Abstract
Klinefelter Syndrome (KS) patients, defined by a 47 XXY karyotype, have increased risk of fragility fractures. We have assessed bone microarchitecture by high resolution peripheral quantitative CT (HR-pQCT) at the radius and tibia in young KS patients, naïve from testosterone replacement therapy (TRT). Areal bone mineral density (BMD) and body composition were assessed by dual X-ray absorptiometry (DXA). Total testosterone (tT) was measured at baseline. Bone measurements have been repeated after 30 months of TRT. We enrolled 24 KS patients and 72 age-matched controls. KS patients were (mean ± SD) 23.7 ± 7.8 year-old. KS patients had significantly lower relative appendicular lean mass index (RALM) and lower aBMD at spine and hip than controls. Ten patients (42%) had low tT level (≤ 10.4 nmol/L). At baseline, we observed at radius a marked cortical (Ct) impairment reflected by lower Ct.area, Ct.perimeter, and Ct.vBMD than controls. At tibia, in addition to cortical fragility, we also found significant alterations of trabecular (Tb) compartment with lower trabecular bone volume (BV/TV) and Tb.vBMD as compared to controls. After 30 months of TRT, 18 (75%) KS patients were reassessed. Spine aBMD and RALM significantly increased. At radius, both cortical (Ct.Pm, Ct.Ar, Ct.vBMD, Ct.Th) and trabecular (Tb.vBMD) parameters significantly improved. At tibia, the improvement was found only in the cortical compartment. Young TRT naïve KS patients have inadequate bone microarchitecture at both the radius and tibia, which can improve on TRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Klinefelter syndrome (KS) is a congenital condition due to an extra X chromosome (47 XXY). Despite being the most frequent sex chromosome disorder (1/660 male births), it is frequently under-diagnosed [1]. Patients have substantial morphotypic symptoms that are inconsistently present such as tall stature, broad hips, narrow shoulders, sparse body hair, gynecomastia, and small testes with azoospermia leading to infertility [2]. KS patients also have an increased risk of fracture with higher morbidity and mortality [3, 4]. KS patient bone phenotype has been essentially explored by areal bone mineral density (aBMD) [5]. The increased fracture risk may be related to lower aBMD, as previously reported in cross sectional studies [6,7,8,9,10,11,12,13,14,15,16]. It is estimated that 42.4% of the KS patients present with osteopenia and osteoporosis [17], but this finding is not constant [18,19,20]. This raises the possibility of impairment in bone quality in addition to the decrease of aBMD. Bone histology reports of KS patients are scarce. In humans, Delmas and Meunier reported histomorphometric analysis of iliac crest biopsies in 5 KS patients. They found rarefied spongy bone and a strong reduction of osteoblastic activity with decreased osteoid thickness and low appositional rate [21]. A reduced bone volume has also been found in the XXY mice model but not the osteoblastic depression [22]. In 3D µCT, these mice displayed reduced trabecular thickness [22].
High-resolution peripheral quantitative computed tomography (HR-pQCT) allows for non invasive bone microarchitecture analysis and distinguishes the trabecular and cortical compartments. Up to now, only one cross-sectional study using HR-pQCT has been performed in KS patients. This study found impaired cortical and trabecular compartments at the tibia in KS patients [23]. Nevertheless, this study included a large proportion of patients previously treated with testosterone replacement therapy (TRT) that may have affected their bone phenotype. Thus, the description of bone microarchitecture in TRT-naïve KS patients remains timely, along with the determination of the effect of TRT on bone microarchitecture.
We therefore conducted a study to assess bone microarchitecture by HR-pQCT in TRT-naïve non-mosaic KS patients, and prospectively examined its evolution over 30 months of TRT.
Subjects and Methods
Participants
FERTIPRESERVE is a clinical research program lead (IP) in Lyon, France (NCT01918280). This program, started in 2012, aims to preserve fertility in KS patients with low sperm count. It has been approved by the local ethics committee “Comité de Protection des Personnes Lyon Sud-Est II—CHU de Lyon, France” (study number 2010-017-2 on June 17th 2010 with amendments on September 9th 2015 and October 10th 2017). The study has been performed in agreement with the Helsinki Declarations of 1975 and 1983. All patients, and parents in case of minors, provided written consent for the study. To be included in FERTIPRESERVE, patients had to be aged ≥ 16 years, have a Tanner score > 5 and a homogenous karyotype assessed on 200 cells. Exclusion criteria were other impaired spermatogenesis causes such as testicular medical history (torsion, radiotherapy, trauma, or orchitis), and medical history of any treatment with gonadal toxicity, including chemotherapy, psychotropic and neuroleptic drugs. Patients with a personal history of bone disease (e.g. Paget bone disease, osteomalacia, primary hyperparathyroidism…) were also excluded. Briefly, in FERTIPRESERVE, before any hormonal TRT, young KS patients were proposed to undergo a surgical testicular biopsy to extract mature spermatozoids by the Testicular Sperm Extraction (TESE) method. The spermatozoids obtained were frozen in liquid nitrogen for future in vitro fertilization via Intra Cytoplasmic Sperm Injection (ICSI) [24]. Once testicular biopsy had been performed, patients underwent the bone evaluation and then received TRT. A second bone evaluation was proposed after 30 months on TRT. The current analysis has been approved by the national data protection commission (CNIL). For this bone analysis, each KS patient was aged-matched (± 1 year) to 3 healthy controls from French male cohorts (STRAMBO for adults [25], and VITADOS, NTC01832623, for teenagers [26].
