Abstract
Summary
Sheehan’s syndrome (SS) is a rare but well-characterized cause of hypopituitarism. Data on skeletal health is limited and on microarchitecture is lacking in SS patients.
Purpose
We aimed to explore skeletal health in SS with bone mineral density (BMD), turnover, and microarchitecture.
Methods
Thirty-five patients with SS on stable replacement therapy for respective hormone deficiencies and 35 age- and BMI-matched controls were recruited. Hormonal profile and bone turnover markers (BTMs) were measured using electrochemiluminescence assay. Areal BMD and trabecular bone score were evaluated using DXA. Bone microarchitecture was assessed using a second-generation high-resolution peripheral quantitative computed tomography.
Results
The mean age of the patients was 45.5 ± 9.3 years with a lag of 8.3 ± 7.2 years prior to diagnosis. Patients were on glucocorticoid (94%), levothyroxine (94%), and estrogen–progestin replacement (58%). None had received prior growth hormone (GH) replacement. BTMs (P1NP and CTX) were not significantly different between patients and controls. Osteoporosis (26% vs. 16%, p = 0.01) and osteopenia (52% vs. 39%, p = 0.007) at the lumbar spine and femoral neck (osteoporosis, 23% vs. 10%, p = 0.001; osteopenia, 58% vs. 29%, p = 0.001) were present in greater proportion in SS patients than matched controls. Bone microarchitecture analysis revealed significantly lower cortical volumetric BMD (vBMD) (p = 0.02) at the tibia, with relative preservation of the other parameters.
Conclusion
Low areal BMD (aBMD) is highly prevalent in SS as compared to age- and BMI-matched controls. However, there were no significant differences in bone microarchitectural measurements, except for tibial cortical vBMD, which was lower in adequately treated SS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sheehan’s syndrome (SS) is an uncommon cause of hypopituitarism affecting young females [1]. There is often a significant delay in diagnosis of SS resulting in a period of untreated pituitary insufficiency, even in contemporary cohorts [2, 3]. The cumulative untreated multiple pituitary hormone deficiencies are usually associated with multiple comorbidities and premature mortality. However, there is a residual burden of comorbidities even in treated patients with SS, including metabolic syndrome, clustering of cardiometabolic risk factors, cardiac dysfunction and atherosclerosis, non-alcoholic fatty liver disease, and osteoporosis [3,4,5,6].
Skeletal fragility in patients with SS is attributed to multiple reasons such as hypogonadism, hypothyroidism, growth hormone (GH) deficiency, nutritional factors, and alterations in calcium metabolism [6,7,8]. Though hypocortisolism may not adversely affect bone (or skeleton), glucocorticoid replacement therapy may predispose to osteoporosis in individuals with hypopituitarism [9, 10]. Hyperprolactinemia is associated with osteoporosis, but a majority (up to 80%) of SS patients have prolactin deficiency, which does not affect bone health [3]. Hypogonadism may also have a significant impact on bone health in patients with SS. However, postmenopausal osteoporosis is characterized by accelerated bone loss during the menopausal transition, at a stage coinciding with the rise in FSH (with only a subtle fall in estrogen) [11, 12]. SS patients have secondary hypogonadism, with low FSH and concurrent other hormone deficiencies, which may have different implications for bone health in terms of prevalence and severity.
The cortical and trabecular compartments of the skeleton are differentially affected by various hormones, with GH, thyroxine, and PTH predominantly affecting cortical bone and glucocorticoids and sex steroids affecting the trabecular compartment [13]. There is some evidence of alteration in bone turnover in patients with SS adequately replaced for hormone deficiencies, but microarchitectural composition including compartment-specific volumetric BMD and geometry has not been studied. Patients with SS have varied hormone deficiencies, which may differentially affect bone quality in addition to bone density and turnover.
The current study aimed to evaluate various aspects of skeletal integrity, including BMD, bone turnover, and microarchitecture in patients with SS.
