Abstract
Background
There is limited evidence regarding the factors causing a prolonged time for tissue expander (TE) exchange into a definitive implant using two-stage implant-based breast reconstruction (IBBR). This study aimed to review our experience with IBBR, focusing on the time for TE-to-implant exchange and determining which factors cause a prolonged time for exchange.
Methods
A retrospective review was performed to include women undergoing immediate two-stage IBBR with TEs after total mastectomy between January 2011 and May 2021. Reconstructions with irradiated TEs were excluded. Cases that had a prolonged time for TE-to-implant exchange were defined as those undergoing exchange longer than 232 days, which corresponds to the 75th percentile of the overall study group.
Results
We included 442 reconstructions in our analysis. The median age for our series was 51 years and the median body mass index was 26.43-kg/m2. The median time for TE-to-implant exchange was 155 days [IQR, 107–232]. Cases that had a prolonged time for TE-to-implant exchange were defined as those undergoing exchange on postoperative day 232 or afterward. Diabetes (OR 4.05, p = 0.006), neoadjuvant chemotherapy (OR 2.76, p = 0.006), an increased length of stay (OR 1.54, p = 0.013), and a lengthier time to complete outpatient expansions (OR 1.018, p < 0.001) were independently associated with a prolonged time for exchange.
Conclusion
As evident from our analysis, the time for exchange is highly heterogeneous among patients. Although several factors affect the timing for TE-to-implant exchange, efforts must be directed to finalize outpatient expansions as soon as possible to expedite the transition into a definitive implant.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, breast reconstruction has experienced several changes and improvements so that we can recreate the breast mound more accurately and provide better surgical outcomes [1]. Although different surgical techniques are available, most patients undergoing total mastectomy prefer implant-based breast reconstruction (IBBR) in the USA [2, 3]. A two-stage approach with tissue expander (TE) prevails as the most common modality for this purpose despite the growing rate of procedures performed with a direct-to-implant technique [4,5,6]. Most of the time this type of reconstructions can be performed without donor site surgery, which makes it very appealing to some patients [7]. When compared to autologous reconstruction, IBBR usually exhibits a lower rate of complications and reoperations but a higher rate of failure [8]. Nonetheless, innovations in implant manufacturing and the incorporation of cutting-edge covering materials such as acellular dermal matrix (ADM) products have substantially improved the results of two-stage IBBR [9].
There are important considerations regarding the timing of TE-to-implant exchange. Once the decision is taken to replace the TE with a definitive implant, symmetrization of the contralateral side can be performed to conclude the reconstructive process and decrease the psychological burden of the oncologic disease. In case radiation is needed, radiation to the TE before the exchange permits surgeons to address any radiation-induced complication during the second stage [10]. On the other hand, it is well known that radiation to the TE generates a prolonged time for TE-to-implant exchange. Therefore, some surgeons may prefer to perform the exchange before radiation starts, as operating on irradiated tissues can be extremely challenging [11, 12]. Finally, delaying postmastectomy radiotherapy may be a concern for some radiation oncologists as this window can theoretically contribute to an increased risk of local recurrence [13]. Hence, expeditious transition into a definitive implant is paramount for some patients.
Previous studies have focused on the optimal timing of TE-to-implant exchange after TE irradiation in immediate two-stage IBBR [14,15,16]. However, there is limited evidence regarding the factors causing a prolonged transition into a definitive implant in patients undergoing two-stage IBBR. This study aimed to review our experience with IBBR using TEs, focusing on the time for TE-to-implant exchange and determining which patient-associated or surgical-related variables can cause a prolonged time for exchange into a definitive implant.
Methods and Patients
Institutional Review Board (IRB) approval was obtained, and a retrospective review of medical records was conducted at a single academic center. Adult women (≥ 18 years) undergoing immediate two-stage IBBR with TEs after total mastectomy between January 2011 and May 2021 were included. Delayed TE placement, direct-to-implant reconstruction, and autologous tissue-assisted reconstruction at the time of TE placement were our exclusion criteria. As radiation to the TE can significantly increase the time for exchange, we did not include these reconstructions. However, we included reconstructions that required postmastectomy radiotherapy to the permanent implant (after TE-to-implant exchange).
