Abstract
Background
Delayed wound healing or infection leads to premature tissue expander (TE) explantation after immediate postmastectomy breast reconstruction. A large study with sufficient duration of follow-up focusing on the impact of chemotherapy (CT) on premature TE removal after immediate breast reconstruction is lacking.
Methods
A retrospective review of patients undergoing immediate TE reconstruction was conducted. Multivariate analyses identified factors contributing to premature removal of TEs including neoadjuvant and adjuvant CT, specific chemotherapeutic regimens, and other factors like cancer stage, body mass index, smoking, radiation, and age. Kaplan–Meier curves were plotted to study the timing of premature TE removal.
Results
Of 899 patients with TEs, 256 received no, 295 neoadjuvant, and 348 adjuvant CT. Premature removal occurred more frequently in the neoadjuvant (17.3 %) and adjuvant (19.9 %) cohorts than the no-CT (12.5 %) cohort (p = 0.056). Premature TE removal occurred earlier (p = 0.005) in patients who received no CT than those with adjuvant CT. Radiation in patients receiving neoadjuvant CT prolonged the mean time to premature removal (p = 0.003). In the absence of radiation, premature removal occurred significantly sooner with neoadjuvant than adjuvant CT (p = 0.035).
Discussion
Premature removal of a TE occurs more commonly in patients treated with neoadjuvant or adjuvant CT and is most commonly observed 2–3 months after placement—well after the follow-up period recorded by the American College of Surgeons National Surgery Quality Improvement Program (NSQIP) database. These findings can be used to aid preoperative counseling and guide the timing of follow-up for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The majority of postmastectomy breast reconstructions begin with placement of a TE that is later exchanged for a breast implant (TE/I), or in some cases an autologous flap.1,2 TE complications, which occur more commonly in the presence of risk factors like elevated body mass index (BMI) and radiation, and to a lesser extent, smoking and age, include infection, explantation, and reconstructive failure.1,3,4
Adjuvant chemotherapy (ACT), when indicated, offers up to a one-third reduction in 10-year breast cancer mortality.5,6 Neoadjuvant chemotherapy (NACT) can be used to control locally advanced breast cancer, reduce tumor size to facilitate lumpectomy in some cases, and assess, in real time, tumor responsiveness to the chemotherapeutic agent.7 Patients receiving NACT have similar rates of recurrence and of disease-free and overall survival relative to ACT.8 The mechanisms of action of chemotherapeutic agents that lead to tumor suppression have the theoretical potential of complicating surgical wound healing.9–12 Despite long-standing concerns with the concurrent use of chemotherapy (CT) either before or after mastectomy, the majority of studies suggest that this is not problematic.13–21 However, there are no large series that examine the differential impact of various chemotherapeutic agents or regimens on complication rates after TE reconstruction specifically.
In our study, we looked at the effects of different CT regimens on premature TE removal in immediate reconstruction and compared them to patients who did not have CT.
Methods
Study Sample
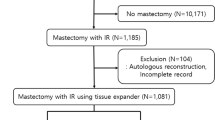
All patients undergoing skin-sparing mastectomy and immediate TE/I breast reconstruction from February 2003 to May 2013 at the Siteman Cancer Center were retrospectively identified from the physicians billing database of Washington University School of Medicine, St. Louis, Missouri. Further patient details were extracted from electronic medical records. Patients who had delayed, autologous, or direct-to-implant breast reconstruction, nipple-sparing mastectomy, or former ipsilateral radiation were excluded from the study, as were patients whose TE was not either prematurely removed or replaced with an implant or autologous flap.
Study Design
Data were retrospectively collected from medical records after Institutional Review Board Approval (Approval 201308013) at Washington University School of Medicine. Demographic information included age at reconstruction, BMI, comorbidities (i.e., diabetes and hypertension), and smoking (i.e., never, prior, and current). Clinical information included laterality of tumor and TE reconstruction, acellular dermal matrix (ADM) use, histology, tumor size, clinical stage, estrogen and progesterone receptor status, HER2/neu status, duration of reconstructive follow-up, duration of operation, and postmastectomy radiotherapy (PMRT). CT was divided into NACT and ACT. The specific regimens that were independently analyzed are listed in Table 1. In cases where premature TE removal occurred, the duration from placement to removal, and the reason for removal were recorded.