Clinical Evaluation and Testosterone Replacement Therapy
At baseline, body weight and height were measured using calibrated scale and height gauge. Personal and familial history of fracture, and lifestyle habits were recorded. Leisure physical activity, current smoking, alcohol consumption (occasional, moderate 1–3 units/day, > 3 units/day) were self-reported. Once TRT had been introduced, patients were regularly followed-up in outpatient clinics (IP) as recommended by the Endocrine Society clinical practice guideline [27]. TRT used injectable testosterone enantate (Bayer®) 250 mg/1 mL by intramuscular injection that was delivered according to the following routine protocol. Initiation of treatment was performed at a dose of 0.2 mL weekly during the first month, subsequently increased to a dose of 0.3 mL. After 6 months of this regimen, injections were performed every 15 days with an adjusted dose ranging between 0.3 and 0.5 mL to maintain plasma testosterone level within the normal range of the laboratory for young men (total testosterone > 12 nmol/L and bioavailable testosterone between 2.25 and 10.7 nmol/L). Biological controls of total testosterone (tT) and bioavailable testosterone (bio-T) were carried out, before and 48 h after the injection, at 3 and 6 months and then every 6 months.
Dual-Energy X-ray Absorptiometry (DXA)
Areal BMD was measured by DXA (Discovery®, Hologic, Inc., Waltham, MA, US) at the total hip, femoral neck and lumbar spine. The CV of daily measurements of the Hologic phantom was 0.35%. Whole body composition was also assessed by DXA; relative appendicular lean mass index (RALM) corresponded to the sum of lean mass of both arms and legs divided by (body height)2. DXA was performed at baseline and repeated after 30 months of TRT.
Bone Microarchitecture
Volumetric Bone Mineral Density (vBMD) and microarchitecture were assessed at the non-dominant distal radius and right distal tibia by HR-pQCT (XtremeCT-1®, Scanco Medical, Brüttisellen, Switzerland) at baseline [28].
Obtained cortical parameters were: cortical vBMD (Ct.vBMD), cortical perimeter (Ct.Pm), cortical area (Ct.Ar) and cortical thickness (Ct.Th). Ct.Th was calculated as the cortical volume divided by the outer bone surface.
Regarding trabecular compartment, we obtained trabecular vBMD (Tb.Vbmd) and trabecular bone volume (BV/TV) assuming fully mineralized bone to have mineral density of 1200 mg HA/cm3. Trabecular elements were identified by the mid-axis transformation, and the distance between them was assessed by the 3D distance transformation (Tb.Sp). Trabecular number (Tb.N, 1/mm) was defined as the inverse of Tb.Sp. Trabecular thickness (Tb.Th, µm) was derived from BV/TV and Tb.N. Intra-individual distribution of Tb.Sp (Tb.Sp.SD, µm) reflects heterogeneity of trabecular network and was quantified using the standard deviation of the distance between the mid-axes.
After 30 months of TRT, bone microarchitecture was reassessed. To ensure a reliable analysis during longitudinal analysis, strict positioning rules are used to perform acquisition. Member (leg or forearm) is placed in a brace with a fixed position. The new scout view is systematically compared to the baseline printed one to correctly replace the region of analysis. Only HR-pQCT slices with at least 80% of common volume of interest between baseline and follow-up acquisitions were used to perform the longitudinal analysis as previously described [29].
Controls and patients were assessed in a single bone research center (Inserm UMR1033, Hôpital Edouard Herriot, Lyon, France) on the same HR-pQCT and DXA machines with regular calibration overtime to ensure reliable and fully comparable data among patients and during follow-up. Controls from VITADOS cohort were assessed contemporaneously to the KS patients (2013–2015) and STRAMBO cohort were measured between 2006 and 2008.
Serum Measurements
At baseline, before any testicular surgery, a fasting-state blood sample was drawn from KS patients at 8 a.m. Serum was stored at − 80 °C. Standard bone laboratory tests were performed using the routine procedure. Total testosterone was measured by tritiated radioimmunoassay (RIA) after diethylether extraction with a lower limit of detection of 0.06 nmol/L and inter-assay coefficient of variation (CV) ≤ 10%. Bioavailable testosterone was assayed by RIA after ammonium sulfate precipitation. Total 17β-estradiol was measured by RIA with a detection limit of 17 pmol/L and an inter-assay CV ≤ 8%. Hypogonadism cut-off for each parameter was defined according to the normal values in our laboratory: 10.4 nmol/L for tT, 2.25 nmol/L bio-T, and 66.0 pmol/L for 17βE2.
