Abstract
Introduction
Rapid MRI with ultrafast T2 sequences can be performed without sedation and is often used in place of computed tomography (CT) to evaluate pediatric patients for indications such as hydrocephalus. This study investigated the sensitivity of rapid magnetic resonance imaging (MRI) for detection and follow-up of acute intracranial hemorrhage in comparison to CT, which is commonly the first-line imaging.
Methods
Patients presenting to a pediatric hospital with acute intracranial hemorrhage on CT and follow-up rapid MRI within 48 h were included. Rapid MRI studies consisted of three plane ultrafast T2 sequences either with or without axial gradient echo (GRE) sequences. Identification of hemorrhage on rapid MRI was assessed by readers both blinded and unblinded to prior CT results.
Results
One hundred two acute hemorrhages in 61 patients were identified by CT. Rapid MRI detection of subdural and epidural hemorrhages was modest in the absence of prior CT for comparison (sensitivity 61–74 %), but increased with review of the prior CT (sensitivity 80–86 %). Hemorrhage size was a significant predictor of detection (p < 0.0001). Three plane fast T2 images alone without GRE sequences were poor at detecting subarachnoid hemorrhage (sensitivity 10–25 %); rapid MRI with GRE sequences identified the majority of subarachnoid hemorrhage (sensitivity 71–93 %). GRE modestly increased detection of other extra-axial hemorrhages.
Conclusions
Rapid MRI with GRE sequences is sensitive for most acute intracranial hemorrhages only when a prior CT is available for review. Rapid MRI is not adequate to replace CT in initial evaluation of intracranial hemorrhages but may be helpful in follow-up of known hemorrhages.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Suspected intracranial hemorrhage (ICH), usually in the setting of trauma, is a common indication for imaging in the pediatric population. Computed tomography (CT) is typically considered the first-line examination for these patients due to its availability, speed, and excellent sensitivity for acute blood products [1, 2]. However, CT requires exposure to radiation, which is of particular concern in the radiosensitive pediatric population [3]. Additionally, patients with ICH may undergo follow-up CT to evaluate for progressive hemorrhage, which results in cumulative radiation exposure. Standard magnetic resonance imaging (MRI) can effectively evaluate for hemorrhage without radiation [4–7], but it is a longer examination and frequently necessitates sedation in young patients. This limits access in the emergent setting and carries additional anesthesia risks.
In recent years, rapid MRI techniques (also known as fast MR, ultrafast MR, quick brain MRI, and MR ventricle exams) have gained increasing popularity for limited pediatric brain imaging. These studies typically consist of fast acquisition T2 weighted images, occasionally with additional sequences, which can be performed quickly and thus without the need for sedation. These techniques have proven valuable in certain instances, most notably in the evaluation of shunted hydrocephalus [8–13]. However, rapid imaging provides limited detail in comparison to a full MRI study. Several studies have noted the limitations of rapid MRI in detection of small lesions, as well as in evaluation for structural and migrational abnormalities, and its adequacy for other indications is uncertain [14–18].
In this study, we examine the sensitivity of rapid non-sedated MRI for both initial detection and follow-up evaluation of acute ICH in comparison to CT.
Materials and methods
Subjects
This was a retrospective study approved by the institutional review board. All rapid MRI studies performed at a tertiary pediatric hospital from 2009 through 2013 were reviewed for a clinical history of acute trauma or hemorrhage. Patients with a prior CT, either at our institution or performed at an outside institution and loaded onto a digital picture archiving and communications system (PACS) workstation, within 48 h of rapid MRI were selected. Patients were excluded in cases of interval neurosurgical procedure, inadequate CT imaging, or no identifiable hemorrhage by CT. Demographic data and clinical history were obtained from the electronic medical record.
Imaging technique
CT technique was variable as images from a variety of institutions were reviewed. All CT scans included non-contrast axial images from skull base through vertex. Reformatted images, when available, were also reviewed. Rapid MRI examinations were performed on either 1.5 Tesla (T) or 3 T scanners (Discovery 750, HDXT Signa scanners, GE Healthcare, Milwaukee, Wisconsin; Magnetom Avanto, Aera and Skyra scanners, Siemens, Erlangen, Germany) and included axial, sagittal, and coronal single-shot fast spin echo (SS-FSE) or half-Fourier acquisition single-shot turbo spin echo (HASTE) sequences for a total scan time of approximately 2–3 min. Representative parameters for 3 T studies were the following: matrix size 320 × 265, field of view 23 cm, TR2000, TE87, slice thickness 4–5 mm. Representative parameters for 1.5 T studies were as follows: matrix size 192 × 180, field of view 20 cm, TR1500, TE78, slice thickness 4–5 mm. Some exams also included axial gradient echo (GRE) sequences for an additional scan time of approximately 1 min with representative parameters as follows: 3 T: matrix size 320 × 218, field of view 20 cm, TR630, TE20, slice thickness 4–5 mm; 1.5 T: matrix size 256 × 200, field of view 18 cm, TR729, TE25, slice thickness 4–5 mm.