Patients and methods
Study design and setting
The cohort comprised patients diagnosed with SS at the Post Graduate Institute of Medical Education and Research (PGIMER), a tertiary care center in India. Patients, either previously diagnosed with SS and already on stable doses of levothyroxine and glucocorticoid replacement or newly diagnosed with SS, were recruited into the study. SS was diagnosed based on a history of post-partum hemorrhage (with or without hypotension), lactation failure, and inability to resume spontaneous menses after delivery, with biochemical evidence of at least one pituitary hormone deficiency and partial or complete empty sella on imaging [3]. All patients were recruited for analysis of demographic, clinical, biochemical, and hormonal profiles. Bone microarchitecture assessment for more detailed compartment-specific bone quality was performed by a second-generation high-resolution peripheral quantitative computed tomography (HRpQCT) (n = 35). Patients with the use of bone-active agents in the recent or remote past were excluded from the study. Age- and BMI-matched controls were enrolled from the outpatient department (n = 35). The study was approved by the Institutional Ethics Committee of PGIMER (IEC-10/2021–2022). Written informed consent was obtained from all patients.
Clinical and hormonal evaluation
Biochemical investigations included serum calcium, albumin, inorganic phosphate, alkaline phosphatase, and creatinine. Hormonal evaluation including 25(OH)D, PTH, 0800 h cortisol, ACTH, DHEAS, T4, TSH, prolactin, LH, FSH, estradiol, and IGF-1 was performed using an electrochemiluminescence assay (ECLIA) (eCOBAS 8000, Roche, Hitachi).
Glucocorticoid and levothyroxine replacement doses were noted for each patient, and cumulative exposure to both was calculated as follows: cumulative exposure = (dose of hydrocortisone or levothyroxine × duration of exposure). For patients on prednisolone, the daily dose was converted to hydrocortisone equivalents. Cyclical gonadal hormone replacement therapy (HRT) was prescribed as per standard-of-care in all young females under the age of 45 years and continued till the age of 45 unless otherwise contraindicated. Briefly, it includes a fixed-dose combined pill of ethinyl estradiol (0.02 mg) and desogestrel (0.15 mg) administered once daily orally for 21 days every month.
Assessment of bone mineral density and bone turnover
Areal BMD was assessed using the DXA (HOLOGIC Discovery A, QDR 4500; Hologic, Inc., Bedford, MA) scanner for assessment of site-specific BMD measurements. Low bone mass was defined as Z-score < − 2 at any of the sites (lumbar spine and femoral neck) and normal if the score was > − 2. BMD T-scores were used to evaluate the status as follows: T > − 1, normal; T − 1 to − 2.5, osteopenia; and T < − 2.5, osteoporosis. Trabecular bone score (TBS) was evaluated using DXA and classified as normal (TBS ≥ 1.35) or low (< 1.35). Low TBS included both partially degraded (1.20 < TBS < 1.35) and degraded (TBS ≤ 1.20) microarchitecture. Bone turnover was assessed by bone formation (P1NP) and bone resorption (CTX) markers, both of which were estimated by ECLIA.
Bone microarchitecture assessment
High-resolution peripheral quantitative computed tomography (HRpQCT) was used to evaluate the three-dimensional skeletal microarchitecture in the cortical and trabecular bone compartments. Bone geometry, three-dimensional microarchitecture, as well as vBMD of the cortical and trabecular compartments were evaluated separately by second-generation HRpQCT (XtremeCT II, Scanco Medical AG, Switzerland). This second-generation scanner is equipped with a resolution of 61 µm and a voxel size of 17–273 µm. Prior to each scan, the patient was properly positioned in the scanner, and the appropriate scan region was identified and immobilized in a manufacturer-provided fiberglass cast. The default scan settings include the non-dominant radius and the dominant tibia. An initial two-dimensional scout view was obtained at a fixed distance (9 mm from the reference line at the endplate of the radius and 22 mm from the reference line at the tibial plafond), with the scan region width of approximately 10.2 mm [14, 15]. Motion artifacts were reduced by grading the individual images and including only scan images with grades 3 or less [16]. Those with image grades 4 or higher were subjected to repeat analysis, as per standard protocol. Cortical microarchitecture assessment included cortical porosity, pore diameter, thickness, area, and vBMD. Trabecular microarchitectural parameters included trabecular number, thickness, separation, area, trabecular bone volume fraction, and vBMD. All parameters were analyzed at both the radius and tibia. The parameters were directly measured rather than “derived,” as the second-generation scanner was used [15]. These measurements are considered to be surrogate markers of bone quality and have been validated to predict fracture risk [17].