Treatment Algorithm
A TE was placed under the pectoralis major muscle and either an ADM or the serratus anterior muscle immediately after skin-sparing mastectomy. TEs were filled with a variable volume at the time of insertion, with further expansion commencing 3–4 weeks after surgery in the absence of wound-healing delays or infection. Drainage tubes placed superficial and deep to the pectoralis muscles were routinely used. A prophylactic intravenous dose of antibiotic was administered upon induction of anesthesia, and oral antibiotics were continued until drain removal, a duration of 1–3 weeks. When indicated, tissue expansion proceeded during CT, with fills performed within 24 h of the next infusion. CT was administered according to the recommendation of the medical oncologist. Patients who received NACT waited at least 4 weeks from their last CT treatment to mastectomy. Tissue expansion was completed before radiotherapy in all cases.
Statistical Analysis
Categorical variables were compared using Pearson’s Chi square or Fisher’s exact tests. Continuous variables were assessed with either Student’s t test to compare two groups or one-way analysis of variance (ANOVA) to compare multiple groups. Post hoc Tukey analysis identified which groups were significantly different. To analyze associations between covariates and premature TE removal, a binary stepwise logistic regression model was constructed. Any two variables with greater than 20 % correlation were included. Adjusted odds ratios (ORs) and 95 % confidence intervals (CIs) were calculated for each independent variable. Kaplan–Meier curves demonstrated the time period between TE placement and premature removal as a function of CT and radiotherapy, with the Mantel-Cox log-rank test used to compare groups. No patients were lost to follow-up from TE placement to replacement with implant or flap, so censoring was not needed. Statistical analyses were performed using SPSS 23 software (IBM, Chicago, IL, USA) with significance at alpha = 0.05.
Results
Patient Characteristics
A total of 1175 patients who received an immediate TE were evaluated. After exclusions, 899 patients (1347 breasts) comprised the study population (Table 2). Of these, 451 were unilateral (228 left; 223 right) and 448 bilateral, and 452 (50.3 %) left-sided and 447 (49.7 %) right-sided. There were 256 patients who received no CT, 295 NACT, and 348 ACT. Patients who received CT were significantly younger than those who did not (p < 0.001). Median BMI of all patients was 27 kg/m2 (range 16.3–57.8 kg/m2). Premature TE removal occurred in 16.9 % of the study cohort overall (Table 2), but it happened most frequently in the ACT (19.9 %) group, followed by the NACT (17.3 %) and no-CT (12.5 %) groups (p = 0.056). Premature TE removal happened earlier when no CT was administered compared to ACT (median of 58 vs. 78 days, p = 0.024).
Nonchemotherapeutic Factors Associated with TE Removal
A total of 152 TE (16.9 % of patients and 11.3 % of breasts) were prematurely removed because of complications. Infection, the most common complication, occurred in 55.9 % of these cases, followed by mastectomy flap necrosis (10.5 %), TE deflation (9.9 %), wound dehiscence (7.9 %), and exposure (4.6 %). Other causes like seroma, hematoma, and patient anxiety comprised the remainder (11.2. %). BMI was significantly higher (p < 0.001) in patients whose TE was removed (29.3 kg/m2) than in those where it was not (26.6 kg/m2). Patients with a BMI of over 35 kg/m2 were characterized by an increased incidence of TE removal (26.6 %) compared to all other BMI groups (p = 0.004). In contrast, patients stratified to the lowest BMI group of less than 25 kg/m2 had the fewest TE failures (12.7 %). Smoking was significantly (p < 0.001) more common in failed (36.2 %) than successful (16.7 %) TE reconstructions. Age, diabetes, cancer stage, tumor size, and length of surgery did not affect TE removal rates.
TE removal was significantly (p = 0.04) more common in patients who received radiotherapy (20 %) than in those who did not (15 %). Moreover, radiotherapy was more commonly delayed in patients with TE failure (130 vs. 84 days; p < 0.005). ADM use did not differ significantly between failed (77.6 %) and successful (80.1 %) TE reconstructions (p = 0.51).