The utilization of ADM products, plane for TE placement, intraoperative TE volume, type of filling (air/saline), time to initiate outpatient expansions, and time for TE-to-implant exchange depended on the attending surgeon’s preference and the patients’ availability. When ADMs were used, TEs were partially wrapped along the inferior pole for submuscular reconstruction or completely wrapped for prepectoral TE placement [17]. Prepectoral or subpectoral TE placement, the use of acellular dermal matrix (ADM) products, and using inferiorly-based dermal flaps have been previously reported [3, 6, 17, 18]. Each individual reconstruction (hemithorax) was regarded as an independent subject for analysis. Drains were removed once output was less than 30-cc per day during 48 consecutive hours.
The time to complete outpatient expansions was defined as the period from immediate TE placement to the postoperative day when the last expansion was performed once the TE volume was deemed appropriate. The time for TE-to-implant exchange was defined as the period from the day of immediate TE placement to the postoperative day when the TE was removed, and a definitive implant was placed. Cases with prolonged time for TE-to-implant exchange were defined as those with a time for exchange longer than the 75th percentile (three-fourths) of that of the overall study group.
Data Extraction
We extracted the following data for this study: number of reconstructions, age, smoking status, body mass index, past medical history of diabetes or hypertension, race/ethnicity, preoperative hematocrit, type of the reconstruction (bilateral/unilateral), diagnosis and stage of the oncologic process, status of hormonal receptors, type of mastectomy (nipple-sparing/skin-sparing), mastectomy pattern, estimated blood loss, plane for TE insertion (prepectoral/subpectoral), type of intraoperative TE filling, use of SPY fluorescence imaging, use of ADMs, blocks with local anesthesia, and neoadjuvant and adjuvant therapies (e.g., radiotherapy, chemotherapy). The mastectomy patterns were classified according to the categories described by Dec et al. [19]. Our surgical outcomes included the intraoperative TE volume, number of drains, drain duration, time for first outpatient expansion, final TE volume, time to conclude outpatient expansions, time for TE-to-implant exchange, size of the implant, 30-day morbidity, and complications during the first stage of reconstruction.
For postoperative complications, we calculated the rate of hematoma, return to the operating room (RTOR) for hematoma evacuation, seroma, periprosthetic infection, infection-related TE explantation, wound disruption (e.g., mastectomy flap necrosis, dehiscence), wound disruption-related unplanned interventions (excision/debridement and closure or TE explantation/removal), TE displacement, TE leak, fat necrosis, and capsular contracture. For this study, all TEs removed during the first phase of reconstruction (with TEs) secondary to any complication were replaced with a second TE in a delayed fashion or were immediately exchanged for a second TE.
Statistical Analysis
Fisher’s exact test was used to analyze categorical data. Continuous data were analyzed with the t test or Mann–Whitney test. Non-normal data were presented as median and interquartile range [IQR]. To determine which factors were independent predictors for a prolonged time for TE-to-implant exchange, variables deemed statistically significant during univariable analysis were integrated into a multivariable regression model. To assess the fitting behavior of the regression model, the area under the receiver operating characteristic (ROC) curve was estimated. An area under the curve greater than 0.6 suggested a satisfactory performance of the model.
Multivariable linear regression analysis was used to analyze whether there was a significant association between the time to finish the last outpatient expansion (days) and the time for TE-to-implant exchange (days). Natural log transformations were applied to variables incorporated in the linear regression if a significant p-value rejected the null hypothesis for the Shapiro–Wilk test. All analyses were performed using R statistical software, version 4.0.0 (R Core Team, 2020) [20]. A p < 0.05 was considered statistically significant.
Results
We initially included 527 immediate IBBRs with TEs in 335 patients. Forty-five reconstructions of the 527 had either abandoned IBBR or were still undergoing expansions when this study was concluded. At the time of chart review, 482 reconstructions underwent TE-to-implant exchange and were preliminary analyzed. From our previous experience, we knew radiation of TEs considerably increased the time for exchange (Supplemental Data 1). Thus, we excluded 40 reconstructions that received radiotherapy to the TE, and we ultimately included 442 reconstructions in our analysis (Fig. 1).