Image analysis
CT and rapid MRI studies were anonymized, and reviewed by two board certified pediatric neuroradiologists (M.R. and A.J.). For each rapid MR examination, one reviewer did not have the prior CT for comparison (blinded) and the other interpreted the exam in conjunction with the prior CT images (unblinded). A subset of patients had an optional GRE sequence performed in addition to the ultrafast T2 sequences as a part of the rapid MR protocol and were evaluated separately.
The presence, type, and size of ICH detected by rapid MRI were recorded. Hemorrhage categories included subdural hemorrhage (SDH), epidural hemorrhage (EDH), subarachnoid hemorrhage (SAH), intraventricular hemorrhage (IVH), and parenchymal hemorrhagic contusion. In many instances, hemorrhages were too small to distinguish between subdural and epidural, and thus SDH and EDH were considered together. SDH/EDH hemorrhages were measured in greatest width in the axial plane. The degree of motion degradation on CT, rapid T2 MRI, and GRE sequences was qualitatively assessed with a 4-point scale (0 = none; 1 = mild, 2 = moderate, 3 = severe).
Statistical analysis
Detection of hemorrhage (dichotomous) served as the primary outcome of interest for analyses, and degree of motion degradation (range 0 to 3) served as a secondary outcome measure of interest. Predictors of interest included the following: blinded vs. unblinded assessment, type of hemorrhage (extra-axial, subarachnoid, contusion), presence vs. absence of GRE sequence, and size of hemorrhage. Analyses employed a series of chi-squared tests for independence comparing categorical predictors with categorical outcome(s), McNemar’s tests for paired data, and Wilcoxon rank-sum tests/Kruskal-Wallis tests for size and degree of motion score. Results of chi-squared tests were compared with those of a generalized linear model (with logit link) for correlated data using generalized estimating equations since images within patient may be associated with one another. In determining predictive ability of size of hemorrhage in detection, analyses involved a logistic regression model with size as the sole predictor. All analyses assumed a 5 % level of significance and no corrections were made for multiple hypothesis tests.
Results
Sixty-one patients met the inclusion criteria of detectable ICH by CT, rapid MR study was performed within 48 h of CT, and there was no neurosurgical intervention during this time. There were 35 male and 26 female subjects, and the mean age was 2.4 years (range 1 day–22 years). The most common indication for imaging was trauma (45 falls, 4 blunt force objects to the head, 3 birth-related injury, 2 suspected non-accidental injuries, and 1 motor vehicle accident). Other indications included seizure (n = 3), cavernoma (n = 1), postlumbar puncture headache (n = 1), and headache with thrombocytopenia (n = 1). The average time interval between CT and MR imaging was 28 h and 43 min (range 2 h 59 m–46 h 1 m).
Of the 61 rapid MRI exams, 43 exams were performed at 1.5 T and 18 at 3 T. Thirty-six exams also included additional GRE sequences, which were analyzed as a subset. There were a total of 102 hyperdense, acute hemorrhages detected on CT, including 72 EDH/SDH, 20 SAH, and 10 parenchymal hemorrhagic contusions. The sensitivity of rapid MRI with ultrafast T2 images alone (blinded) and with prior CT for comparison (unblinded) are summarized in Table 1. Hemorrhage detection in the subset of exams containing GRE sequences in addition to ultrafast T2 images is summarized in Table 2.
Assuming CT as the gold standard, the overall sensitivity of ICH detection by rapid MRI T2 images alone was 54 %, which increased to 71 % with comparison to prior CT (p = 0.0004). Detection was only slightly higher with studies performed at 3 T, compared with 1.5 T (Table 3), but the difference was not statistically significant (p = 0.7671 for blinded, p = 0.8457 for unblinded).
The overall sensitivity of ICH detection by blinded rapid MRI with GRE was 76 %, which increased to 90 % for unblinded rapid MRI with GRE (p = 0.0114). When compared to rapid MRI without GRE, the addition of a GRE sequence significantly increased the overall detection rate for both blinded (54 versus 76 %, p = 0.0003) and unblinded readers (71 versus 90 %, p < 0.0001). Hemorrhages detected on rapid MRI and rapid MRI with GRE sequences for blinded and unblinded readers are summarized in Fig. 1.
