Abstract
Purpose
Pharmacogenomics investigates interindividual genetic variability in the DNA sequence of drug targets, drug-metabolizing enzymes or disease genes, RNA expression, or protein translation of genes affecting drug response and drug safety. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most commonly prescribed medications with well-documented variation in patient response in terms of efficacy and safety. This variation may in part be explained by pharmacogenomics.
Methods
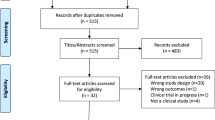
In this paper I review data on the pharmacogenomics of aspirin and other NSAIDs focusing on clinical implications.
Results
Existing scientific evidence supports the pharmacogenomic basis of interindividual variation in treatment response to aspirin and NSAIDs, with clinical implications for antiplatelet action, cancer chemoprevention, and drug safety. However, further research efforts are needed before knowledge on the pharmacogenomics of aspirin and NSAIDs can be implemented in clinical practice.
Conclusion
The outcome of these research efforts would be anticipated to have added value for both science and society, contributing to the enhanced efficacy and safety of these agents through patient selection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interindividual variation in treatment response to standard doses of drug therapy can lead to treatment failure or to life-threatening adverse drug reactions among patients receiving identical doses of the same drug. A drug’s activity is the result of its interaction with the proteins involved in absorption, distribution, metabolism, and elimination (ADME proteins) and the molecular drug targets or target pathways. Genetic variation in these proteins, i.e., single nucleotide polymorphisms (SNPs) in genes coding for metabolizing enzymes or drug transporters, might have a significant influence on the drug effect. Pharmacogenomics investigates interindividual genetic variability in the DNA sequence of drug targets, drug-metabolizing enzymes, and disease genes, RNA expression, or protein translation of genes affecting drug response and drug safety [1].
Although clinical trials that include thousands of patients may generally indicate the efficacy and lack of toxicity of the drugs being tested, it is well known that it is not possible to predict a priori whether an individual patient will respond to a given medication without adverse effects. Individual variability in drug response can be explained by a number of parameters, including age, sex, weight, pharmacokinetics, disease severity, concomitant diseases, and environmental factors. Moreover, genetic differences among individuals in drug metabolism and/or cellular drug targets may explain a significant component of this variability [2]. Interindividual variability in drug metabolism in particular is a major cause of adverse drug effects. In many cases, such variability is linked to polymorphisms in genes coding for drug-metabolizing enzymes resulting in null variant alleles or variant alleles that code proteins with increased or reduced activity. Individuals carrying enzyme-inactivating mutations display impaired drug metabolism. Thus, when treated at standard doses, carriers of inactivating mutations have higher plasma drug concentrations and lower clearance rates, rendering them susceptible to adverse drug reactions [3]. Aspirin and other nonsteroidal anti-inflammatory drugs/agents (NSAIDs) are among the most commonly prescribed medications with well-documented variation in patient response in terms of efficacy and safety. This variation may in part be explained by pharmacogenomics. In this paper, I review data on the pharmacogenomics of aspirin and other NSAIDs, focusing on clinical implications.
Pharmacogenomics and acetylsalicylic acid
Antiplatelet therapy with aspirin represents the cardinal therapeutic strategy for the prevention of atherothrombotic events in patients with acute coronary syndromes and those with percutaneous coronary interventions. However, it is known that there is great variation in the antiplatelet effect of aspirin, and this variation could be partly be explained by pharmacogenetic variation. A number of polymorphisms have been associated with cardiovascular outcomes, leading to the suggesting that these polymorphisms modulate the antiplatelet effect of aspirin. However, most of the data have been contradictory. In this context, polymorphisms in the genes encoding glycoproteins (i.e., IIb/IIIa, Ia/IIa, VI, and Ibα), cyclooxygenases (COX1 and COX2), adenosine diphosphate receptors (P2Y1 and P2Y12) and proteins involved in hemostasis (i.e., thromboxane A2 receptor, coagulation factor XIII) have been investigated [4]. Of these, the most intensively studied polymorphism to date is the PlA1/A2 polymorphism in the GPIIIa platelet receptor. Studies in healthy humans have suggested that carriers of P2Y(12) ADP receptor polymorphisms may be at increased risk of experiencing cardiovascular events. However, Bierend et al. demonstrated that the platelet response to acetylsalicylic acid is independent of the presence or absence of P2Y(12) ADP receptor polymorphisms in patients with stable coronary artery disease who have had their first myocardial infarction [5]. Alternatively, based on the results of their systematic review of the pharmacogenetics of aspirin resistance, Goodman et al. [6] concluded that while literature data support a genetic association between the PlA1/A2 molecular variant and aspirin resistance in healthy subjects, the effect diminishes markedly in the presence of cardiovascular disease. This difference between the healthy population and cardiovascular disease patients was attributed to the effect of co-medications on platelet function, i.e., a degree of platelet inhibition by statins obscures the presence of aspirin resistance. These authors also suggested that the presence of heterogeneity in the methods used for the measurement of aspirin resistance could have an additional effect on the outcomes [6]. Recent studies have shown that specific COX1 A-842G, C50T, and GPIIIa PLA1/A2 genetic polymorphisms that are frequently observed in Caucasians are not commonly in patients from mainland China. In Chinese population, the presence of the P2Y1 893CC genotype appears to confer an attenuated antiplatelet effect during aspirin treatment in healthy Chinese volunteers [7].
