospitalized patients and to limit both patient and surgical team risk of virus transmission, we found a significant reduction in the length of stay following immediate IBBR during the COVID-19 pandemic compared to the pre-pandemic era. As opposed to our initial hypothesis or expected outcome, the time to initiate outpatient expansions and the time to conclude the expansion process were not affected by COVID-19.
Although the duration of hospitalization after surgery in the U.S. has been decreasing gradually since 2008, the COVID-19 pandemic led to the prioritization of outpatient procedures [19]. This shift towards outpatient procedures has been further reinforced due to the need for operation triage during the pandemic [18, 20]. The effects of COVID-19 on plastic surgery and breast reconstruction have been noteworthy [20, 21]. In this study, we achieved to significantly reduce the length of stay during the COVID-19 pandemic without increasing the overall 30-day morbidity or the rates of complications during the time expanders remained in the mastectomy pockets. Similar to our outcomes, other reports have supported the idea of reducing the length of stay after immediate IBBR without increasing perioperative morbidity [5, 19]. A recent study using NSQIP data from 2007 through 2019, the authors demonstrated no difference in overall 30-day postoperative complication rates between patients who had same-day surgery discharge (< 24 h) with IBBR compared to patients who had non-same-day surgery discharge [19].
We investigated several predictors for prolonged length of stay on multivariable analysis. Although several reports have suggested regional anesthesia blocks may expedite patient discharge and reduce length of stay following IBBR [22, 23], we did not find an association between regional anesthesia blocks and a reduced length of stay, as it was also demonstrated in a recent study by Chow et al.[19] On the other hand, on multivariable analysis, we demonstrated that performing IBBR during the COVID-19 was determined to be an independent predictor associated with early patient discharge.
Several studies have established strong associations between increased morbidity following elective procedures and infection by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [24,25,26,27]. On this matter, our study presents proof that performing immediate two-stage prosthetic breast reconstruction with expanders is both practical and secure even in the midst of the COVID-19 pandemic. Similar to the studies presented by other authors [28], we experienced a similar complication rate following IBBR between the pre-pandemic and COVID-19 group.
There are few case reports demonstrating the incidence of late seromas following COVID-19 infection, [29,30,31] or the incidence of potential localized and systemic reactions in implant carriers after receiving a COVID-19 vaccine [31]. The temporal relationship between the occurrence of breast-related complications and infection with SARS-CoV-2, seroconversion, or administration of vaccines is still yet to be further evaluated in prospective studies. Of note, the implementation of a direct-to-implant approach may avoid postoperative visits and requirements of an exchange procedure in selected patients; hence, reducing patient exposure to healthcare institutions and reducing risk of COVID-19 infection [32].
Limitations
The retrospective design of this study and the use of institutional databases for mastectomy data limited its scope. Mistakes in Current Procedural Terminology (CPT®) coding may affect the number of cases observed. Additionally, the study is based on the experience of a single institution and its findings may lack external validity. This study did not evaluate short-term oncologic outcomes since there wasn't enough time to follow-up on these patients. Likewise, due to the temporal feature of the SARS-CoV-2, the pre-pandemic group had a lengthier follow-up compared to the COVID-19 group. Due to limitations regarding the acquisition of data, the effect of immunological factors (e.g., seroconversion after SARS-CoV-2 infection, fluctuations in C-reactive protein levels) on the rate of complications was not evaluated.
Conclusions
Our study presents proof that performing immediate IBBR with tissue expanders is both practical and secure amid the COVID-19 pandemic. Due to the adjustment in perioperative management and the implementation of institutional and state recommendations, IBBR with tissue expander during the COVID-19 pandemic exhibited a reduced length of stay compared to pre-pandemic reconstructions.
Data Availability
Raw data were generated at the URMC. Derived data supporting the findings of this study are available from the corresponding author O.J.M. on request.