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) 22.0 software program (IBM Statistics 22.0). Normality was assessed for quantitative parameters using the Kolmogorov–Smirnov method, and they were classified as parametric or non-parametric. Categorical variables were compared between the groups using Pearson’s chi-square or Fisher’s exact test. Mann–Whitney U-test was used to compare the median values for non-parametric data, and the student’s t-test was used to compare the means of two groups for parametric data. P-values less than 0.05 were considered significant. Data are presented as n (%), median (quartile q25–q75), or mean ± standard deviation (SD).
Results
Of the 40 patients with SS in our cohort, 5 patients who received bone-active agents (bisphosphonates or teriparatide) were excluded, and the remaining 35 patients were recruited in the study cohort. The mean age of the patients at enrolment was 45.5 ± 9.3 years with a lag of 8.3 ± 7.2 years prior to diagnosis (from last childbirth) (Table 1). Multiple hormone deficiencies were present in all patients, with 86% having insufficiency of three or more hormone axes. Regular glucocorticoid and levothyroxine replacement was ongoing in 94% of the cohort. The mean daily glucocorticoid dose (in hydrocortisone equivalents) was 12.2 ± 5.8 mg, and 12% of the cohort was on prednisolone (single daily dose). Estrogen–progestin replacement was given in 58% of patients, with a mean duration of 6.3 ± 3.2 years of usage and 9.3 ± 6.0 years since stopping medication. GH deficiency was present in 93% of the patients, but none of the patients had received GH replacement at the time of enrolment. None of the patients in either group had chronic kidney disease, history of malabsorption, rheumatoid arthritis, smoking, alcohol intake or were on anti-epileptics, warfarin, or therapeutic glucocorticoids. The mean duration of follow-up was 9.7 ± 7.1 years.
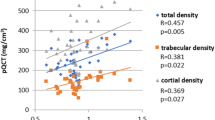
Serum 25(OH)D and PTH levels were comparable between the groups (Table 1). Bone turnover markers (P1NP and CTX) were not significantly different between patients and controls (p > 0.05) (Table 1). T-scores [− 1.6 (− 2.3 to − 1.3) vs − 0.7 (− 1.5 to − 0.2)] (p = 0.002) and Z-scores [− 1.2 (− 1.6 to − 0.3) vs − 0.4 (− 1.0 to 0.3)] (p = 0.01) were significantly lower at the femoral neck (FN) in SS as compared to controls. T-scores [− 1.9 (− 2.3 to − 0.9) vs − 1.2 (− 2.3 to − 0.3)] and Z-scores [− 1.2 (− 1.8 to − 0.9) vs − 0.8 (− 2.0 to − 0.2)] at the lumbar spine (LS) were also lower in patients as compared to controls, but it was non-significant (Table 2). Osteopenia was present in 52% of patients at the LS, 58% at the FN, and 32% at the distal 1/3rd of radius (DER) in SS and in 39% of the controls at the LS, 29% at the FN, and 22% at the DER. Osteoporosis was present in 26% of patients at the LS, 23% at the FN, and 22% at the DER and in 16% of the controls at the LS, 10% at the FN, and 4% at the DER. Low aBMD (osteopenia or osteoporosis) was prevalent in a significantly greater proportion of SS as compared to controls at LS (78% vs 55%), FN (81% vs 39%), and DER (54% vs 26%) (Fig. 1). Similar results were obtained on excluding peri- and postmenopausal controls with respect to low aBMD.