Statistical Analysis
All calculations were performed using R version 3.4.4 software (Copyright 2017 The R Foundation for Statistical Computing). The distribution of variables was assessed using the Shapiro–Wilk’s test. Tb.Sp and Tb.Sp.SD had skewed distribution and were log-transformed. At baseline, comparisons between patients with KS and controls were performed using the Student t-test for continuous variables. Patients with KS were stratified according to: age, steroids (tT and bio-T), RALM (median = 7.61 kg/m2), fat mass (median = 22.5%) and growth plate status. Each stratum was compared to the controls using the Dunett–Hsu test. A paired Student t-test was used to compare aBMD and bone microarchitecture between baseline and follow-up time points. Data are presented as mean ± SD, or median (interquartile range, IQR). Statistical significance was set at p < 0.05.
Results
Baseline Characteristics
Between February 2014 and November 2015, a total of 33 KS patients were screened. All patients entered the care pathway through infertility. Most of the time, infertility was associated with low body hair and muscle mass. Among these, 9 were excluded (8 had previously received in the past significant amount of TRT, 1 had a mosaic mutation) so 24 patients were included in the bone substudy. KS patients were age-matched with 72 male controls (66 from the STRAMBO cohort and 6 from the VITADOS cohort).
The mean ± SD age of KS patients was 23.7 ± 7.8 years (see age distribution in Supplemental 4A) and the mean BMI was normal (20.9 ± 3.4 kg/m2). Body weight, height and BMI did not differ significantly between cases and controls. One patient had a personal history of fragility fracture (non-traumatic wrist fracture during adolescence). Among KS patients, 11 (46%) practiced regular physical activity, and 11 (46%) were current smokers. None of the patients received calcium-vitamin D supplementation. The mean ± SD level of tT was 11.5 ± 5.3 nmol/L, that of bio-T was 2.0 ± 1.1 nmol/L, and that of 17βE2 was 61.5 ± 33 pmol/L (Table 1).
Bone Mass and Bone Microarchitecture
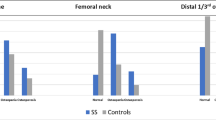
KS patients had significantly lower aBMD at lumbar spine, femoral neck, and total hip (p < 0.001 for each) than controls. KS patients also had a significantly lower RALM (p < 0.001) and greater proportion of fat mass (p < 0.001; Table 2). This is all the more true that the KS patients are hypogonadal (Table 3).
At the distal radius, we observed a marked cortical deterioration with lower Ct.Ar, Ct.Pm, and Ct.vBMD, as compared to controls. At the tibia, in addition to cortical fragility, we also found a significant impairment of trabecular parameters with lower BV/TV and Tb.vBMD (Table 4).
Hypogonadism and Bone Microarchitecture
Ten (42%) and 15 (63%) patients were hypogonadal according to tT and bio-T. At the radius, testosterone hypogonadal patients had significantly lower cortical parameters (CtPm, Ct.Ar) than control patients whereas eugonadal patients had not (Table 5). There were no significant trabecular differences. In contrast, at the tibia, tT hypogonadal patients not only displayed lower cortical parameters but also lower BV/TV and lower Tb.vBMD parameters than controls. KS patients with normal tT had only significant lower cortical parameters in comparison to controls (Table 5). These results were independent of muscle mass since all differences remained statistically significant after adjustment for RALM.
Muscle Mass, Fat Mass, and Bone Microarchitecture
At both skeletal sites, patients with low RALM (Table 6) had impaired cortical parameters in comparison to controls. In addition, at the tibia, patients with low RALM had also lower Tb.vBMD compared to the controls. All comparisons remained significant after adjustment for bio-T.
At the radius, there was no difference according to fat mass group (Supplemental Table S1). At the tibia, all KS patients had lower Tt.vBMD and Ct.Th. The phenotype was even more severe in the high fat mass group with a significant reduction of BV/TV, Ct.vBMD and Tb.vBMD.
Change in Bone Microarchitecture After Testosterone Replacement Therapy
A total of 18 KS patients (75%) were reassessed after median of 30.4 (29.7–31.0) months of TRT. Others declined. Over this period, none of them underwent any fragility fracture. aBMD increased significantly at the lumbar spine (0.949 g/cm2 ± 0.11 to 0.993 g/cm2 ± 0.11; p < 0.01) but no significant change was observed at the femoral neck (p = 0.38). During this period, there was also a significant increase in muscle mass (RALM from 7.53 ± 1.28 to 8.02 ± 1.42 kg/m2 (p < 0.01)).
At the radius, both the trabecular and cortical compartments significantly improved on TRT. At the tibia, the improvement was found only in the cortical compartment (Ct.Ar, Ct.vBDM, Ct.Th) (Table 7).
Regarding hypogonadism (hypogonadal patients with tT ≤ 10.4 nmol/L vs eugonadal patients tT > 10.4 nmol/L), a significant gain was observed at both sites (radius and tibia) in both groups on TRT. Nevertheless, the gain looks larger in the hypogonadal group (Table 7).