Interaction of CT and Other Factors on TE Removal
Patients who had ACT experienced more TE failure (20 %) than other groups; this group approached statistical significance (p = 0.06). Binary logistic regression analysis demonstrated that current smoking (OR 3.46; 95 % CI 2.22–5.38; p < 0.001) and a BMI of over 35 kg/m2 (OR 2.65; 95 % CI 1.51–4.66; p < 0.001) were significant predictors of premature TE removal (Fig. 1). Further logistic regression analyses adjusted by CT group (Fig. 2) showed that in the no-CT group, current smoking increased premature TE removal (OR 3.1; 95 % CI 1.15–8.37; p = 0.025). In the NACT group, both prior smoking (OR 2.54; 95 % CI 1.12–5.79; p = 0.03) and current smoking (OR 3.54; 95 % CI 1.62–7.72; p = 0.001) were risk factors for premature TE removal. In the ACT group, BMI over 35 kg/m2 (OR 2.66; 95 % CI 1.24–5.71; p = 0.01) and current smoking (OR 4.21; 95 % CI 2.14–8.27; p < 0.001) increased premature TE removal. Radiotherapy was a risk factor for premature TE removal in the ACT group (OR 1.99; 95 % CI 1.09–3.67; p = 0.026) but not the NACT group (p = 0.76). When independently evaluated, none of the individual CT regimens was found to be a particular risk factor for TE failure.
Impact of CT on the Timing of Premature TE Removal
Analysis of the time interval between immediate TE placement and premature TE removal revealed that the mean time to TE removal was significantly earlier (p = 0.005) in the no-CT group (n = 32; mean 57 days) than the ACT group (n = 68; mean 74 days; Fig. 3). No patient receiving radiation in the no-CT group required premature TE removal (Table 2). The mean time to premature removal of a TE occurred sooner in patients receiving ACT without radiation (n = 33; mean 67 days) relative to ACT with radiation (n = 35; mean 93 days) and approached statistical significance (p = 0.055). In contrast, in patients receiving NACT, radiation significantly increased the mean time to premature TE removal, occurring in 36 days (n = 18) for NACT patients who did not receive radiation and 126 days (n = 31) for NACT patients who did receive radiation (p = 0.003). In the absence of radiation, premature TE removal occurred significantly sooner in the NACT group (n = 18; mean 36 days) than the ACT group (n = 33; mean 67 days; p = 0.035).
Kaplan–Meier survival analysis showing time period between TE placement and premature removal in patients with no CT, as well as those with neoadjuvant and adjuvant CT with or without radiation (p < 0.001). Explantations occurring after 30 days, indicated by black vertical line at 30-day time point, would not have been captured by NSQIP database. No CT and RT(−) no chemotherapy, no radiation; NACT and RT(−) neoadjuvant chemotherapy, no radiation; NACT and RT(+) neoadjuvant chemotherapy, radiation; ACT and RT(−) adjuvant chemotherapy, no radiation; ACT and RT(+) adjuvant chemotherapy, radiation
Discussion
The 16.9 % rate of premature TE removal found in our study is consistent with previous work.20,22 Premature TE removal rates were higher in patients treated with NACT (17.3 %) and ACT (19.9 %) compared to the no-CT group (12.5 %; p = 0.056). These trends are consistent with a smaller series of 108 TE reconstructions where patients who did not receive CT had slightly lower rates of loss (18 %) than those treated with NACT (26 %) or ACT (22 %).23 In our study, this finding can be explained in part by the fact that in the absence of CT or radiation, patients went on to exchange the TE with a permanent breast implant or autologous flap more quickly. As a result, the TE was simply not in as long as the other treatment groups, so the patient had a lower chance of experiencing an adverse event requiring explantation. However, if duration of TE implantation was the only factor contributing to differences in premature TE removal among groups, then the median value for premature TE explantation would have occurred closer to the middle of the follow-up period, halfway between TE insertion and exchange for an implant or autologous flap. However, this was not the case (Table 2). The majority of failures were clustered (Fig. 3) in the early phases after reconstruction (Table 2, median 67 days), closer temporally to when TE were placed than when they were exchanged (median 354 days). Treatment duration, along with radiation, CT, smoking, and BMI, represent only a few of the factors contributing to the heterogeneity of this patient population and the inherent challenges of comparing treatment groups.
With few exceptions, previous studies fail to show an association between NACT or ACT and complications after TE breast reconstruction.18,24–26 These studies, however, differ from the current one by often including mixed reconstructive cohorts, delayed and immediate reconstructions, and shorter follow-up times.15,18,26–28 One such study compared 180 patients receiving NACT to 485 receiving ACT and found a similar overall complication rate (30 vs. 31 %) in the first 60 days after mastectomy.28 Notably, 55.6 % of the NACT and 41.9 % of the ACT cohort did not undergo reconstruction at all.28 When reconstruction was performed, it consisted of a mixed cohort of prosthetic and autologous tissue reconstructions, and patients receiving NACT were less likely to undergo immediate reconstruction (28 %) relative to those receiving ACT (40 %). Surgeon preference and patient treatment fatigue after an exhaustive course of NACT were offered as possible explanations for this discrepancy. Interestingly, despite undergoing fewer immediate reconstructions, NACT patients in this series were also less likely to pursue a delayed reconstruction.26 At our institution we have found that overall reconstruction rates are not influenced by the administration of CT.29 However, patients receiving NACT are more likely to undergo delayed autologous flap reconstruction.