The bone microarchitectural assessment showed no significant differences between SS patients and controls either in terms of the mean TBS scores or the proportion of patients with impaired bone microarchitecture (low TBS score). On HRpQCT analysis, there were no differences between the groups in terms of bone geometry parameters (Table 3). Cortical vBMD was significantly lower in SS patients at the tibia as opposed to controls (925.0 ± 93.2 vs 979.6 ± 59.3 mg HA/ccm, p = 0.002). None of the other vBMD parameters showed any significant differences between the groups. Bone structural parameters were also comparable between both groups, except for a higher trabecular number at the tibia in patients with SS (Table 3). On comparing SS patients with premenopausal controls, there were no significant differences in bone microarchitectural parameters. Representative images of age-matched SS patients and controls are shown in Fig. 2.
HRpQCT images (a–d). The radius and tibia of a patient with Sheehan’s syndrome (a and c) and the radius and tibia of a control (b and d). Similar cortical vBMDs at radius in the patient with Sheehan’s syndrome (a) and the control (b); the significantly lower cortical volumetric BMD at tibia in the Sheehan’s syndrome patient (c) as compared to the preserved cortical volumetric BMD in the control (d)
Evaluation of patients with prior exposure to estrogen–progestin versus no exposure to estrogen–progestin was performed. Those with prior exposure to estrogen–progestin were significantly younger at current evaluation (42.9 ± 8.2 vs 51.3 ± 8.1 years, p = 0.007) and had a shorter lag period prior to diagnosis (5.3 ± 4.1 vs 12.0 ± 8.3 years, p = 0.008). There were no significant differences between the two groups in terms of T- or Z-scores or the prevalence of osteopenia or osteoporosis, but radius trabecular parameters (trabecular volumetric BMD [134.4 ± 33.0 vs 112.5 ± 39.6 mg HA/ccm, p = 0.05], trabecular bone volume fraction [0.20 ± 0.05 vs 0.16 ± 0.05, p = 0.05], and trabecular separation [0.73 ± 0.12 vs 0.86 ± 0.20 mm, p = 0.05]) were better in the group who received estrogen–progestin as compared to the group which did not, with a trend toward significance. On comparing SS patients who received estrogen–progestin (n = 20) with premenopausal controls (n = 18), while there were no significant differences in aBMD, the trabecular number at the tibia was significantly higher in patients than controls (1.19 ± 0.19 vs 1.00 ± 0.23, p = 0.01).
The prevalence of low aBMD (osteopenia or osteoporosis) was significantly higher in SS patients as compared to controls at all three sites. There was no significant correlation between LS or FN aBMD and any of the other clinical parameters (including current age, age at onset of disease, lag period, duration of disease, and glucocorticoid or levothyroxine dose or duration) (Table 4). On analyzing the determinants of low aBMD at the LS, only the lag period showed a trend toward significance, with a longer lag period in those having low aBMD as compared to those with normal aBMD (10.2 ± 7.4 vs 4.8 ± 3.7, p = 0.09). Similarly, only a cumulative dose of levothyroxine was significantly associated with BMD at FN, with a higher median cumulative dose in those with low aBMD as compared to those with normal aBMD [219 (118–520) vs 27 (11–137) mg, p = 0.04] (Supplementary Table 1 and 2). None of the other clinical factors, including age, lag period before diagnosis, and glucocorticoid dose or duration, were significantly different between those with low aBMD and those with normal aBMD at LS or FN. Clinical fractures were present in 5 patients historically. There were no incident fractures.
Discussion
The current study provides novel insights into the skeletal integrity including microarchitectural parameters in women diagnosed and treated for Sheehan’s syndrome. Patients with SS had a significantly greater prevalence of low aBMD as compared to age- and BMI-matched controls at all three sites studied (lumbar spine, femoral neck, and distal third of radius). There were no significant differences in the bone microarchitecture, except for lower cortical vBMD at the tibia in these patients who were on adequate and appropriate hormone replacement for relevant hormone deficiencies except GH. To the best of our literature search, this is the first study to report vBMD, bone geometry, and structure in patients with SS.