The sensitivity for parenchymal hemorrhage was high, regardless of GRE sequences or prior CT availability (89–100 %). Subarachnoid hemorrhage was frequently not detectable by rapid MRI without GRE, even when the prior CT was available for comparison (sensitivity 25 % unblinded, 10 % blinded), but detection was significantly increased with GRE sequences (sensitivity 93 % unblinded, p = 0.0016, 71 % blinded, p = 0.0067). The sensitivity of SDH/EDH was significantly higher when the prior CT was reviewed (sensitivity 81 % unblinded versus 61 % blinded, p = 0.0010). The addition of GRE further increased this to 86 %, although this difference was not statistically significant.
The average size of SDH/EDH by CT was 5.7 mm (range 2–23 mm). The average size of SDH/EDH identified by rapid MRI was 6.3 mm (unblinded) and 6.8 mm (blinded). The average size of SDH/EDH missed by rapid MRI was significantly lower for both unblinded (mean 3.2 mm, p = 0.0015) and blinded (mean 4 mm, p = 0.0010) readers. SDH/EDH size was a statistically significant predictor of detection for both blinded and unblinded readers (Fig. 2). Every millimeter increase in size corresponded to an odds ratio for detection of 1.68 [(1.18, 2.39), p = 0.0042] for unblinded rapid MRI and an odds ratio of 1.39 [(1.19, 1.61), p < 0.0001], for blinded rapid MRI.
Two patients also demonstrated IVH on CT. Neither case was recognized by rapid T2 images alone, but both were identified with GRE sequences.
Motion degradation, scored from none (0) to severe (3), was significantly less for CT (mean 0.4) than for rapid MRI (mean 0.8) and GRE (mean 1.3, Kruskal-Wallis test p < .0001).
Of the 41 fractures detected by CT, rapid MRI identified only 11. One patient with hydrocephalus and five patients with mild midline shift were identified on both blinded and unblinded rapid MRI.
Discussion
Rapid MRI has been considered as an alternative to standard MRI or CT for evaluation of intracranial pathologies. This is particularly relevant in children who may require sedation for full-length MRI and are also more sensitive to the risks of ionizing radiation from CT. However, there is little data on the use of these limited exams for indications other than hydrocephalus. Interpretation of the literature is also confounded by variability in both terminology and techniques of rapid MRI. A recent study by Cohen et al. [19] suggested rapid MRI may be feasible to evaluate acute pediatric head trauma in the emergency room setting from a technical and resource utilization standpoint, but they did not evaluate the sensitivity of these studies. A prior study by Griffiths et al. [20] comparing rapid MRI with standard MR and CT in the diagnosis of acute neurologic conditions showed that rapid MRI detected the majority of intracranial pathology in acute neurosurgical admissions, with the exception of SAH, but did not describe the sensitivity for other ICH types. Of note, the rapid MRI technique in that study consisted of echo planar T1 and DWI images in addition to single-shot fast spin echo T2 sequences, but they did not include GRE images. Recently, a study by Mehta et al. [21] assessed rapid MRI, which included axial T2 FLAIR and DWI images in addition to GRE and multiplanar ultrafast T2 sequences, for the evaluation of pediatric head trauma. These investigators found an almost perfect concordance between rapid MR and CT detection of extra-axial hemorrhages, although the size of the hemorrhages was not referenced.
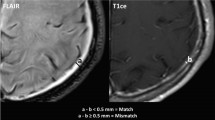
In our series, rapid MRI detected the majority of extra-axial hemorrhages when GRE sequences were used and the prior CT was available for review (Fig. 3). The sensitivity for SAH was poor with T2 images alone, in concordance with the results of Griffith et al., but significantly improved with the addition of GRE sequences (Fig. 4). Gradient sequences only mildly improved detection of SDH/EDH. In many instances, this may have been due to volume averaging with low signal of the skull and difficulty distinguishing small extra-axial hemorrhages from adjacent calvarium or scalp hematoma (Fig. 5). Rapid MRI detected nearly all parenchymal hemorrhagic contusions evident by CT, with or without additional GRE sequences, presumably due to the sensitivity of T2 weighted images for associated edema (Fig. 6). Overall hemorrhage detection did not appear substantially increased in cases performed at 3 T compared to 1.5 T studies. Although this could be due to the small 3 T sample size, it is also possible that higher magnet field strength does not significantly aid in distinguishing T2 hypointense blood products from adjacent T2 hypointense calvarium in cases of small hemorrhages.