Particular CT regimens did not appear to differentially impact premature TE removal rates in our study (Fig. 2). Studies evaluating the effects of CT on immediate TE/I reconstruction rarely investigate the impact of a particular regimen or agent.15,24,28,30 Theoretically, specific chemotherapeutic agents may adversely impact wound healing and the risk of infection on an immediate TE.12 Both NACT and ACT compromise the remodeling of ADMs, frequently used in TE/I reconstruction.31–34 Because of a potentially insufficient sample size, we cannot rule out an association between a particular chemotherapeutic agent and premature TE loss. Any small adverse impact of a chemotherapeutic agent on reconstructive outcomes would be outweighed by its therapeutic benefit. Changing the order of CT with mastectomy and TE reconstruction may impact wound healing and outcomes. Patients who receive NACT may be impacted in the immediate postoperative period by the residual impact of previous CT (Table 2, median 68 days) and, when administered, a couple months later (Table 2, median 68 days) by PMRT. By contrast, ACT (Table 2, median 39 days) and PMRT (Table 2, median 194 days) impact later phases of wound healing. Patients requiring PMRT in the NACT are usually receiving radiation during the same period after mastectomy with TE as those in the ACT group are receiving CT.
Radiation significantly increased the rate of explantation in patients receiving ACT (Fig. 2) (p = 0.025). An association between radiation and premature TE removal is widely reported, but it is not clear why radiation increased premature TE removal in the ACT but not the NACT group.25 Some investigators suggest that NACT may confer a protective effect against early morbidity after mastectomy with reconstruction, which may counteract the deleterious effects of radiation.26 Because shorter operative times are an independent predictor of postoperative morbidity, they suggest that reducing tumor size with NACT in advance of mastectomy would lead to shorter operative times and fewer subsequent complications.26,35 This study, however, is consistent with our own findings that NACT leads to longer operative times (Table 2). The impact of radiation may extend beyond premature removal to impact the long-term success of a prosthesis after exchange.36,37 In fact, to mitigate the effects of radiation on prostheses, some practitioners routinely perform implant exchange before radiation.38 Consistent with other centers, we frequently replace the TE with an autologous flap to minimize the risk of radiation-associated implant loss after exchange, limit the risk of capsular contracture, and facilitate nipple reconstruction with nonirradiated tissue.37,39–44 At our institution, patients receiving NACT who will require radiation after mastectomy are more likely to forgo TE reconstruction altogether and proceed with an autologous flap after radiotherapy if other comorbidities like obesity or smoking are present. As such, an unexpectedly lower rate of TE explantation in the cohort of patients receiving an immediate TE, NACT, and PMRT may have been impacted by selection bias.
Current smoking was the only factor consistently associated with a significantly higher rate of premature TE removal for every treatment group and overall. A higher rate of mastectomy skin flap necrosis in smokers leading to device exposure, bacterial contamination, and explantation is corroborated by numerous studies.45–49 A higher percentage of patients were current smokers in the ACT and NACT group, but overall there was no statistically significant difference between current, past, and never smokers (p = 0.06). Although it is conceivable that differences in premature explantation were related to smoking, a history of smoking was also a significant predictor of premature explantation in the NACT group; however, there were more prior smokers in the no-CT than the NACT group (Table 2). Severe obesity (>35 kg/m2) was associated with an increased risk of premature TE removal for the overall study population (Fig. 1) and the ACT group (Fig. 2). The breast reconstruction literature is replete with studies that clearly show a deleterious impact of increasing BMI on reconstructive complications.50–54 As such, we modify our approach in managing this population by frequently performing delayed reconstructions or autologous flaps to limit risk.55,56 The unexpectedly low impact of BMI on premature TE removal in our patients, then, may result from selection bias and a limited cohort of overweight patients. Corticosteroids, routinely administered with chemotherapeutic regimens, may also affect premature TE removal, as they are known to impact wound healing in this context.57–64 Patients in the no-CT group did not receive corticosteroids, while those in the NACT group had not received them for a median of 68 days before mastectomy with TE reconstruction, a period longer than their reported impact on wound healing rates.65 Although the impact of corticosteroids on healing in prosthetic breast reconstruction is not well studied and it is largely inferred by their mechanism of action, we cannot rule out an increased impact of corticosteroid use in the ACT group versus the other cohorts. In addition, some data in a rodent sarcoma model suggest that the presence of cancer itself may delay cutaneous healing independent of adjuvant therapies.66,67