To take into account the young age of our KS patients, growth plates were scored at baseline into three groups (Supplemental 2). The subgroup of patients with fully closed growth plate (N = 14 at radius and N = 9 at tibia) still presented a significant increase in bone microarchitecture parameters. Supplemental 3A. Furthermore, patients with open growth plate experimented on TRT a significant larger increase of bone microarchitecture parameters than the one with closed growth plate. Supplemental 3B.
Bone microarchitecture parameters were not so much different—except the Ct vBMD- at baseline between the youngest KS patients (< 20) and the oldest one (≥ 20 years old). Nevertheless, the bone parameters absolute variations tended to be higher in youngest group than in the oldest one. Supplemental 4 B and 4C.
Discussion
We described for the first time the bone microarchitecture in TRT naïve young KS patients and its evolution on TRT treatment. We found that young adult KS patients did not achieve cortical mass and architecture comparable with the age-matched healthy controls. At the tibia, trabecular bone was also impaired. After 30 months of TRT, patients experienced at both sites an improvement of their aBMD, RALM and cortical bone status. The trabecular bone status also improved at the radius. Altogether, these data suggest a benefit of TRT treatment in young adult KS patients for a better bone health.
One issue may be the risk of supraphysiologic testosterone serum levels on TRT. Testosterone was administrated every 2 weeks. The choice of intermittent regimen rhythm limits supraphysiologic testosterone levels. Moreover, patients were clinically evaluated at initiation and during follow-up to look for “supraphysiologic” symptoms such as aggressiveness and sexual compulsions. In addition, total testosterone and bioavailable testosterone were assessed before injection and at the peak (48 h after injection). Therapeutic objectives were to obtain testosterone levels at physiologic levels (total testosterone between 10 and 24 nmol/L and bioavailable testosterone between 2.25 and 10.70 nmol/L). Estradiol level was also assessed and no excessive serum level (< 100 pmol/L) was observed under TRT. We believe that this monitoring of TRT in KS patients reduce as much as possible the risk of over testosterone replacement in patients.
Our results are consistent with the reduced bone volume observed in XYY mice [19]. They are also consistent with microarchitecture data reported by Shanbogue et al. who conducted a cross sectional study in 31 KS patients aged 35.8 ± 8.2 years [23]. In addition to their findings, we observed an impaired bone geometry in our cohort (significantly lower Ct.Pm and Ct.Ar). The difference may stem from distinct study populations because more than two-thirds of their population (21/31) had previously received TRT [23], and we presently show that bone microarchitecture of KS patients is particularly sensitive to TRT. Moreover, our study highlights the precocity of bone alterations that are already present in these young otherwise healthy KS patients without fracture. The greater differences observed here in this young group of KS patients may suggest a delayed peak bone mass acquisition in these patients.
Regarding longitudinal analysis, to the best of our knowledge, there is no other study in humans investigating the change in bone microarchitecture after TRT. The only available data were obtained using aBMD [10, 30] or total vBMD [8]. Interestingly, it seems that TRT did not improve aBMD [7, 18, 31] except if initiated before the age of attainment of peak bone mass [13], supporting early TRT treatment for these patients to optimize bone architecture and peak bone mass. Herein, after a median 30 months on TRT, our patients experienced a significant increase in Ct.Pm, Ct.Th and Ct.vBMD at both skeletal sites and a significant decrease in Tb.Ar. These findings suggest that the observed bone gain during TRT may be related to both endocortical apposition and periostal apposition.
The FERTIPRESERVE project is in line with the Endocrine Society clinical practice guideline for TRT in men with hypogonadism [27] and the recent guidelines of the European Academy of Andrology (EAA) on KS [32]. These guidelines, by their holistic approach of the KS from birth to adulthood and from pathophysiology to comorbidities, are a major contribution to the field. The guidelines recommend to introduce TRT not before the end of adolescence and after treatment of fertility disorders by semen collection, cryopreservation or even testicular biopsy for TESE [32]. The recommendations stress the importance of vitamin D supplementation and suitable calcium intake. They also highlight that patients with KS are at risk of low bone mineral density and fractures independently of their serum levels of testosterone. Our bone sub-protocol echoes to the lack of bone data underlined by the guidelines [27, 32]. The major contribution of our study is to describe the bone microarchitecture in a very homogenous group of non treated young adult KS patients and to follow their response to TRT. We have observed that independently of their hormonal status, the whole group benefit from the TRT, even if the gain was larger in the hypogonadal group. This finding provide new data to discuss in the next KS guidelines since the current ones restrict TRT introduction to hypogonadal patients after fertility consideration.