Acetylsalicylic acid is metabolized by UDP-glucuronosyltransferase 1A6 (UGT1A6) and cytochrome P450 2C9 (CYP2C9), and interindividual differences in the activity of these enzymes have been implicated in aspirin resistance as well as in the safety of antiplatelet doses of acetylsalicylic acid. One particularly relevant study investigated whether interindividual variability in the UGT1A6 or CYP2C9 gene is related to the prevalence of gastric complaints in hospitalized cardiovascular patients using acetylsalicylic acid for secondary prevention of ischemic heart disease. No association was found between polymorphisms in the genes encoding for aspirin-metabolizing enzymes and gastric complaints in this cohort of patients [8].
The regular use of aspirin and NSAIDs also has a protective effect on the incidence of colon neoplasia. However, this protective effect can be modulated by genomic variation. Bigler et al. were the first group to investigate the influence of the CYP2C9 and UGT1A6 genotypes on the effect of aspirin on colon adenoma risk [9]. These authors found that variations in genotype modified the risk among aspirin users. An assessment of colon adenoma risk in users and nonusers based on either the CYP2C9 or the UGT1A6 genotype revealed an inverse association with aspirin only for individuals who were homozygous wild-type for CYP2C9 or those who carried a variant UGT1A6 allele. However, contrary to the results obtained for aspirin users, an inverse association was observed between nonaspirin NSAID use and colon adenoma risk regardless of genotype [9]. Chan et al. conducted a nested case–control study of 1,062 women who provided blood specimens and detailed data on aspirin use before undergoing lower endoscopy, with the aim of investigating whether polymorphisms in the UGT1A6 enzyme modulate the protective benefit of regular aspirin use on colorectal adenoma. These authors concluded that the UGT1A6 genotype affects the chemopreventive effect of aspirin on colorectal adenoma risk [10].
Pharmacogenomics and other NSAIDs
Nonsteroidal anti-inflammatory drugs/agents are some of the most widely prescribed and over-the-counter medications. At least 16 different registered NSAIDs are at least partially metabolized by CYP2C9. These include aceclofenac, acetylsalicylic acid, azapropazone, celecoxib, diclofenac, frurbiprofen, ibuprofen, indomethacin, lornoxicam, mefenamic acid, meloxicam, naproxen, phenylbutazone, piroxicam, and tenoxicam [11–22]. Two common variants of the CYP2C9 gene (CYP2C9*2 and *3) have been reported to significantly lower the activity of the CYP2C9 enzyme. These two alleles differ from the wild-type CYP2C9*1 allele by a single point mutation. CYP2C9*2 is characterized by a 430C >T exchange in exon 3 resulting in an Arg144Cys amino acid substitution, while CYP2C9*3 is characterized by a 1075A >T exchange in exon 7 causing an lle359leu substitution in the catalytic site of the enzyme. Significant intergenotypic differences have been reported in the pharmacokinetics of celecoxib, flurbiprofen, ibuprofen, and tenoxicam which could potentially be translated into dose recommendations based upon CYP2C9 genotype [22]. In contrast, an effect of CYP2C9 genotype on the pharmacokinetics of naproxen, ketoprofen, and sulindac has not been reported.