Time from mastectomy to premature TE removal varied significantly between groups (p = 0.024), as median time to explantation for patients treated with NACT (85 days) or ACT (78 days) exceeded that for those who did not receive CT (58 days). While a recent study utilizing the National Surgery Quality Improvement Program (NSQIP) database indicates that NACT does not increase complication rates with TE or any other form of immediate breast reconstruction within the first 30 days after surgery, data from our study suggest that this relatively short follow-up period may be inadequate to evaluate explantation rates after TE breast reconstruction.18 Patients who undergo prosthetic reconstruction usually receive oral antibiotics until drain removal, often continuing antibiotic therapy for up to 3 weeks after surgery.68–76 Prolonged use of perioperative antibiotics may simply suppress or delay an infection beyond the 30-day window recorded by NSQIP. Further, the effect of ACT on TE complication rates cannot be evaluated with NSQIP because ACT is administered after the 30-day window that is evaluated. In fact, in a review of 2285 breast implants placed for a mixture of reconstructive and aesthetic purposes, the mean time to explantation of reconstructive breast prostheses was 41 days.77 In this cohort, which also included direct-to-implant, implant exchange, delayed TE, and prostheses placed under flaps, less than 50 % of explants occurred within the first 30 days, with 9 % of explants happening >100 days after reconstructive prosthesis placement. In our study, premature TE removal occurred in the entire population at a median of 67 days after insertion.
Our study, with the inherent weaknesses of a retrospective review, was intentionally limited to immediate TE reconstructions after skin-sparing mastectomy to minimize the impact of variables like delayed or autologous reconstruction and nipple-sparing mastectomy. Exclusion of these other oncologic and reconstructive modalities increases susceptibility to selection bias and does not account for differences between oncologic and plastic surgeons with respect to factors like mastectomy flap thickness, surgical technique, and tolerance for delaying or attempts to salvage a potentially compromised TE. Moreover, the study was likely underpowered because differences between groups with respect to premature TE removal often approached but did not reach statistical significance.
Conclusions
Our data suggest that the majority of premature TE removals occur 2–3 months after placement, well after the follow-up period recorded by the NSQIP database, and can occur throughout the period of implantation. Moreover NACT or ACT may be independently associated with a higher incidence of premature TE removal after immediate reconstruction. Clinically, the biopsychosocial benefits of an immediate reconstruction should not be ignored. However, in patients who received NACT and for those at significant risk for requiring ACT, the option of a delayed reconstruction should be discussed, particularly in the presence of additional risk factors for premature TE removal like smoking, radiation, and severe obesity. In patients who experience clinical adverse effects related to CT, reconstruction can be delayed by limiting the pace of expander fills or delaying the time to device exchange. Our findings provide plastic and oncologic surgeons more specific information about the risk of premature TE removal, can be used to provide more precise counseling, and may guide the timing of follow-up so that patients may be evaluated when they are most susceptible to premature TE removal.
References
Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg. 2013;131:15–23.
Cemal Y, Albornoz CR, Disa JJ, et al. A paradigm shift in U.S. breast reconstruction: part 2. The influence of changing mastectomy patterns on reconstructive rate and method. Plast Reconstr Surg. 2013;131:320e-6e.
Garvey PB, Villa MT, Rozanski AT, et al. The advantages of free abdominal-based flaps over implants for breast reconstruction in obese patients. Plast Reconstr Surg. 2012;130:991–1000.
Weichman KE, Wilson SC, Weinstein AL, et al. The use of acellular dermal matrix in immediate two-stage tissue expander breast reconstruction. Plast Reconstr Surg. 2012;129:1049–58.
Early Breast Cancer Trialists’ Collaborative Group; Peto R, Davies C, et al. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet. 2012;379:432–44.
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Thompson AM, Moulder-Thompson SL. Neoadjuvant treatment of breast cancer. Ann Oncol. 2012;23(Suppl 10):x231–6.
van Nes JG, Putter H, Julien JP, et al. Preoperative chemotherapy is safe in early breast cancer, even after 10 years of follow-up; clinical and translational results from the EORTC trial 10902. Breast Cancer Res Treat. 2009;115:101–13.