Patients with SS have a deficiency of multiple pituitary hormones by the time they are diagnosed. Hormone replacement is required for the deficient hormonal axes and is usually lifelong, except estrogen–progestin replacement. In the current study, ongoing levothyroxine and glucocorticoid replacement was required in 94% of the cohort. Past or current estrogen–progestin replacement was done in 58% of patients. Though SS is a rare cause of GH deficiency overall, the prevalence of GH deficiency in SS is quite high per se [18], as was found in the current study. There was no significant difference between patients and controls with respect to circulating levels of calcium and 25(OH)D, or bone turnover as assessed by serum P1NP and CTX. Bone turnover markers (P1NP and CTX) have not been extensively evaluated in SS, but evidence from patients with hypopituitarism suggests low bone turnover status at baseline, which increases following hormone replacement [19, 20]. This was the probable reason why P1NP and CTX were not significantly different in SS patients as opposed to controls, due to optimal hormone replacement.
We found a greater prevalence of low aBMD at all three sites when T-scores were considered but a comparable prevalence at all sites except DER when using Z-scores. With the T-score-based BMD interpretation, the prevalence of low aBMD (osteopenia or osteoporosis) was higher in our cohort compared with a previous study [6]. However, a lower prevalence of osteopenia and osteoporosis was found while comparing our results with a Z-score-based interpretation of a previous study. Possible reasons for finding a lower prevalence of low bone mass in the present study could be earlier diagnosis and timely intervention with appropriate hormone replacement especially correction of gonadal hormone deficiency, but this would need further elucidation. The prevalence of osteopenia and osteoporosis has been variably studied in very few prior studies in terms of T- and Z-scores, all being cross-sectional in nature [6,7,8]. In a small interventional analysis, low BMD at baseline significantly improved following estrogen replacement, coupled with calcium and vitamin D supplementation nutritional optimization, despite all patients being GH deficient [7]. This also suggests the predominant role of gonadal hormone deficiency in causing osteoporosis.
On further examining the determinants of low aBMD at the LS, we found a longer lag period in those with low aBMD as opposed to those with normal BMD, but this only showed a trend toward significance. This could be because of the longer duration of untreated gonadal hormone deficiency. But those who had received gonadal hormone replacement had better trabecular vBMD, greater trabecular bone volume fraction, and lesser trabecular separation at the radius, all with a trend toward significance, without any differences in terms of areal BMD or TBS. They also had a shorter diagnostic delay, which also suggests the potential benefit of early diagnosis and timely intervention with the replacement of deficient hormones, which has a favorable impact on bone health on long-term follow-up. However, this needs to be ratified in larger studies in the future.
Apart from hormone deficiencies, hormone replacement with glucocorticoids can also adversely affect bone health status in SS even with smaller doses normally required as replacement doses for secondary hypocortisolism [21, 22]. There was no appreciable evidence reminiscent of glucocorticoid-induced osteoporosis in these patients due to much lower doses of glucocorticoids than normally used for therapy. GH normally inhibits the generation of active from inactive cortisol by inhibiting 11beta-hydroxysteroid dehydrogenase 1 (11-βHSD1). GH deficiency (seen in majority of patients with SS) upregulates 11-βHSD1, resulting in increased conversion of inactive to active cortisol [23]. This may be responsible for exaggerated adverse skeletal effects even at low doses of glucocorticoids in patients with SS. The mean daily glucocorticoid dose in the current study was lower overall (12.2 ± 5.8 mg in terms of hydrocortisone equivalents) as compared to a previous study in hypopituitary patients on glucocorticoid replacement (20·5 ± 5·8 mg/day) [21]. However, the mean daily dose of hydrocortisone replacement was comparable between those who had low aBMD versus those who did not. This suggests that rather than the daily replacement dose, it is the chronicity of exposure or cumulative dose that probably bears more relevance for adversely impacting bone in patients with SS [22]. It is also known that there are differential effects of prednisolone and hydrocortisone on the skeleton, with more detrimental effects of prednisolone as compared to hydrocortisone, both in terms of BMD and fracture risk [24, 25]. However, as most of our patients were receiving hydrocortisone (n = 29) and only 3 were on prednisolone, we could not assess the differential effect of hydrocortisone versus prednisolone on BMD because of the small size.