The pharmacokinetics of celecoxib has been investigated in humans genotyped for CYP2C9. Celecoxib has been one of the first drugs for which the manufacturer’s drug information recommends caution when celecoxib is administered to poor metabolizers of CYP2C9 substrates, as they could have abnormally high levels [22].
Diclofenac is metabolized through glucuronidation and hydroxylation. More than 50 % of diclofenac is metabolized to 4-hydroxydiclofenac via CYP2C9. CYP2C9 polymorphisms do not affect the pharmacokinetics of diclofenac [22]. CYP2C8 is involved in diclofenac 5-hydroxylation.
CYP2C8 polymorphisms may influence interindividual variability in the pharmacokinetics of ibuprofen and diclofenac [23–26]. In the case of ibuprofen, it has been shown that polymorphisms in CYP2C8 significantly change the clearing capacity of individuals who are heterozygous or homozygous for mutants of this metabolizing enzyme.
Pharmacogenomics of NSAIDs and gastrointestinal bleeding
The presence of the CYP2C9 variant alleles CYP2C9*2 and *3 has been associated with acute gastrointestinal hemorrhage due to NSAIDs. Pilotto et al. conducted a relevant case–control study that included 26 patients with endoscopically documented NSAID-related gastroduodenal bleeding lesions and 52 controls with no lesions at endoscopy [27]. The participants of both groups were Helicobacter pylori negative and acute users of a NSAID or COX-2 inhibitor that undergoes CYP2C9 metabolism (i.e., celecoxib, diclofenac, ibuprofen, naproxen, or piroxicam). Two marker SNPs in the CYP2C9 gene, identified as the CYP2C9 *2 and *3 allele, were evaluated. Significantly higher frequencies of CYP2C9*1/*3 [34.6 vs. 5.8 %; P < 0.001, odds ratio (OR) 12.9, 95 % confidence interval (CI) 2.917–57.922] and CYP2C9*1/*2 (26.9 vs. 15.4 %; P = 0.036, OR 3.8, 95 % CI 1.090–13.190) were identified in bleeding versus control patients [27]. In 2003, acute gastrointestinal bleeding was reported in a 71-year-old patient under long-term treatment with acenocoumarol, after treatment with indomethacin. Upon genotyping, the patient was found to be homozygous for the CYP2C9*3 allele, and the authors suggested that the interaction of genetically impaired metabolism of indomethacin and acenocoumarol, as well as a putative interaction in the metabolism of both CYP2C9 substrates, was the cause of bleeding [28]. Following this case report, Martínez et al. published the first case–control study that investigated the effect of CYP2C9 polymorphisms in NSAID-induced gastrointestinal bleeding. The results of their study demonstrated that the carriers of CYP2C9 variant alleles were more prone to develop acute gastrointestinal bleeding when they received NSAIDs that were CYP2C9 substrates [3].
Not only CYP2C9 polymorphisms but also CYP2C8 polymorphisms have been implicated in NSAID-induced gastrointestinal hemorrhage. CYP2C9*2 is in partial linkage disequilibrium with CYP2C8*3, and many NSAIDs are substrates for both enzymes. In a cross-sectional study of NSAID users (n = 134 bleeding cases, n = 177 nonbleeding controls), Blanco et al. investigated whether CYP2C9 and CYP2C8 polymorphisms were associated with gastrointestinal bleeding [29]. The frequencies of the CYP2C8*3 and CYP2C9*2 alleles were higher in NSAID users who experienced a bleeding event versus those that did not (CYP2C8*3: OR 3.4, P < 0.002; CYP2C9*2: OR 2.7, P = 0.013). Further analysis of the data revealed that the highest bleeding risk was in patients who possessed both of the variant CYP2C8*3 and CYP2C9*2 alleles. The authors hypothesized that CYP2C8*3 and CYP2C9*2 alleles conferred an increased risk of gastrointestinal bleeding due to decreased metabolic clearance and increased plasma concentrations of NSAIDs [29].