Devereux DF, Thibault L, Boretos J, Brennan MF. The quantitative and qualitative impairment of wound healing by Adriamycin. Cancer. 1979;43:932–8.
Lawrence WT, Talbot TL, Norton JA. Preoperative or postoperative doxorubicin hydrochloride (Adriamycin): which is better for wound healing? Surgery. 1986;100:9–13.
Choron RL, Chang S, Khan S, et al. Paclitaxel impairs adipose stem cell proliferation and differentiation. J Surg Res. 2015;196:404–15.
Oh E, Chim H, Soltanian HT. The effects of neoadjuvant and adjuvant chemotherapy on the surgical outcomes of breast reconstruction. J Plast Reconstr Aesthet Surg. 2012;65:e267–80.
Bland KI, Palin WE, von Fraunhofer JA, et al. Experimental and clinical observations of the effects of cytotoxic chemotherapeutic drugs on wound healing. Ann Surg. 1984;199:782–90.
Calnan J, Davies A. The effect of methotrexate (amethopterin) on wound healing: an experimental study. Br J Cancer. 1965;19:505–12.
Gouy S, Rouzier R, Missana MC, et al. Immediate reconstruction after neoadjuvant chemotherapy: effect on adjuvant treatment starting and survival. Ann Surg Oncol. 2005;12:161–6.
Furey PC, Macgillivray DC, Castiglione CL, Allen L. Wound complications in patients receiving adjuvant chemotherapy after mastectomy and immediate breast reconstruction for breast cancer. J Surg Oncol. 1994;55:194–7.
Francis SH, Ruberg RL, Stevenson KB, et al. Independent risk factors for infection in tissue expander breast reconstruction. Plast Reconstr Surg. 2009;124:1790–6.
Decker MR, Greenblatt DY, Havlena J, et al. Impact of neoadjuvant chemotherapy on wound complications after breast surgery. Surgery. 2012;152:382–8.
Song J, Zhang X, Liu Q, et al. Impact of neoadjuvant chemotherapy on immediate breast reconstruction: a meta-analysis. PLoS One. 2014;9:e98225.
Warren Peled A, Itakura K, Foster RD, et al. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch Surg. 2010;145:880–5.
Narui K, Ishikawa T, Satake T, et al. Outcomes of immediate perforator flap reconstruction after skin-sparing mastectomy following neoadjuvant chemotherapy. Eur J Surg Oncol. 2015;41:94–9.
Sultan MR, Smith ML, Estabrook A, et al. Immediate breast reconstruction in patients with locally advanced disease. Ann Plast Surg. 1997;38:345–9.
Peled AW, Foster RD, Garwood ER, et al. The effects of acellular dermal matrix in expander-implant breast reconstruction after total skin-sparing mastectomy: results of a prospective practice improvement study. Plast Reconstr Surg. 2012;129:901e–8e.
Mitchem J, Herrmann D, Margenthaler JA, Aft RL. Impact of neoadjuvant chemotherapy on rate of tissue expander/implant loss and progression to successful breast reconstruction following mastectomy. Am J Surg. 2008;196:519–22.
Berry T, Brooks S, Sydow N, et al. Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol. 2010;17(Suppl 3):202–10.
Abt NB, Flores JM, Baltodano PA, et al. Neoadjuvant chemotherapy and short-term morbidity in patients undergoing mastectomy with and without breast reconstruction. JAMA Surg. 2014;149:1068–76.
Peled AW, Stover AC, Foster RD, et al. Long-term reconstructive outcomes after expander-implant breast reconstruction with serious infectious or wound-healing complications. Ann Plast Surg. 2012;68:369–73.
Hu YY, Weeks CM, In H, et al. Impact of neoadjuvant chemotherapy on breast reconstruction. Cancer. 2011;117:2833–41.
Elmore L, Myckatyn TM, Gao F, et al. Reconstruction patterns in a single institution cohort of women undergoing mastectomy for breast cancer. Ann Surg Oncol. 2012;19:3223–9.
Azzawi K, Ismail A, Earl H, et al. Influence of neoadjuvant chemotherapy on outcomes of immediate breast reconstruction. Plast Reconstr Surg. 2010;126:1–11.
Myckatyn TM, Cavallo JA, Sharma K, et al. The impact of chemotherapy and radiation therapy on the remodeling of acellular dermal matrices in staged, prosthetic breast reconstruction. Plast Reconstr Surg. 2015;135:43e–57e.