Mechanisms underlying bone fragility in KS patients remain unclear. First, we observed that bone alterations were more severe in hypogonadal KS patients suggesting that sex steroid deficit may play an important role. In KS patients, tT serum levels are normal in prepubertal boys, but increase inadequately during puberty, leading to hypogonadism in 65–85% of adults [33]. In our patient group, less than half of the KS patients were tT hypogonadal which was less than expected for a KS population [33]. This may be due to the young age of the included patients, since testicular function declines with age in KS patients after puberty [34]. Indeed, testicular failure is observed during puberty, with hyalinization and fibrosis of seminiferous tubes, leading to small testes and spermatogenesis failure and hypoleidigism with a reduction of androgen secretion despite an elevated secretion of LH. Our finding that the most severe bone alterations were present in hypogonadal patients, is in line with earlier studies that investigated the association between tT and bone parameters measured via aBMD [9,10,11, 29, 35]. Nevertheless, it was not the case for the studies using aBMD reported by Bojesen et al. [36], and Ferlin et al. [17], or the study reported by Wong et al. using QCT [37].
Total testosterone, includes biologically inactive testosterone bound to Sex Hormone Binding Globulin (SHBG). Unfortunately, data on free testosterone, bioavailable testosterone (bio-T), or 17β-estradiol (17βE2) and bone in these KS patients are scarce. Except a few studies [10, 12, 18, 36], most of them [7,8,9, 13, 17, 23, 30, 31, 35, 38] only assess the relationship between aBDM or bone microarchitecture and tT. Therefore, we also measured bio-T. The deterioration of bone microarchitecture of bio-T hypogonadal KS patients was in line with the results of tT but more profoundly impaired suggesting that the assessment of bio-T may be relevant in future studies.
Estradiol is also a key component of bone health in males since estrogen play a major role in bone physiology during puberty and in preventing bone loss in aging healthy men. In KS patients, some studies found normal [12, 36, 39] or elevated 17βE2 levels [17, 18, 40, 41] compared to controls. Herein, nearly three-quarters of patients had decreased 17βE2 concentrations beside their increased fat mass. However, this might be expected since concentrations of 17βE2 and bio-T are strongly correlated; 85% of estradiol comes from peripheral aromatization of testosterone [42]. Thus, TRT may act directly on cortical apposition through testosterone and indirectly on endocortical apposition through estradiol. Interestingly, Shanbogue et al. found a positive association between 17βE2 and Ct.Th at the radius and Tt.vBMD at the tibia, but not with tT [23] which supports the role of both bio-T and 17βE2 in these patients.
Because some KS patients had normal sex steroid levels, other mechanisms may be responsible for bone fragility. This is supported by an in vivo study from Liu et al. [22], where the XXY mice did not fully recovered a normal bone phenotype when treated by TRT. In our cohort, we also observed a partial bone improvement since at the tibia, all patients on TRT improved, whereas at the radius, the improvement was mainly observed in hypogonadal KS patients. The discrepancy between the two sites radius and tibia provides a clue for further investigation to explore the role of mechanical loading in KS patients. Furthermore, as reported with aBMD [36], microarchitecture deterioration was also more severe in KS patients with low RALM suggesting that muscle has a significant role in sustaining bone microarchitecture in these patients. In another cohort of both KS and patients with anorchia, lower RALM was associated with poorer Ct.Ar and Ct.Th at the tibia as assessed by QCT [37]. After TRT, our patients had a significant increase of RALM. This is consistent with a double-blind placebo-controlled randomized trial of TRT for 6 months, that found a significantly increased muscle mass and decreased fat mass in 274 older hypogonadal men [43]. An indirect effect of TRT on the impaired muscle/fat ratio [19, 36] is possible but has never been fully explored.
In addition to its association with testosterone, bone-muscle crosstalk may be involved not only through its mechanical effect (load and strength applied). The potential involvement of dystrophin, present on X chromosome, has never been studied in KS patients. Further investigations on bone-muscle interactions in KS might be helpful.
Other genetic aspects should also be considered. It has been described that some KS patients present a substantial genetic variation of Androgen Receptor (AR) gene with repeated CAG polymorphisms of the first exon. This is of interest since CAG length is inversely proportional to the AR function and that the X chromosome with fewer CAG polymorphisms is preferentially inactivated [44]. AR function may therefore be reduced and thus explaining bone fragility despite normal levels of sex steroids. Selective inactivation of the shorter X chromosome may also be responsible of a lower bone response to TRT [45, 46].
Regarding bone turnover, serum biomarkers in young KS patients naïve from TRT are scarce but worth to be shown. The limited number of patients and the absence of controls in our study prevent too much interpretation. Nevertheless, the data we observed were in the normal range of our laboratory and we did not observe any trend between hypogonadal (low tT) and eugonadal patients. In the literature, Bojeson et al. have also assessed bone turnover markers in 70 KS patients and 71 controls. No difference was observed suggesting that KS patients, at least through classical serum biomarkers evaluation, had no bone turnover alteration [36].