Levothyroxine replacement was significantly associated with low aBMD at FN. This is previously described in the context of FN BMD and is probably due to a higher proportion of cortical bone at this site [26]. For patients with Sheehan’s syndrome or any other cause of secondary hypothyroidism, T4 (total or free) is used to monitor thyroid hormone replacement rather than TSH. However, in this scenario, the use of T4 could sometimes result in overtreatment with levothyroxine and, consequently, adverse effects on bone metabolism as there is a direct correlation between T4 and BMD with or without osteoporosis [27].
The current study investigated bone microarchitecture in patients with SS. We found lower cortical vBMD at the tibia, with relatively preserved trabecular parameters in SS as opposed to age- and BMI-matched controls. Volumetric BMD, apart from bone microstructure, is reported to be an independent predictor for clinical and major osteoporotic fractures in other settings [28]. In general, cortical vBMD is greater in females than in males [29]. However, the current study revealed deficits in cortical vBMD in women with SS. This was probably due to the residual GH deficiency (a major impediment for GH replacement is its high cost in resource-poor environments such as India) despite appropriate and adequate replacement for all other hormone deficiencies including gonadal replacement. GH exerts its predominant influence on the cortical compartment of the skeleton, as evidenced by rodent models of mutated GH-releasing hormone or GH receptor manifesting low BMD and reduced cortical bone, with preserved trabecular bone [30, 31]. Cortical bone fragility is characteristically seen in adults with GH deficiency, and GH therapy leads to increased cortical thickness mediated via endosteal bone growth [32]. Our observation of no significant differences in trabecular microarchitectural parameters is concordant with prior studies that have reported similar findings albeit in other settings [33, 34] and also corroborates with the greater influence of GH on cortical bone. However, the exact reason for these findings occurring at the tibia and not at the radius is not known and needs to be explored in future studies.
It can thus be summarized that patients with SS have a high prevalence of low BMD, and the predominant contributor to low BMD is a low cortical BMD, substantiated by findings from the current study. This is because the cortical bone contributes to nearly 80% of the entire skeleton [35]. The cortical bone also provides strength and protection to the skeleton, so it is probably more important than the trabecular (cancellous) bone from the clinical point of view. The trabecular bone provides stability and transfers the load to the cortical bone. Furthermore, cortical vBMD is a key parameter associated with major osteoporotic fractures, with better predictive performance than even incident fractures [36].
The strengths of the study are the evaluation of multiple skeletal health-related parameters including bone microarchitectural assessment using HRpQCT in the largest single-center cohort of patients with SS. We acknowledge certain limitations, such as a small patient number for microarchitectural assessment, cross-sectional nature, lack of complete data on fractures and BMD, mechanical strength, bone histomorphometry, and calcium and vitamin D intake. Larger multicentric studies with histomorphometry may improve further understanding of bone fragility in SS.
Conclusion
SS is a model for hypopituitarism with a high prevalence of low aBMD, which should be evaluated in all patients with SS. Tibial cortical vBMD is significantly lower with relative preservation of trabecular vBMD in treated SS patients. Baseline and prospective surveillance for BMD in patients with SS may lead to improved overall outcomes in these patients.
Data Availability
The data that support the findings of this study are available on reasonable request from the corresponding author.