Sbitany H, Langstein HN. Acellular dermal matrix in primary breast reconstruction. Aesthet Surg J. 2011;31:30S–7S.
Sbitany H, Sandeen SN, Amalfi AN, et al. Acellular dermis-assisted prosthetic breast reconstruction versus complete submuscular coverage: a head-to-head comparison of outcomes. Plast Reconstr Surg. 2009;124:1735–40.
Namnoum JD. Expander/implant reconstruction with AlloDerm: recent experience. Plast Reconstr Surg. 2009;124:387–94.
Daley BJ, Cecil W, Clarke PC, et al. How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. J Am Coll Surg. 2015;220:550–8.
Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg. 2000;105:930–42.
Ascherman JA, Hanasono MM, Newman MI, Hughes DB. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg. 2006;117:359–65.
Cordeiro PG, Albornoz CR, McCormick B, et al. What is the optimum timing of postmastectomy radiotherapy in two-stage prosthetic reconstruction: radiation to the tissue expander or permanent implant? Plast Reconstr Surg. 2015;135:1509–17.
Buchholz TA, Kronowitz SJ, Kuerer HM. Immediate breast reconstruction after skin-sparing mastectomy for the treatment of advanced breast cancer: radiation oncology considerations. Ann Surg Oncol. 2002;9:820–1.
Kronowitz SJ, Lam C, Terefe W, et al. A multidisciplinary protocol for planned skin-preserving delayed breast reconstruction for patients with locally advanced breast cancer requiring postmastectomy radiation therapy: 3-year follow-up. Plast Reconstr Surg. 2011;127:2154–66.
Kronowitz SJ, Robb GL. Radiation therapy and breast reconstruction: a critical review of the literature. Plast Reconstr Surg. 2009;124:395–408.
Benediktsson K, Perbeck L. Capsular contracture around saline-filled and textured subcutaneously-placed implants in irradiated and non-irradiated breast cancer patients: five years of monitoring of a prospective trial. J Plast Reconstr Aesthet Surg. 2006;59:27–34.
Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg. 2006;59:1043–51.
Boccola MA, Savage J, Rozen WM, et al. Surgical correction and reconstruction of the nipple–areola complex: current review of techniques. J Reconstr Microsurg. 2010;26:589–600.
Lin KY, Blechman AB, Brenin DR. Implant-based, two-stage breast reconstruction in the setting of radiation injury: an outcome study. Plast Reconstr Surg. 2012;129:817–23.
McCarthy CM, Mehrara BJ, Riedel E, et al. Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg. 2008;121:1886–92.
Padubidri AN, Yetman R, Browne E, et al. Complications of postmastectomy breast reconstructions in smokers, ex-smokers, and nonsmokers. Plast Reconstr Surg. 2001;107:342–9.
Nguyen KT, Hanwright PJ, Smetona JT, et al. Body mass index as a continuous predictor of outcomes after expander-implant breast reconstruction. Ann Plast Surg. 2014;73:19–24.
Woerdeman LA, Hage JJ, Hofland MM, Rutgers EJ. A prospective assessment of surgical risk factors in 400 cases of skin-sparing mastectomy and immediate breast reconstruction with implants to establish selection criteria. Plast Reconstr Surg. 2007;119:455–63.
Albornoz CR, Cordeiro PG, Farias-Eisner G, et al. Diminishing relative contraindications for immediate breast reconstruction. Plast Reconstr Surg. 2014;134:363e–9e.
Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg. 2013;217:656–64.
Fischer JP, Nelson JA, Serletti JM, Wu LC. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005–2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg. 2013;66:1504–12.
Fischer JP, Wes AM, Kanchwala S, Kovach SJ. Effect of BMI on modality-specific outcomes in immediate breast reconstruction (IBR)—a propensity-matched analysis using the 2005–2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48:297–304.
Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Plast Reconstr Surg. 2011;128:395e–402e.
Hanwright PJ, Davila AA, Hirsch EM, et al. The differential effect of BMI on prosthetic versus autogenous breast reconstruction: a multivariate analysis of 12,986 patients. Breast. 2013;22:938–45.
Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265–74.
Markman M, Sheidler V, Ettinger DS, et al. Antiemetic efficacy of dexamethasone. Randomized, double-blind, crossover study with prochlorperazine in patients receiving cancer chemotherapy. N Engl J Med. 1984;311:549–52.