The overall high sensitivity for ICH by rapid MRI when used to follow up positive CT findings in our study is similar to Mehta et al. and lends support to the potential role of rapid MR for assessment of intracranial trauma. However, it should be noted that, in our series, the size of the SDH/EDH was a significant predictor for detection. Although none of the patients with missed ICH required neurosurgical intervention, small collections were not reliably identified, even when the prior CT was reviewed for comparison and most fractures were not recognized by rapid MRI. Rapid MRI would be unlikely to fail to detect a neurosurgically relevant collection, but in some instances, such as evaluation for abusive head trauma, trace hemorrhages may still be of critical importance and could be missed by this technique. Additionally, although the SDH/EDH detection was high when the prior CT was available for comparison, the sensitivity was only modest in the absence of CT for comparison. This suggests that although rapid MRI may be helpful in reevaluation of known ICH documented by prior CT, this technique is not adequate to replace CT as an initial screening examination for head trauma.
The utility of repeat imaging of ICH in the absence of neurologic deterioration has been debated, particularly in pediatric patients where assessment of neurologic status may be more challenging, but there is also a greater concern for the effects of cumulative radiation [22–24]. However, in practice, repeat head CTs in pediatric patients with ICH appear to be frequently performed for routine follow up [25, 26]. Rapid MR could provide a safe modality for reevaluation, without radiation or anesthetic risks.
There are several limitations to this study. As with many pediatric studies, the sample size is relatively small. Patients with interval procedures, such as hematoma evacuation, were excluded from the study, creating a bias for patients with less significant head trauma. There also may be an unknown selection bias regarding which patients received rapid MRI follow-up in contrast to those who had no repeat imaging or follow-up CT. Additionally, this study assumes CT as the gold standard for ICH and that hemorrhages did not substantially change in size during between CT and MR imaging. Progressive hemorrhage or redistribution of blood products would affect comparisons between CT and rapid MRI. As only positive CT cases were included, the specificity of rapid MRI and the possibility that rapid MRI could be more sensitive for some types of hemorrhage or contusion than CT is cannot be assessed here. Additionally, rapid MR studies consisted only of ultrafast T2 and, in some instances, GRE sequences. Other fast MR sequences, such as fast FSE FLAIR images, have been employed in some rapid MR imaging protocols and could potentially provide superior detection (21). Thinner (3 mm) slices may also have increased detection, although increasing the slice number and sequences would result in some increased imaging time. As noted in the statistical Materials and methods section, analyses involved simple chi-squared tests; however, failure to account for potential within-patient association across images may result in misleading statistical inference and interpretation. To mitigate this limitation, the simpler, more intuitive chi-squared results were compared with that of the more complex generalized estimating equation results, and all major inferences and interpretations remained comparable. It should be noted, however, that the sensitivities reported should be viewed as estimates since observations are not necessarily independent. In addition, no corrections were made for multiple statistical hypothesis tests since these analyses were deemed exploratory.
Conclusion
Rapid MRI may be useful as an alternative to CT in the follow up of known acute ICH in the pediatric population. Non-sedated rapid MRI sequences demonstrated a high sensitivity for CT-positive acute ICH when the prior CT was available for comparison. The addition of GRE sequences significantly increased the detection of ICH and should be included in rapid MRI techniques for hemorrhage evaluation. However, the more modest sensitivity of rapid MRI for hemorrhage in the absence of prior CT and limited detection of very small extra-axial collections suggests that this technique is not adequate for initial evaluation of head trauma.