The present study has some limitations. Sex steroid measurements were only measured at baseline and were performed by RIA. At that time LC–MS was not routinely available in our Institution. Because of insufficient materials, we were able to re-assess only some patients by LC–MS. In these low value range, results are consistent (R2 = 0.93) between the two technics. This is in line with the comparative test between RIA and LC–MS performed in 180 patients to set the method (Supplemental 5). Thus, we remain confident in our findings. Hip aBMD was not available in the controls from the VITADOS cohort. Indeed, VITADOS cohort did not plan hip aBMD since it enrolled children down to 12 years old with still bone immaturity. In addition, because of the image acquisition protocol used for HR-pQCT, measurement site may vary with arm and leg length at baseline. Another bias in this longitudinal study of a young population could be related to re-positioning, which was minimized by recruiting only patient with Tanner stage V or more that do not grow anymore. Finally, our study remains an exploratory research work on bone microarchitecture in KS patients. We acknowledge that bone microarchitecture is an intermediate criterion that does not totally recapitulate general bone health of subjects and that our study was not design to explore fracture events. We observed that even in a homogenous population of young, never treated, non-mosaic KS patients, there were some microarchitecture heterogeneity among patients. Growth plate status, testosterone serum level, and age were important contributors for baseline status and evolution on TRT. The small sample size of the subgroups and the absence of control group call for further studies and preclude from drawing firm conclusions to treat patients. For the moment, physicians should still stick to the current guidelines.
In conclusion, we found that TRT-naïve without mosaics KS patients have an early bone impairment at both radius and tibia, that is more severe when they are hypogonadal and/or with low muscle mass. TRT over a median 30 months, in addition to the previously known benefits, also improves bone microarchitecture at both skeletal sites. Our findings suggest a beneficial effect of an early TRT initiation in KS patients to optimize their peak bone mass acquisition and improve their bone microarchitecture. Nevertheless, this is uncontrolled data involving a difficult analysis of longitudinal HR-pQCT data and with possible confounders such as the young age of some subjects without full skeletal maturity. Further studies of early TRT vs placebo are required to clarify the natural gain expected in these patients and the boost effect provided by TRT.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Forti G, Corona G, Vignozzi L, Krausz C, Maggi M (2010) Klinefelter’s syndrome: a clinical and therapeutical update. Sex Dev 4(4–5):249–258
Groth KA, Skakkebæk A, Høst C, Gravholt CH, Bojesen A (2013) Clinical review: Klinefelter syndrome—a clinical update. J Clin Endocrinol Metab 98(1):20–30
Swerdlow AJ, Higgins CD, Schoemaker MJ, Wright AF, Jacobs PA (2005) United Kingdom Clinical Cytogenetics Group. Mortality in patients with Klinefelter syndrome in Britain: a cohort study. J Clin Endocrinol Metab 90(12):6516–6522
Bojesen A, Juul S, Birkebæk N, Gravholt CH (2004) Increased mortality in Klinefelter Syndrome. J Clin Endocrinol Metab 89(8):3830–3834
Pizzocaro A, Vena W, Condorelli R, Radicioni A, Rastrelli G, Pasquali D, Selice R, Ferlin A, Foresta C, Jannini EA et al (2020) Testosterone treatment in male patients with Klinefelter syndrome: a systematic review and meta-analysis. J Endocrinol Investig 43(12):1675–1687
Stepan JJ, Burckhardt P, Hána V (2003) The effects of three-month intravenous ibandronate on bone mineral density and bone remodeling in Klinefelter’s syndrome: the influence of vitamin D deficiency and hormonal status. Bone 33(4):589–596
van den Bergh JP, Hermus AR, Spruyt AI, Sweep CG, Corstens FH, Smals AG (2001) Bone mineral density and quantitative ultrasound parameters in patients with Klinefelter’s Syndrome after long-term testosterone substitution. Osteoporos Int 12(1):55–62
Behre HM, Kliesch S, Leifke E, Link TM, Nieschlag E (1997) Long-term effect of testosterone therapy on bone mineral density in hypogonadal men. J Clin Endocrinol Metab 82(8):2386–2390
Horowitz M, Wishart JM, O’Loughlin PD, Morris HA, Need AG, Nordin BE (1992) Osteoporosis and Klinefelter’s syndrome. Clin Endocrinol 36(1):113–118
Choi HR, Lim SK, Lee MS (1995) Site-specific effect of testosterone on bone mineral density in male hypogonadism. J Korean Med Sci 10(6):431–435