Overall, the median age for our series was 51 years [IQR, 43–59] and the median body mass index was 26.43 kg/m2 [IQR, 23.3–30.4]. Most reconstructions were performed in White/Caucasian (80.8%) and African-American/Black patients (10.4%). Overall, 4.3% of the reconstructions were performed in current smokers, while 33.3% were performed in former smokers. Twenty-eight percent of the reconstructions were performed in patients with past medical history of hypertension and 6.3% in patients with diabetes mellitus (Table 1).
Most reconstructions were performed after therapeutic mastectomy (56.1%). Data regarding the diagnosis and staging of breast cancer are reported in Table 2. Pre-mastectomy radiotherapy was reported in 1.6% of the reconstructions, while 14.9% of the reconstructions were performed in patients who had neoadjuvant chemotherapy. Adjuvant chemotherapy was reported in 23.1% of the reconstructive cases, while 9.3% of the reconstructions received adjuvant radiotherapy to the definitive implant after TE-to-implant exchange. Adjuvant radiotherapy to the implant was performed at a median time of 38 days (IQR, 30–55 days) after TE-to-implant exchange.
Peripheral nerve blocks were used in 44.3% of the reconstructions. Most ablative procedures were skin-sparing mastectomies (85.5%). The transverse mastectomy pattern (e.g., teardrop-shaped, fusiform periareolar, oblique) was the most common pattern for incisions (60.4%). The median mastectomy specimen weight was 519.5 gr [IQR, 355.25–769]. Most procedures were bilateral (81.2%) and subpectoral (74.7%) reconstructions using textured TEs (65.4%). SPY fluorescence imaging was used in 30.5% of the cases. ADMs were used in 89.1% of the cases (Table 3). Saline was used in 76.5% of the cases for intraoperative filling of TE, while air was used in 23.5% of the reconstructions. Most reconstructions had two drains in place at the time of reconstruction (69.2%).
Surgical Outcomes
The surgical outcomes are reported in Table 4. The median length of stay was 1 day [IQR, 1–2]. The median intraoperative expansion volume was 250 ml [IQR, 100–300]. The median duration of drains was 14 days [IQR, 11–20]. The median time for first outpatient expansion was 22 days [IQR, 15–34], and the time to complete the expansion process was 51.5 days [IQR, 35–82.5]. The median volume of TEs at the end of the expansion process was 470 ml [IQR, 362.5–557.75]. The median time for TE-to-implant exchange was 155 days [IQR, 107–232]. Cases that had a prolonged time for TE-to-implant exchange (> 75th percentile) were defined as those undergoing exchange on postoperative day 232 or afterward (Fig. 2). The median time to receive a definitive implant in reconstructions that had a prolonged exchange was 337 days [IQR, 272–457], and for those that underwent an early exchange was 131 days [IQR, 93.5–176.75] (p < 0.001).
Logistic Regression Analysis
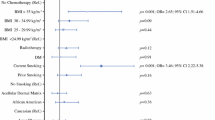
We evaluated factors associated with a prolonged time for TE-to-implant exchange following immediate TE placement (> 232 days) (Supplemental Data 2). Diabetes (OR 2.75, p = 0.01), the stage of the oncologic disease (Stage I versus no malignancy; OR 0.55, p = 0.037), neoadjuvant chemotherapy (OR 2.02, p = 0.012), SPY fluorescence imaging (OR 0.46, p = 0.004), subpectoral versus prepectoral device placement (OR 1.77, p = 0.037), length of stay (OR 1.73, p < 0.001), using air versus saline for intraoperative TE filling (OR 0.41, p = 0.004), using two drains versus one drain (OR 0.485, p = 0.001), the time to initiate outpatient expansions (OR 1.01, p < 0.001), the time to conclude outpatient expansions (OR 1.016, p < 0.001), the final TE volume (OR 1.001, p = 0.044), the size of the definitive implant (OR 1.002, p = 0.04), and adjuvant irradiation to the definitive implant (OR 0.29, p = 0.023) were initially associated with either prolonged or early TE-to-implant exchange on univariable analysis.