References
Rubenstein RN, Stern CS, Plotsker EL et al (2022) Effects of COVID-19 on mastectomy and breast reconstruction rates: a national surgical sample. J Surg Oncol 126(2):205–213. https://doi.org/10.1002/jso.26889
Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Biomed 91(1):157–160. https://doi.org/10.23750/abm.v91i1.9397
Dietz JR, Moran MS, Isakoff SJ et al (2020) Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat 181(3):487–497. https://doi.org/10.1007/s10549-020-05644-z
Brindle ME, Gawande A (2020) Managing COVID-19 in surgical systems. Ann Surg 272(1):e1–e2. https://doi.org/10.1097/SLA.0000000000003923
Keane AM, Keane GC, Skolnick GB et al (2023) Immediate post-mastectomy implant-based breast reconstruction: an outpatient procedure? Plast Reconstr Surg 152(1):1e–11e. https://doi.org/10.1097/PRS.0000000000010156
Jallali N, Hunter JE, Henry FP et al (2020) The feasibility and safety of immediate breast reconstruction in the COVID-19 era. J Plast Reconstr Aesthet Surg 73(11):1917–1923. https://doi.org/10.1016/j.bjps.2020.08.044
Escandón JM, Nazerali R, Ciudad P et al (2022) Minimally invasive harvest of the latissimus dorsi flap for breast reconstruction: a systematic review. Int J Med Robot 18(6):e2446. https://doi.org/10.1002/rcs.2446
Bracaglia R, D’Ettorre M, Gentileschi S, Tambasco D (2014) Was the surgeon a satisfactory informant? How to minimize room for claims. Aesthetic Surg J 34(4):632–635. https://doi.org/10.1177/1090820X14528504
Gentileschi S, Caretto AA, Tagliaferri L, Salgarello M, Peris K (2020) Skin cancer plastic surgery during the COVID-19 pandemic. Eur J Surg Oncol 46(6):1194–1195. https://doi.org/10.1016/j.ejso.2020.04.048
Sbitany H, Sandeen SN, Amalfi AN, Davenport MS, Langstein HN (2009) Acellular dermis-assisted prosthetic breast reconstruction versus complete submuscular coverage: a head-to-head comparison of outcomes. Plast Reconstr Surg 124(6):1735–1740
Escandón JM, Ali-Khan S, Christiano JG et al (2022) Simultaneous fat grafting during tissue expander-to-implant exchange: a propensity score-matched analysis. Aesthetic Plast Surg. https://doi.org/10.1007/s00266-022-03152-7
Escandón JM, Sweitzer K, Christiano JG et al (2022) Subpectoral versus prepectoral two-stage breast reconstruction: a propensity score-matched analysis of 30-day morbidity and long-term outcomes. J Plast Reconstr Aesthetic Surg 76:76–87. https://doi.org/10.1016/j.bjps.2022.10.028
Calderon T, Skibba KE, Hansen T, Amalfi A, Chen E (2022) Safety of breast reconstruction using inferiorly based dermal flap for the ptotic breast. Ann Plast Surg 88(3 Suppl 3):S156–S162. https://doi.org/10.1097/SAP.0000000000003177
Sweitzer K, Patel AU, Wingate NA, Milek D, Escandon J, Christiano JG (2023) Outpatient model for reduced utilization of narcotics following breast reduction. J Plast Reconstr Aesthet Surg 77:18–20. https://doi.org/10.1016/j.bjps.2022.11.065
Lotan AM, Tongson KC, Police AM, Dec W (2020) Mastectomy incision design to optimize aesthetic outcomes in breast reconstruction. Plast Reconstr Surg - Glob Open 8(9):e3086. https://doi.org/10.1097/GOX.0000000000003086
Escandón JM, Milek D, Christiano JG, Chen E, Langstein HN, Manrique OJ (2022) Impact of intraoperative expansion with air and outcomes in first stage implant-based breast reconstruction: a propensity-matched analysis. Plast Reconstr Surg Glob Open 10(10 Suppl):89. https://doi.org/10.1097/01.GOX.0000898776.63214.ea
R Core Development Team. R Core Team (2021) R: a language and environment for statistical computing. (Version 4.0) [Computer Software]. Retrieved from https://cran.r-project.org/. Published online 2021. https://cran.r-project.org
Hemal K, Boyd CJ, Bekisz JM, Salibian AA, Choi M, Karp NS (2021) Breast reconstruction during the COVID-19 pandemic: a systematic review. Plast Reconstr Surgery Glob Open 9(9):e3852. https://doi.org/10.1097/GOX.0000000000003852