References
Datta S, Stoodley N, Jayawant S, Renowden S, Kemp A (2005) Neuroradiological aspects of subdural haemorrhages. Arch Dis Child 90:947–951
Kemp AM, Rajaram S, Mann M et al (2009) What neuroimaging should be performed in children in whom inflicted brain injury (iBI) is suspected? A systematic review. Clin Radiol 64:473–483
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505
Kidwell CS, Chalela JA, Saver JL et al (2004) Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA 292:1823–1830
Roguski M, Morel B, Sweeney M et al (2015) Magnetic resonance imaging as an alternative to computed tomography in select patients with traumatic brain injury: a retrospective comparison. J Neurosurg Pediatr 15:529–534
Liang L, Korogi Y, Sugahara Y et al (1999) Detection of intracranial hemorrhage with susceptibility-weighted MR sequences. AJNR 20:1527–1534
Buttram SD, Garcia-Filion P (2015) Computed tomography vs magnetic resonance imaging for identifying acute lesions in pediatric traumatic brain injury. Hosp Pediatr 5:79–84
Niederhauser BD, McDonald RJ, Keating GF et al (2013) Retrospective review of rapid pediatric brain MR imaging at an academic institution including practice trends and factors affecting scan times. AJNR 2013:1836–1840
Ashley WW, McKinstry RC, Leonard J, Smyth MD, Lee BC, Park TS (2015) Use of rapid-sequence magnetic resonance imaging for evaluation of hydrocephalus in children. J Neurosurg 103:124–130
Koral K, Blackburn T, Bailey AA, Koral KM, Anderson J (2012) Strengthening the argument for rapid brain MR imaging: estimation of reduction in lifetime attributable risk of developing fatal cancer in children with shunted hydrocephalus by instituting a rapid brain MR imaging protocol in lieu of head CT. AJNR 33:1851–1854
Iskandar BJ, Sansone JM, Medow J, Rowley HJ (2004) The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg 101:147–151
Patel D, Tubbs R (2014) Fast-sequence MRI studies for surveillance imaging in pediatric hydrocephalus. J Neurosurg Pediatr 13:440–447
Yue EL, Meckler GD, Fleischman RJ (2015) Test characteristics of quick brain MRI for shunt evaluation in children: an alternative modality to avoid radiation. J Neurosurg Pediatr 15:420–426
Ba-Ssalamah A, Schick S, Heimberger K et al (2000) Ultrafast magnetic resonance imaging of the brain. Magn Reson Imaging 18:237–243
Patel MR, Klufas RA, Alberico RA, Edelman RR (1997) Half-Fourier acquisition single-shot turbo spin-echo (HASTE) MR: comparison with fast spin-echo MR in diseases of the brain. AJNR 18:1635–1640
Penzkofer AK, Pfluger T, Pochmann Y, Meissner O, Leinsinger G (2002) MR imaging of the brain in pediatric patients: diagnostic value of HASTE sequences. AJR 179:509–514
Singh RK, Smith JT, Wilkinson ID, Griffiths PD (2003) Ultrafast MR imaging in pediatric neuroradiology. Acta Radiol 44:550–557
Missios S, Quebada PB, Forero JA (2008) Quick-brain magnetic resonance imaging for nonhydrocephalus indications. J Neurosurg 103:438–444
Cohen AR, Caruso P, Duhaime AC, Klig GE (2015) Feasibility of “rapid” magnetic resonance imaging in pediatric acute head injury. Am J Emerg Med 33:887–890
Griffiths PD, Wilkinson ID, Patel MC et al (2000) Acute neuromedical and neurosurgical admissions standard and ultrafast MR imaging of the brain compared with cranial CT. Acta Radiol 41:401–409
Mehta H, Acharya J, Mohan AL, Tobias ME, LeCompte L, Jeevan D (2016) Minimizing radiation exposure in evaluation of pediatric head trauma: use of rapid MR imaging. AJNR 37:1–8
Givner A, Gurney J, O’Connor D, Kassarjian A, LaMorte WW, Moulton S (2002) Reimaging in pediatric neurotrauma: factors associated with progression of intracranial injury. J Pediatr Surg 37:381–385
Chwals WJ, Robinson AV, Sivit CJ, Alaedeen D, Fitzenrider E, Cizmar L (2008) Computed tomography before transfer to a level I pediatric trauma center risks duplication with associated increased radiation exposure. J Pediatr Surg 43:2268–2272
Howe J, Fitzpatrick CM, LaKam DR, Gleisner A, Vane DW (2014) Routine repeat brain computed tomography in all children with mild traumatic brain injury may result in unnecessary radiation exposure. J Trauma Acute Care Surg 76:292–295
Da Silva PS, Reis ME, Aguiar VE (2008) Value of repeat cranial computed tomography in pediatric patients sustaining moderate to severe traumatic brain injury. J Trauma 65:1293–1297
Figg RE, Stouffer CW, Vander Kolk WE, Connors RH (2006) Clinical efficacy of serial computed tomographic scanning in pediatric severe traumatic brain injury. Pediatr Surg Int 22:215–218
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that this manuscript does not contain clinical studies or patient data.
Conflict of interest
We declare that we have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ryan, M.E., Jaju, A., Ciolino, J.D. et al. Rapid MRI evaluation of acute intracranial hemorrhage in pediatric head trauma. Neuroradiology 58, 793–799 (2016). https://doi.org/10.1007/s00234-016-1686-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-016-1686-x