On multivariable analysis, diabetes (OR 4.05, p = 0.006), neoadjuvant chemotherapy (OR 2.76, p = 0.006), an increased length of stay (OR 1.54, p = 0.013), and a lengthier time to complete outpatient expansions (OR 1.018, p < 0.001) were independently associated with increased odds of a prolonged time for TE-to-implant exchange. On the other hand, the use of two drains versus one (OR 0.4, p = 0.004) and performing adjuvant radiotherapy to the definitive implant (OR 0.21, p = 0.037) were independently associated with decreased odds of a prolonged TE-to-implant exchange (Table 5). This means that using two drains instead of one and adjuvant radiotherapy to the definitive implant increased the probability of an early exchange. The area under the curve was estimated to be 0.818 (Fig. 3).
Complication Profile
We investigated the rate of complications of the first stage to characterize morbidity among reconstructions that had prolonged TE-to-implant exchange and those undergoing early exchange. In terms of acute complications, a higher rate of 30-day TE explantations secondary to infection was reported in reconstructions that had a prolonged time for TE-to-implant exchange (5.4% vs. 0.9%, p = 0.01) (Table 6). Evaluating the entire time between immediate reconstruction and exchange, higher rates of periprosthetic infection (21.4% vs. 9.7%, p = 0.004), infection-related TE explantations (8% vs. 1.5%, p = 0.002), and wound disruption-related TE explantations (8% vs. 1.8%, p = 0.004) were reported in reconstructions that had a prolonged time for TE-to-implant exchange (Table 7).
Linear Regression Analysis
Multivariable linear regression analysis confirmed the (log-transformed) time to complete outpatient expansions to be a significant predictor for the (log-transformed) time for TE-to-implant exchange after adjusting for the rate of 30-day periprosthetic infection-related TE explantations and rate of wound disruption-related TE explantations (Supplemental Data 3). The (log-transformed) time to complete outpatient expansions was positively associated with the (log-transformed) time for TE-to-implant exchange in our different models.
Discussion
This study demonstrated that the time for TE-to-implant exchange can be highly heterogeneous among subjects. Using our predetermined threshold for prolonged TE-to-implant exchange (≥ 232 days), we found that past medical history of diabetes, neoadjuvant chemotherapy, an increased length of stay, and an increased time to complete outpatient expansions increased the odds of a prolonged time for exchange. Conversely, using two versus one drain and adjuvant radiotherapy to the definitive implant expedited the exchange process (decreased the odds of a prolonged time for exchange).
In this study, the time to complete outpatient expansions was 51.5 days [IQR, 35–82.5]. However, outcomes on this matter have been highly diverse with the mean of different studies ranging from 21 to 133 days [9, 21]. Similar to our outcomes, Collins et al. reported the mean time to complete the expansion process to be 58 days (range, 21–177) [22], while Foo et al. reported an average of 4–5 weeks (28–35 days) [23]. When comparing the plane of TE placement, two different studies have shown that a prepectoral approach reduced the time of the expansion process compared to a subpectoral approach [24, 25]. Wormer et al. registered a mean time to expansion completion of 40.4 ± 37.8 days with prepectoral placement compared to 62.5 ± 50.2 days with a subpectoral technique (p < 0.001) [24]. Likewise, Haddock et al. reduced the time to complete expansions from 49.11 ± 44.07 days with subpectoral placement to 23.48 ± 34.67 days with a prepectoral approach (p < 0.001) [25]. Another strategy to reduce the expansion time presented in contemporary reports has been the incorporation of carbon dioxide-based expansions using remote-activated TEs. Ascherman et al. reported a median time to complete expansions of 21 days (range, 5–117 days) with AirXPanders for prepectoral and subpectoral IBBR [21].