Chow AL, Luthringer MM, Van Kouwenberg EA, Agag RL, Sinkin JC (2023) Same-day mastectomy and immediate prosthetic breast reconstruction: a twelve-year analysis of a national database and early postoperative outcomes. Plast Reconstr Surg. https://doi.org/10.1097/PRS.0000000000010348
Sun P, Luan F, Xu D, Cao R, Cai X (2021) Breast reconstruction during the COVID-19 pandemic: a systematic review. Medicine (Baltimore) 100(33):e26978. https://doi.org/10.1097/MD.0000000000026978
Chi D, Chen AD, Dorante MI, Lee BT, Sacks JM (2021) Plastic surgery in the time of COVID-19. J Reconstr Microsurg 37(2):124–131. https://doi.org/10.1055/s-0040-1714378
Tokita HK, Polanco TO, Shamsunder MG et al (2019) Non-narcotic perioperative pain management in prosthetic breast reconstruction during an opioid crisis: a systematic review of paravertebral blocks. Plast Reconstr Surgery Glob Open 7(6):e2299. https://doi.org/10.1097/GOX.0000000000002299
Shah A, Rowlands M, Krishnan N, Patel A, Ott-Young A (2015) Thoracic intercostal nerve blocks reduce opioid consumption and length of stay in patients undergoing implant-based breast reconstruction. Plast Reconstr Surg 136(5):584e–591e. https://doi.org/10.1097/PRS.0000000000001717
Deng JZ, Chan JS, Potter AL et al (2022) The risk of postoperative complications after major elective surgery in active or resolved COVID-19 in the United States. Ann Surg 275(2):242–246. https://doi.org/10.1097/SLA.0000000000005308
Gupta S, Goil P, Mohammad A, Escandón JM (2022) Mucormycosis management in COVID-19 Era: is immediate surgical debridement and reconstruction the answer? Arch Plast Surg 49(3):397–404. https://doi.org/10.1055/s-0042-1748654
Gulinac M, Novakov IP, Antovic S, Velikova T (2021) Surgical complications in COVID-19 patients in the setting of moderate to severe disease. World J Gastrointest Surg 13(8):788–795. https://doi.org/10.4240/wjgs.v13.i8.788
Prasad NK, Lake R, Englum BR et al (2022) Increased complications in patients who test COVID-19 positive after elective surgery and implications for pre and postoperative screening. Am J Surg 223(2):380–387. https://doi.org/10.1016/j.amjsurg.2021.04.005
Faulkner HR, Coopey SB, Liao EC, Specht M, Smith BL, Colwell AS (2022) The safety of performing breast reconstruction during the COVID-19 pandemic. Breast Cancer 29(2):242–246. https://doi.org/10.1007/s12282-021-01304-2
Chan SLS, Mok JWL (2022) Late seroma in breast implants: a Coronavirus disease 2019 phenomenon? Arch Plast Surg 49(5):611–613. https://doi.org/10.1055/s-0042-1756295
Martínez Núñez P, Pérez González M, Juárez CÁ (2022) Late seroma of the breast in association with COVID-19 infection: two case reports. Eur J Plast Surg 45(4):671–674. https://doi.org/10.1007/s00238-021-01898-y
Weitgasser L, Mahrhofer M, Schoeller T (2021) Potential immune response to breast implants after immunization with COVID-19 vaccines. Breast 59:76–78. https://doi.org/10.1016/j.breast.2021.06.002
Gentileschi S, Bracaglia R, Garganese G et al (2013) Immediate definitive prosthetic reconstruction in patients with ptotic breasts. Ann Plast Surg 70(2):144–148. https://doi.org/10.1097/SAP.0b013e3182367bfd
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The local ethics committee approved this study (IRB#: STUDY00006499).
Conflict of Interest
The authors have no conflict of interests or commercial associations to disclose related to this study.
Patient Consent Statement
Written informed consent for publication of their details was obtained from the patient/study participant/parent/guardian/next of kin.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presentation
This article has not been presented in a national or international meeting.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Escandón, J.M., Aristizábal, A., Langstein, H.N. et al. Immediate two-stage implant-based breast reconstruction during the COVID-19 pandemic: retrospective single center study. Eur J Plast Surg 46, 1081–1092 (2023). https://doi.org/10.1007/s00238-023-02115-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02115-8