Pharmacogenomics of NSAIDs and hepatotoxicity
Diclofenac has been associated with rare, but serious hepatotoxicity [30]. Although the mechanism of diclofenac-induced hepatotoxicity has not yet been elucidated, it is hypothesized that diclofenac adducts are formed through either the 5-hydroxydiclofenac metabolic pathway or the UGT2B7 glucuronidation pathway. These adducts seem to play a role in the pathogenesis of diclofenac-induced hepatotoxicity through the covalent modification of proteins, resulting in alteration of protein function or in induction of the immune response [31]. Relevant studies have demonstrated that the CYP2C9 genotype is not associated with the risk of diclofenac-induced hepatitis [31]. Daly et al. designed a case–control study to investigate the effect of CYP2C8 polymorphisms on the risk of diclofenac hepatotoxicity [32]. Cases were 24 patients who had experienced diclofenac hepatotoxicity, and controls were 160 patients who had received diclofenac without developing hepatotoxicity. All patients were genotyped for the CYP2C8*3 and *4 alleles. The authors found that CYP2C8 polymorphisms could not predict the risk of hepatotoxicity. In contrast, genes involved in the metabolism and biliary excretion of diclofenac (i.e., UGT2B7 and ABCC2, respectively) were associated with diclofenac hepatotoxicity [32] .
Pharmacogenomics NSAIDs and chemoprevention
The effect of the CYP2C9 genotype on colorectal adenoma risk was investigated by Chan et al. in individuals with CYP2C9*2 and CYP2C9*3 genotypes in the Adenoma Prevention with Celecoxib trial [33]. Following adenoma removal, patients were assigned randomly to groups given placebo or low-dose (200 mg, twice-daily) or high-dose (400 mg, twice-daily) celecoxib and underwent follow-up colonoscopies at 1 and/or 3 years. The authors observed a pharmacogenetic association between the CYP2C9*3 variant genotype and the risk of adenoma according to celecoxib dosing—i.e., the greater efficacy of high-dose celecoxib, compared with low-dose celecoxib, in preventing colorectal adenoma remained confined to individuals with slow-metabolizer (CYP2C9*3) genotypes [33]. In another study, Samowits et al. investigated the interactions between CYP2C9 and UGT1A6 polymorphisms and NSAIDs in colorectal cancer prevention. These authors determined the UGT1A6 and CYP2C9 genotypes in 2,295 individuals with colorectal cancer and in 2,903 controls, as well as interactions between these genotypes with aspirin or ibuprofen use and colorectal cancer risk. According to the data, variant CYP2C9 genotypes enhanced the protective effect of ibuprofen on the prevention of colorectal cancer. However, no interaction was found between the variant CYP2C9 genotype and aspirin use, nor between the UGT1A6 genotype with either NSAID [34]. On the other hand, in another study, no evidence of interaction was found between polymorphisms in CYP2C8, CYP2C9, UGT1A6, PPARdelta, and PPARgamma and the protective effect of regular NSAID use on the risk of colorectal carcinoma [35]
Discussion
Aspirin and other NSAIDs are among the most commonly prescribed medications, with indications ranging from pain treatment to secondary prevention of cardiovascular events and cancer chemoprevention. It is well known that aspirin and other NSAIDs are multi-target agents, and these drugs are currently being investigated for novel therapeutic indications. In addition, these agents are often implicated in serious adverse events. At the same time, interindividual variation in the efficacy and safety of these agents is well recognized.
The findings reported in this review indicate that pharmacogenomics could explain a part of this variation. However, the reader should be well aware that this article is not a systematic review, but rather a critical review based on studies that focus on the clinical relevance of the pharmacogenomics of aspirin and NSAIDs. Most of the studies cited herein include a limited number of genotyped persons taking one dose of the drug. Based on these data, dose recommendations cannot be suggested. In addition, it is important to take into account that many pathways contribute to the overall clearance of NSAID. Thus, further research efforts are needed before our knowledge on the pharmacogenomics of aspirin and NSAIDs can be implemented in clinical practice. It is anticipated that the outcome of these research efforts will be of added value for science and society by contributing to the enhanced efficacy and safety of these agents through patient selection.
Conclusion
Current evidence suggests that pharmacogenomics explain in part the variation in efficacy and safety of aspirin and NSAIDs. However, research is needed before dose recommendations can be implemented in clinical practice.