In our study, the median time for TE-to-implant exchange was 155 days. Heterogeneity within and between studies has also been a constant for this outcome. Using AirXPanders (AeroForm TE), the authors reported a median time to reach exchange of 112 days (range, 55–329 days) [21]. Other authors using standard TEs have reported the time for exchange to be 154 days, similar to our result [22]. Remarkably, although prepectoral approach may reduce the time to complete outpatient expansions [24], the time to reach TE-to-implant exchange has been comparable among patients undergoing subpectoral and prepectoral reconstruction in several articles. For instance, as reported by Wormer et al. (200.5 ± 93.3 days versus 169.3 ± 56.1, p = 0.191) [24], or as evident from our previous propensity score-matched analysis (175 days vs. 152 days, p = 0.53), no difference was found regarding the time of exchange comparing the prepectoral versus subpectoral technique [3]. Of note, studies comparing microtextured versus macrotextured TEs have also demonstrated an extended mean time for exchange of almost a year (11.9 months vs. 11.7 months, p = 0.474) [9].
Benefits of early exchange include that patients can undergo nipple reconstruction in a more expeditious way, can undergo symmetrization procedures of the contralateral side (e.g., contralateral mastopexy, reduction mammoplasty, augmentation mammoplasty), and can conclude the reconstructive process. Furthermore, an early TE-to-implant exchange has been suggested to increase satisfaction among patients. For instance, Foo et al. highlighted that 81% of patients preferred an early exchange (within two weeks of the last outpatient expansion) rather than a late exchange (6 months after outpatient expansions were completed [23].
Although there is no definitive consensus on an ideal timing to receive a definitive implant after ambulatory expansions, an early TE-to-implant exchange has been favored by several authors as it can also decrease the rate of some postoperative complications. Schwartz presented a retrospective study of 430 reconstructions undergoing “conventional” exchange surgery at least 6 months after initial TE placement (n = 224), and reconstructions that underwent a rapid exchange protocol, 3–6 weeks after initial TE placement, (n = 206) [26]. Compared to “conventional” exchange, a rapid exchange had a lower rate of overall major late complications (7.6% vs. 1.5%, p = 0.003), major infectious complications after TE exchange (3.9% vs. 0%, p < 0.001), and infection-related device explantations (3.6% vs. 0%, p < 0.001) [26]. On multivariable analysis, “conventional” exchange was associated with major late infectious complications requiring implant removal or salvage (OR 3.6, 95%CI 1.4 to 7.8, p = 0.009). In another study, Fuji et al. presented a case series of 25 breasts that underwent reconstruction with TEs but were not exchanged within a year of immediate TE placement (first stage) [27]. The incidence of TE rupture was determined to begin at 1.5 years after the initial insertion, and the cumulative rate of TE rupture was 32.6% and 55.1% by the third and fifth year, respectively [27].
From our analysis, we found that some complications following immediate TE placement were associated with a prolonged time for TE-to-implant exchange. For instance, surgeons may delay TE-to-implant exchange if the reconstruction presents with periprosthetic infection to let the inflammation subside and achieve complete resolution of the infectious process. Although the incidence of these complications may have a meaningful influence on the timing for exchange, we believe that a shorter period to conclude outpatient expansions can be an even stronger predictor for early TE-to-implant exchange. Certainly, our multivariable linear regression analysis confirmed our hypothesis demonstrating a strong association between the time to complete outpatient expansions and time for exchange (days) when adjusting for the incidence of 30-day infection-related TE explantations and wound disruption-related TE explantations. Further studies are required to determine an adequate window between immediate TE placement and exchange for a definitive implant that yields the best surgical outcomes in terms of safety.
Of note, adjuvant chemotherapy may delay the expansion process at some institutions. Furthermore, some surgeons may argue that these patients could be at a higher risk of valve site infection, and they recommend avoiding expansion sessions during periods of immunosuppression secondary to chemotherapy. At our institution, we always schedule the expansion during the weeks when patients are not undergoing adjuvant chemotherapy. As chemotherapy is not administered weekly but every other week, we coordinate with our medical oncology group to ensure that expansion occurs during the weeks when patients are not receiving chemotherapy. Additionally, we strictly adhere to a minimum 72-hour interval after the last chemotherapy dose before proceeding with any expansion.