Foresta C, Ruzza G, Mioni R, Meneghello A, Baccichetti C (1983) Testosterone and bone loss in Klinefelter syndrome. Horm Metab Res 15(1):56–57
Hiéronimus S, Lussiez V, Le Duff F, Ferrari P, Bständig B, Fénichel P (2011) Klinefelter’s syndrome and bone mineral density: is osteoporosis a constant feature? Ann Endocrinol 72(1):14–18
Kübler A, Schulz G, Cordes U, Beyer J, Krause U (1992) The influence of testosterone substitution on bone mineral density in patients with Klinefelter’s syndrome. Exp Clin Endocrinol Diabetes 100(3):129–132
Stagi S, Cavalli L, Cavalli T, de Martino M, Brandi ML (2016) Peripheral quantitative computed tomography (pQCT) for the assessment of bone strength in most of bone affecting conditions in developmental age: a review. Ital J Pediatr. https://doi.org/10.1186/s13052-016-0297-9
Devogelaer JP, De Cooman S, de Deuxchaisnes CN (1992) Low bone mass in hypogonadal males. Effect of testosterone substitution therapy, a densitometric study. Maturitas 15(1):17–23
Smith DA, Walker MS (1977) Changes in plasma steroids and bone density in Klinefelter’s Syndrome. Calcif Tissue Res 22:225–228
Ferlin A, Schipilliti M, Vinanzi C, Garolla A, Di Mambro A, Selice R, Lenzi A, Foresta C (2011) Bone mass in subjects with Klinefelter Syndrome: role of testosterone levels and androgen receptor gene CAG polymorphism. J Clin Endocrinol Metab 96(4):E739–E745
Luisetto G, Mastrogiacomo I, Bonanni G, Pozzan G, Botteon S, Tizian L, Galuppo P (1995) Bone mass and mineral metabolism in Klinefelter’s syndrome. Osteoporos Int 5(6):455–461
Aksglaede L, Molgaard C, Skakkebaek NE, Juul A (2008) Normal bone mineral content but unfavourable muscle/fat ratio in Klinefelter Syndrome. Arch Dis Child 93(1):30–34
Vena W, Pizzocaro A, Indirli R, Amer M, Maffezzoni F, Delbarba A, Leonardi L, Balzarini L, Ulivieri FM, Ferlin A et al (2020) Prevalence and determinants of radiological vertebral fractures in patients with Klinefelter Syndrome. Andrology 8(6):1699–1704
Delmas P, Meunier PJ (1981) Osteoporosis in Klinefelter’s syndrome Quantitative bone histological data in 5 cases and relationship with hormonal deficiency (author’s transl). Nouv Presse Med 10(9):687–690
Liu PY, Kalak R, Lue Y, Jia Y, Erkkila K, Zhou H, Markus JS, Wang C, Swerdloff RS, Dunstan CR (2010) Genetic and hormonal control of bone volume, architecture, and remodeling in XXY mice. J Bone Miner Res 25(10):2148–2154
Shanbhogue VV, Hansen S, Jørgensen NR, Brixen K, Gravholt CH (2014) Bone geometry, volumetric density, microarchitecture, and estimated bone strength assessed by HR-pQCT in Klinefelter Syndrome. J Bone Miner Res 29(11):2474–2482
Tournaye H, Liu J, Nagy Z, Verheyen G, Van Steirteghem A, Devroey P (1996) The use of testicular sperm for intracytoplasmic sperm injection in patients with necrozoospermia. Fertil Steril 66(2):331–334
Chaitou A, Boutroy S, Vilayphiou N, Munoz F, Delmas PD, Chapurlat R, Szulc P (2010) Association between bone turnover rate and bone microarchitecture in men: the STRAMBO study. J Bone Miner Res 25(11):2313–2323
Bacchetta J, Ginhoux T, Bernoux D, Dubourg L, Ranchin B, Roger C (2019) Assessment of mineral and bone biomarkers highlights a high frequency of hypercalciuria in asymptomatic healthy teenagers. Acta Paediatr 108(12):2253–2260
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM, Snyder PJ, Swerdloff RS, Wu FC, Yialamas MA (2018) Testosterone therapy in men with hypogonadism: an endocrine society* clinical practice guideline. J Clin Endocrinol Metab 103(5):1715–1744
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90(12):6508–6515
Szulc P, Boutroy S, Chapurlat R (2018) Prediction of fractures in men using bone microarchitectural parameters assessed by high-resolution peripheral quantitative computed tomography—the prospective STRAMBO study. J Bone Miner Res 33(8):1470–1479
Haider A, Meergans U, Traish A, Saad F, Doros G, Lips P, Gooren L (2014) Progressive improvement of T-scores in men with osteoporosis and subnormal serum testosterone levels upon treatment with testosterone over six years. Int J Endocrinol 2014:496948
Wong FH, Pun KK, Wang C (1993) Loss of bone mass in patients with Klinefelter’s Syndrome despite sufficient testosterone replacement. Osteoporos Int 3(1):3–7
Zitzmann M, Aksglaede L, Corona G, Isidori AM, Juul A, T’Sjoen G, Kliesch S, D’Hauwers K, Toppari J, Słowikowska-Hilczer J (2021) European academy of andrology guidelines on Klinefelter Syndrome endorsing organization: European Society of Endocrinology. Andrology 9(1):145–167
Lee YS, Cheng AWF, Ahmed SF, Shaw NJ, Hughes IA (2007) Genital anomalies in Klinefelter’s syndrome. Hormone Res Paediatr 68(3):150–155
Ferlin A, Schipilliti M, Di Mambro A, Vinanzi C, Foresta C (2010) Osteoporosis in Klinefelter’s Syndrome. Mol Hum Reprod 16(6):402–410