References
Evans W (1999) Translating functional genomics into rational therapeutics. Science 286:487–491
Siva C, Yokoyama WM, McLeod HL (2002) Pharmacogenetics in rheumatology: the prospects and limitations of an emerging field. Rheumatology 41:1273–1279
Martínez C, Blanco G, Ladero JM, García-Martín E, Taxonera C, Gamito FG, Diaz-Rubio M, Agúndez JA (2004) Genetic predisposition to acute gastrointestinal bleeding after NSAIDs use. Br J Pharmacol 141:205–208
Würtz M, Kristensen SD, Hvas AM, Grove EL (2012) Pharmacogenetics of the antiplatelet effect of aspirin. Curr Pharm Des 18:5294–5308
Bierend A, Rau T, Maas R, Schwedhelm E, Böger RH (2008) P2Y12 polymorphisms and antiplatelet effects of aspirin in patients with coronary artery disease. Br J Clin Pharmacol 65:540–547
Goodman T, Ferro A, Sharma P (2008) Pharmacogenetics of aspirin resistance: a comprehensive systematic review. Br J Clin Pharmacol 66:222–223
Li Q, Chen BL, Ozdemir V, Ji W, Mao YM, Wang LC, Lei HP, Fan L, Zhang W, Liu J, Zhou HH (2007) Frequency of genetic polymorphisms of COX1, GPIIIa and P2Y1 in a Chinese population and association with attenuated response to aspirin. Pharmacogenomics 8:577–578
van Oijen MG, Huybers S, Peters WH, Drenth JP, Laheij RJ, Verheugt FW, Jansen JB (2005) Polymorphisms in genes encoding acetylsalicylic acid metabolizing enzymes are unrelated to upper gastrointestinal health in cardiovascular patients on acetylsalicylic acid. Br J Clin Pharmacol 60:623–628
Bigler J, Whitton J, Lampe JW, Fosdick L, Bostick RM, Potter JD (2001) CYP2C9 and UGT1A6 genotypes modulate the protective effect of aspirin on colon adenoma risk. Cancer Res 61:3566–3569
Chan AT, Tranah GJ, Giovannucci EL, Hunter DJ, Fuchs CS (2005) Genetic variants in the UGT1A6 enzyme, aspirin use, and the risk of colorectal adenoma. J Natl Cancer Inst 97:457–460
Hamman MA, Thompson GA, Hall SD (1997) Regioselective and stereoselective metabolism of ibuprofen by human cytochrome P450 2C. Biochem Pharmacol 54:33–41
Duggan DE, Hogans AF, Kwan KC, McMahon FG (1972) The metabolism of indomethacin in man. J Pharmacol Exp Ther 181:563–575
Zarza J (2003) Major bleeding during combined treatment with indomethacin and low doses of acenocoumarol in a homozygous patient for 2C9*3 variant of cytochrome P-450 CYP2C9. Thromb Haemost 90:161–162
Brenner SS, Herrlinger C, Dilger K, Mürdter TE, Hofmann U, Marx C, Klotz U (2003) Influence of age and cytochrome P450 2C9 genotype on the steady-state disposition of diclofenac and celecoxib. Clin Pharmacokinet 42:283–292
Kirchheiner J, Meineke I, Steinbach N, Meisel C, Roots I, Brockmoller J (2003) Pharmacokinetics of diclofenac and inhibition of cyclooxygenases 1 and 2: no relationship to the CYP2C9 genetic polymorphism in humans. Br J Clin Pharmacol 55:51–61
Yasar U, Eliasson E, Forslund-Bergengren C, Tybring G, Gadd M, Sjöqvist F, Dahl ML (2001) The role of CYP2C9 genotype in the metabolism of diclofenac in vivo and in vitro. Eur J Clin Pharmacol 57:729–735
Kirchheiner J, Tsahuridu M, Jabrane W, Roots I, Brockmoller J (2004) The CYP2C9 polymorphism: from enzyme kinetics to clinical dose recommendations. Personalized Med 1:63–84
Miners JO, Coulter S, Tukey RH, Veronese ME, Birkett DJ (1996) Cytochromes P450, 1A2, and 2C9 are responsible for the human hepatic O-demethylation of R- and S-naproxen. Biochem Pharmacol 51:1003–1008
Zhao J, Leemann T, Dayer P (1992) In vitro oxidation of oxicam NSAIDS by a human liver cytochrome P450. Life Sci 51:575–581
Hutzler JM, Kolwankar D, Hummel MA, Tracy TS (2002) Activation of CYP2C9-mediated metabolism by a series of dapsone analogs: kinetics and structural requirements. Drug Metab Dispos 30:1194–1200