Limitations
Although a specific database was systematically created for this study and the subject population is substantially homogeneous, this study has some limitations. The retrospective nature of this study limits how accurately data were recorded when reviewing the records of patients. Multiple surgeons performed the oncologic and reconstructive segments of the procedures. Variations between institutions regarding operating room availability, the surgeons’ preferences, and the patients’ schedules and availability for expansion, may limit the reproducibility and the external validity of our results. Causality cannot be determined due to the type of study.
Conclusion
As evident from our analysis, the time for TE-to-implant exchange is highly heterogeneous among patients. As suspected, factors that are historically associated with increased risk of complications such as neoadjuvant chemotherapy and diabetes increased the odds of prolonged time for TE-to-implant exchange. On the other hand, the need for postmastectomy radiotherapy aiming to irradiate the breast after exchange was an independent predictor to decrease the time for TE-to-implant exchange. Although several complications may affect the timing for TE-to-implant exchange, efforts must be directed to finalize outpatient expansions as soon as possible to expedite the transition into a definitive implant.
References
Colwell AS, Taylor EM (2020) Recent advances in implant-based breast reconstruction. Plast Reconstr Surg 145(2):421e–432e
Albornoz CR, Bach PB, Mehrara BJ et al (2013) A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg 131(1):15–23
Escandón JM, Sweitzer K, Christiano JG et al (2022) Subpectoral versus prepectoral two-stage breast reconstruction: a propensity score-matched analysis of 30-day morbidity and long-term outcomes. J Plast Reconstr Aesthet Surg 76:76–87
Chopra K, Singh D, Hricz N, Brassard K, Orlov V, Holton Iii LH (2019) Two-stage prosthetic prepectoral breast reconstruction: comparing tissue expansion with carbon dioxide and saline. Plast Reconstr Surg Glob Open 7(3):e2051
Kraenzlin FS, Darrach H, Chopra K, Rosson GD, Broderick KP, Sacks JM (2020) Prepectoral 2-stage breast reconstruction with carbon dioxide tissue expansion. Plast Reconstr Surg Glob Open 8(5):e2850
Escandón JM, Ali-Khan S, Christiano JG et al (2020) Simultaneous fat grafting during tissue expander-to-implant exchange: a propensity score-matched analysis. Aesthet Plast Surg. https://doi.org/10.1007/s00266-022-03152-7
Ozturk CN, Ozturk C, Soucise A et al (2018) Expander/implant removal after breast reconstruction: analysis of risk factors and timeline. Aesthet Plast Surg 42(1):64–72
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2018) Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg 153(10):901–908
Lee K-T, Park HY, Jeon B-J, Mun G-H, Bang SI, Pyon JK (2021) Does the textured-type tissue expander affect the outcomes of two-stage prosthetic breast reconstruction? A propensity score matching analysis between macrotextured and microtextured expanders. Plast Reconstr Surg 147(3):545–555
Kronowitz SJ, Lam C, Terefe W et al (2011) A multidisciplinary protocol for planned skin-preserving delayed breast reconstruction for patients with locally advanced breast cancer requiring postmastectomy radiation therapy: 3-year follow-up. Plast Reconstr Surg 127(6):2154–2166
Cordeiro PG (2016) Reply: what is the optimum timing of postmastectomy radiotherapy in two-stage prosthetic reconstruction: radiation to the tissue expander or permanent implant? Plast Reconstr Surg 138(1):151e
Cordeiro PG, Pusic AL, Disa JJ, McCormick B, VanZee K (2004) Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 113(3):877–881
Tsoutsou PG, Koukourakis MI, Azria D, Belkacémi Y (2009) Optimal timing for adjuvant radiation therapy in breast cancer: a comprehensive review and perspectives. Crit Rev Oncol Hematol 71(2):102–116
Kim A, Bae J, Bang S-I, Pyon J-K (2022) Optimal timing of expander-to-implant exchange after irradiation in immediate two-stage breast reconstruction. Plast Reconstr Surg 149(2):185e–194e