Cutroneo KR, Meisler N, Counts DF. Anti-inflammatory prednisolone derivatives inhibit collagen synthesis and pro-alpha(1) (I) collagen promoter activity in rat skin fibroblasts. Wound Repair Regen. 1994;2:292–6.
Wang AS, Armstrong EJ, Armstrong AW. Corticosteroids and wound healing: clinical considerations in the perioperative period. Am J Surg. 2013;206:410–7.
Coates A, Gebski V, Bishop JF, et al. Improving the quality of life during chemotherapy for advanced breast cancer. A comparison of intermittent and continuous treatment strategies. N Engl J Med. 1987;317:1490–5.
Soukop M. Management of cyclophosphamide-induced emesis over repeat courses. Oncology. 1996;53(Suppl 1):39–45.
Roohk DJ, Varady KA, Turner SM, et al. Differential in vivo effects on target pathways of a novel arylpyrazole glucocorticoid receptor modulator compared with prednisolone. J Pharmacol Exp Ther. 2010;333:281–9.
Autio P, Oikarinen A, Melkko J, et al. Systemic glucocorticoids decrease the synthesis of type I and type III collagen in human skin in vivo, whereas isotretinoin treatment has little effect. Br J Dermatol. 1994;131:660–3.
Cavallo JA, Gangopadhyay N, Dudas J, et al. Remodeling characteristics and collagen distributions of biologic scaffold materials biopsied from postmastectomy breast reconstruction sites. Ann Plast Surg. 2015;75:74–83.
Ismael H, Horst M, Farooq M, et al. Adverse effects of preoperative steroid use on surgical outcomes. Am J Surg. 2011;201:305–8.
Lawrence WT, Norton JA, Harvey AK, et al. Wound healing in sarcoma-bearing rats: tumor effects on cutaneous and deep wounds. J Surg Oncol. 1987;35:7–12.
Thomas Hess C. Checklist for factors affecting wound healing. Adv Skin Wound Care. 2011;24:192.
Alderman A, Gutowski K, Ahuja A, et al. ASPS clinical practice guideline summary on breast reconstruction with expanders and implants. Plast Reconstr Surg. 2014;134:648e–55e.
Avashia YJ, Mohan R, Berhane C, Oeltjen JC. Postoperative antibiotic prophylaxis for implant-based breast reconstruction with acellular dermal matrix. Plast Reconstr Surg. 2013;131:453–61.
Lanier ST, Wang ED, Chen JJ, et al. The effect of acellular dermal matrix use on complication rates in tissue expander/implant breast reconstruction. Ann Plast Surg. 2010;64:674–8.
Chun YS, Verma K, Rosen H, et al. Implant-based breast reconstruction using acellular dermal matrix and the risk of postoperative complications. Plast Reconstr Surg. 2010;125:429–36.
Liu AS, Kao HK, Reish RG, et al. Postoperative complications in prosthesis-based breast reconstruction using acellular dermal matrix. Plast Reconstr Surg. 2011;127:1755–62.
Nahabedian MY. AlloDerm performance in the setting of prosthetic breast surgery, infection, and irradiation. Plast Reconstr Surg. 2009;124:1743–53.
Spear SL, Parikh PM, Reisin E, Menon NG. Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg. 2008;32:418–25.
Breuing KH, Colwell AS. Inferolateral AlloDerm hammock for implant coverage in breast reconstruction. Ann Plast Surg. 2007;59:250–5.
Brzezienski MA, Jarrell JAt, Mooty RC. Classification and management of seromas in immediate breast reconstruction using the tissue expander and acellular dermal matrix technique. Ann Plast Surg. 2013;70:488–92.
Cohen JB, Carroll C, Tenenbaum MM, Myckatyn TM. Breast implant-associated infections: the role of the National Surgical Quality Improvement Program and the local microbiome. Plast Reconstr Surg. 2015;136(5):921–9.
Acknowledgment
The authors are grateful to Dr. A. Tülay Bağci Bosi, MSc, PhD, epidemiologist at the Department of Public Health, University of Hacettepe School of Medicine, Turkey, for guidance and review of our statistical analyses.
Disclosures
No funds from any granting agency or company were used to prepare this manuscript. Dr. Myckatyn: Receives grant funding from Allergan which makes breast implants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dolen, U.C., Schmidt, A.C., Um, G.T. et al. Impact of Neoadjuvant and Adjuvant Chemotherapy on Immediate Tissue Expander Breast Reconstruction. Ann Surg Oncol 23, 2357–2366 (2016). https://doi.org/10.1245/s10434-016-5162-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5162-y