Martínez C, Blanco G, García-Martín E, Agúndez JA (2006) Clinical pharmacogenomics for CYP2C8 and CYP2C9: general concepts and application to the use of NSAIDs. Farm Hosp 30:240–248
Kirchheiner J, Seeringer A (2007) Clinical implications of pharmacogenetics of P450 drug metabolising enzymes. Biochim Biophys Acta 1770:489–494
Tang W (2003) The metabolism of diclofenac—enzymology and toxicology perspectives. Curr Drug Metab 4:319–329
Kumar S, Samuel K, Subramanian R, Braun MP, Stearns RA, Chiu SH, Evans DC, Baillie TA (2002) Extrapolation of diclofenac clearance from in vitro microsomal metabolism data: role of acylglucuronidation and sequential oxidative metabolism of the acyl glucuronide. J Pharmacol Exp Ther 303:969–978
Martínez C, García-Martín E, Blanco G, Gamito FJ, Ladero JM, Agúndez JA (2005) The effect of the cytochrome P450 CYP2C8 polymorphism on the disposition of (R)-ibuprofen enantiomer in healthy subjects. Br J Clin Pharmacol 59:62–69
García-Martín E, Martínez C, Tabares B, Frías J, Agúndez JA (2004) Interindividual variability in ibuprofen pharmacokinetics is related to interaction of cytochrome P450 2C8 and 2C9 amino acid polymorphisms. Clin Pharmacol Ther 76:119–127
Pilotto A, Seripa D, Franceschi M, Scarcelli C, Colaizzo D, Grandone E, Niro V, Andriulli A, Leandro G, Di Mario F, Dallapiccola B (2007) Genetic susceptibility to nonsteroidal anti-inflammatory drug-related gastroduodenal bleeding: role of cytochrome P450 2C9 polymorphisms. Gastroenterology 133:465–471
Zarza Z (2003) Major bleeding during combined treatment with indomethacin and low doses of acenocoumarol in a homozygous patient for 2C9*3 variant of cytochrome P-450 CYP2C9. Thromb Hemost 90:161–162
Blanco G, Martinez C, Ladero JM, Garcia-Martin E, Taxonera C, Gamito FG, Diaz-Rubio M, Agundez JA (2008) Interaction of CYP2C8 and CYP2C9 genotypes modifies the risk for nonsteroidal anti-inflammatory drugs-related acute gastrointestinal bleeding. Pharmacogenet Genomics 18:37–43
de Abajo FJ, Montero D, Madurga M, Garcia Rodriguez LA (2004) Acute and clinically relevant drug-induced liver injury: a population based case–control study. Br J Clin Pharmacol 58:71–80
Aithal GP, Day CP, Leathart JB, Daly AK (2000) Relationship of polymorphism in CYP2C9 to genetic susceptibility to diclofenac-induced hepatitis. Pharmacogenetics 10:511–518
Daly AK, Aithal GP, Leathart JB, Swainsbury RA, Dang TS, Day CP (2007) Genetic susceptibility to diclofenac-induced hepatotoxicity: contribution of UGT2B7, CYP2C8, and ABCC2 genotypes. Gastroenterology 132:272–281
Chan AT, Zauber AG, Hsu M, Breazna A, Hunter DJ, Rosenstein RB, Eagle CJ, Hawk ET, Bertagnolli MM (2009) Cytochrome P450 2C9 variants influence response to celecoxib for prevention of colorectal adenoma. Gastroenterology 136:2127.e1–2136.e1
Samowitz WS, Wolff RK, Curtin K, Sweeney C, Ma KN, Andersen K, Levin TR, Slattery ML (2006) Interactions between CYP2C9 and UGT1A6 polymorphisms and nonsteroidal anti-inflammatory drugs in colorectal cancer prevention. Clin Gastroenterol Hepatol 4:894–901
McGreavey LE, Turner F, Smith G, Boylan K, Timothy Bishop D, Forman D, Roland Wolf C, Barrett JH, Colorectal Cancer Study Group (2005) No evidence that polymorphisms in CYP2C8, CYP2C9, UGT1A6, PPARdelta and PPARgamma act as modifiers of the protective effect of regular NSAID use on the risk of colorectal carcinoma. Pharmacogenet Genomics 15:713–721
Conflict of interest
None.
Sources of funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yiannakopoulou, E. Pharmacogenomics of acetylsalicylic acid and other nonsteroidal anti-inflammatory agents: clinical implications. Eur J Clin Pharmacol 69, 1369–1373 (2013). https://doi.org/10.1007/s00228-013-1477-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-013-1477-9