Naoum GE, Ioakeim MI, Shui AM et al (2022) Radiation modality (proton/photon), timing, and complication rates in patients with breast cancer receiving 2-stages expander/implant reconstruction. Pract Radiat Oncol 12(6):475–486
Yan C, Fischer JP, Freedman GM et al (2016) The timing of breast irradiation in two-stage expander/implant breast reconstruction. Breast J 22(3):322–329
Sbitany H, Sandeen SN, Amalfi AN, Davenport MS, Langstein HN (2009) Acellular dermis-assisted prosthetic breast reconstruction versus complete submuscular coverage: a head-to-head comparison of outcomes. Plast Reconstr Surg 124(6):1735–1740
Calderon T, Skibba KE, Hansen T, Amalfi A, Chen E (2022) Safety of breast reconstruction using inferiorly based dermal flap for the ptotic breast. Ann Plast Surg 88(3 Suppl 3):S156–S162
Lotan AM, Tongson KC, Police AM, Dec W (2020) Mastectomy incision design to optimize aesthetic outcomes in breast reconstruction. Plast Reconstr Surg Glob Open 8(9):e3086
R Core Development Team. R Core Team (2021) R: a language and environment for statistical computing. (Version 4.0) [Computer Software]. Retrieved from https://cran.r-project.org/. Published online 2021. https://cran.r-project.org
Ascherman JA, Zeidler K, Morrison KA et al (2020) Results of XPAND II: a multicenter, prospective, continued-access clinical trial using the aeroform tissue expander for two-stage breast reconstruction. Plast Reconstr Surg 145(1):21e–29e
Collis N, Sharpe DT (2000) Breast reconstruction by tissue expansion. A retrospective technical review of 197 two-stage delayed reconstructions following mastectomy for malignant breast disease in 189 patients. Br J Plast Surg 53(1):37–41
Foo IT, Coleman DJ, Holmes JD, Palmer JH, Sharpe DT (1992) Delay between expansion and expander/implant exchange in breast reconstruction—a prospective study. Br J Plast Surg 45(4):279–283
Wormer BA, Valmadrid AC, Ganesh Kumar N et al (2019) Reducing expansion visits in immediate implant-based breast reconstruction: a comparative study of prepectoral and subpectoral expander placement. Plast Reconstr Surg 144(2):276–286
Haddock NT, Kadakia Y, Liu Y, Teotia SS (2021) Prepectoral versus subpectoral tissue expander breast reconstruction: a historically controlled, propensity score-matched comparison of perioperative outcomes. Plast Reconstr Surg 148(1):1–9
Schwartz J-CD (2020) Early expander-to-implant exchange after postmastectomy reconstruction reduces rates of subsequent major infectious complications. Plast Reconstr Surg Glob Open 8(12):e3275
Fujii T, Yajima R, Kuwano H (2016) Implications of long-term indwelling of tissue expander in breast reconstruction: risk of expander rupturing. Anticancer Res 36(8):4337–4340
Funding
None of the authors received any funds or has any financial interests to disclose for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors did not receive any compensation or financial support for this study. The authors have no commercial associations to disclose related to this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained for all subjects included in this study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has not been presented in a national or international meeting.
Supplementary Information
Below is the link to the electronic supplementary material.
266_2023_3536_MOESM1_ESM.tiff
Supplemental Data 1: Distribution of reconstruction that had the TE irradiated versus reconstructions that did not have radiation to the TE expander. Reconstructions that had adjuvant radiation to the definitive implant after TE-to-implant exchange were assigned into the “No Irradiation of the TE” group. The median time for TE-to-implant exchange when the TE was irradiated before exchange was 505 days [IQR, 441.7 – 568.5] (TIFF 2078 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Escandón, J.M., Langstein, H.N., Christiano, J.G. et al. Predictors for Prolonged TE-to-Implant Exchange During Implant-Based Breast Reconstruction: A Single Institution Experience. Aesth Plast Surg 48, 2088–2097 (2024). https://doi.org/10.1007/s00266-023-03536-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-023-03536-3