Seo JT, Lee JS, Oh TH, Joo KJ (2007) The clinical significance of bone mineral density and testosterone levels in Korean men with non-mosaic Klinefelter’s Syndrome. BJU Int 99(1):141–146
Bojesen A, Birkebæk N, Kristensen K, Heickendorff L, Mosekilde L, Christiansen JS, Gravholt CH (2011) Bone mineral density in Klinefelter Syndrome is reduced and primarily determined by muscle strength and resorptive markers, but not directly by testosterone. Osteoporos Int 22(5):1441–1450
Wong SC, Scott D, Lim A, Tandon S, Ebeling PR, Zacharin M (2015) Mild deficits of cortical bone in young adults with Klinefelter Syndrome or anorchia treated with testosterone. J Clin Endocrinol Metab 100(9):3581–3589
Eulry F, Bauduceau B, Lechevalier D, Magnin J, Flageat J, Gautier D (1993) Early spinal bone loss in Klinefelter syndrome. X-ray computed tomographic evaluation in 16 cases. Rev du Rhumat Ed Française 60(4):287–291
Bojesen A, Kristensen K, Birkebaek NH, Fedder J, Mosekilde L, Bennett P, Laurberg P, Frystyk J, Flyvbjerg A, Flyvbjerg A (2006) The metabolic syndrome is frequent in Klinefelter’s Syndrome and is associated with abdominal obesity and hypogonadism. Diabetes Care 29(7):1591–1598
Kanakis GA, Nieschlag E (2018) Klinefelter Syndrome: more than hypogonadism. Metabolism 86:135
Lanfranco F, Kamischke A, Zitzmann M, Nieschlag E (2004) Klinefelter’s Syndrome. Lancet 364(9430):273–283
Gennari L, Nuti R, Bilezikian JP (2004) Aromatase activity and bone homeostasis in men. J Clin Endocrinol Metab 89(12):5898–5907
Srinivas-Shankar U, Roberts SA, Connolly MJ, O’Connell MDL, Adams JE, Oldham JA, Wu FC (2010) Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab 95(2):639–650
Beilin J, Ball EM, Favaloro JM, Zajac JD (2000) Effect of the androgen receptor CAG repeat polymorphism on transcriptional activity: specificity in prostate and non-prostate cell lines. J Mol Endocrinol 25(1):85–96
Zitzmann M, Depenbusch M, Gromoll J, Nieschlag E (2004) X-chromosome inactivation patterns and androgen receptor functionality influence phenotype and social characteristics as well as pharmacogenetics of testosterone therapy in Klinefelter patients. J Clin Endocrinol Metab 89(12):6208–6217
Bojesen A, Hertz JM, Gravholt CH (2011) Genotype and phenotype in Klinefelter syndrome—impact of androgen receptor polymorphism and skewed X inactivation. Int J Androl 34(6 Pt 2):e642–e648
Acknowledgements
The authors thank Y Bourgin, C Coutisson, B Dancer, D Foesser, N Paquin, C Planckaert, N Trehet-Mendel and V Ripoll for their help to conduct the study. The authors thank François Duboeuf (INSERM UMR 1033) for extracting data on body composition. The authors thank Dr M. Proriol for her advice on growth plate aspect. The authors thank P Robinson (Hospices Civils de Lyon) for editing corrections. This study was supported by a non restricted Research Grant from Roche-Chugai to CC.
Funding
This study was supported by a non restricted Research Grant from Roche-Chugai Pharmaceutical (CC). An institutional funding for the VITADOS cohort was provided by the Programme Hospitalier de Recherche Clinique Inter-régional (PHRCi AURA) (J Bacchetta, 2011).
Author information
Authors and Affiliations
Contributions
Study design: IP, SB and CC. Study conduct: IP and CC. Data collection: IP, SA, SB, JB, HL and CC. Data analysis: AP, CC, MP, PS. Data interpretation: AP, CC, PS. Drafting manuscript: AP, CC, PS. Revising manuscript content: IP, SA, SB, JB, HL and RC. Approving final version of manuscript: AP, PS, IP, SA, SB, JB, HL, RC and CC. AP and CC take responsibility for the integrity of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
A. Piot, I. Plotton, S. Boutroy, J. Bacchetta, S. Ailloud, H. Lejeune, R. D. Chapurlat, P. Szulc and C. B. Confavreux declare that they have no conflict of interest concerning this study.
Ethical Approval
It has been approved by the local ethics committee “Comité de Protection des Personnes Lyon Sud-Est II—CHU de Lyon, France” (study number 2010-017-2 on June 17th 2010 with amendments on September 9th 2015 and October 10th 2017). The study has been performed in agreement with the Helsinki Declarations of 1975 and 1983.
Informed Consent
All patients, and parents in case of minors, provided written consent for the study.
Human and Animal Rights statement
The authors certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Piot, A., Plotton, I., Boutroy, S. et al. Klinefelter Bone Microarchitecture Evolution with Testosterone Replacement Therapy. Calcif Tissue Int 111, 35–46 (2022). https://doi.org/10.1007/s00223-022-00956-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-022-00956-2