References
Das L, Dutta P (2023) Approach to the patient: a case with an unusual cause of hypopituitarism. J Clin Endocrinol Metab 108(6):1488–1504
Ramiandrasoa C, Castinetti F, Raingeard I, Fenichel P, Chabre O, Brue T, Courbiere B (2013) Delayed diagnosis of Sheehan’s syndrome in a developed country: a retrospective cohort study. Eur J Endocrinol 169(4):431–438
Das L, Sahoo J, Dahiya N, Taneja S, Bhadada SK, Bhat MH, Singh P, Suri V, Laway BA, Dutta P (2022) Long-term hepatic and cardiac health in patients diagnosed with Sheehan’s syndrome. Pituitary 25(6):971–981
Laway BA, Rasool A, Baba MS, Misgar RA, Bashir MI, Wani AI, Choh N, Shah O, Lone A, Shah Z (2023) High prevalence of coronary artery calcification and increased risk for coronary artery disease in patients with Sheehan syndrome-a case-control study. Clin Endocrinol (Oxf) 98(3):375–382. https://doi.org/10.1111/cen.14871
Laway BA, Ramzan M, Allai MS, Wani AI, Misgar RA (2016) Cardiac structural and functional abnormalities in females with untreated hypopituitarism due to Sheehan syndrome: response to hormone replacement therapy. Endocr Pract 22(9):1096–1103
Chihaoui M, Yazidi M, Chaker F, Belouidhnine M, Kanoun F, Lamine F, Ftouhi B, Sahli H, Slimane H (2016) Bone mineral density in Sheehan’s syndrome; prevalence of low bone mass and associated factors. J Clin Densitom 19(4):413–418
Agarwal P, Gomez R, Bhatia E, Yadav S (2019) Decreased bone mineral density in women with Sheehan’s syndrome and improvement following oestrogen replacement and nutritional supplementation. J Bone Miner Metab 25(37):171–178
Gokalp D, Tuzcu A, Bahceci M, Arikan S, Ozmen CA, Cil T (2009) Sheehan’s syndrome and its impact on bone mineral density. Gynecol Endocrinol 25(5):344–349
Ragnar Agnarsson H, Johannsson G, Ragnarsson O (2014) The impact of glucocorticoid replacement on bone mineral density in patients with hypopituitarism before and after 2 years of growth hormone replacement therapy. J Clin Endocrinol Metab 99(4):1479–1485
Ragnarsson O, Nyström HF, Johannsson G (2012) Glucocorticoid replacement therapy is independently associated with reduced bone mineral density in women with hypopituitarism. Clin Endocrinol 76(2):246–252
Zaidi M, Yuen T, Kim SM (2023) Pituitary crosstalk with bone, adipose tissue and brain. Nat Rev Endocrinol 15:1–4
Wang J, Zhang W, Yu C, Zhang X, Zhang H, Guan Q, Zhao J, Xu J (2015) Follicle-stimulating hormone increases the risk of postmenopausal osteoporosis by stimulating osteoclast differentiation. PLoS One 10(8):e0134986
Seeman EH, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL (1982) Differential effects of endocrine dysfunction on the axial and the appendicular skeleton. J Clin Investig 69(6):1302–1309
Whittier DE, Boyd SK, Burghardt AJ, Paccou J, Ghasem-Zadeh A, Chapurlat R, Engelke K, Bouxsein ML (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31:1607–1627
Agarwal S, Rosete F, Zhang C, McMahon DJ, Guo XE, Shane E, Nishiyama KK (2016) In vivo assessment of bone structure and estimated bone strength by first-and second-generation HR-pQCT. Osteoporos Int 27:2955–2966
Sode M, Burghardt AJ, Pialat JB, Link TM, Majumdar S (2011) Quantitative characterization of subject motion in HR-pQCT images of the distal radius and tibia. Bone 48(6):1291–1297
Mikolajewicz N, Bishop N, Burghardt AJ, Folkestad L, Hall A, Kozloff KM, Lukey PT, Molloy-Bland M, Morin SN, Offiah AC, Shapiro J (2020) HR-pQCT measures of bone microarchitecture predict fracture: systematic review and meta-analysis. J Bone Miner Res 35(3):446–459
Das L, Dutta P (2023) Unusual and lesser-known rare causes of adult growth hormone deficiency. Best Pract Res Clin Endocrinol Metab 28:101820
Kandemir N, Gone EN, Yord N (2002) Responses of bone turnover markers and bone mineral density to growth hormone therapy in children with isolated growth hormone deficiency and multiple pituitary hormone deficiencies. J Pediatr Endocrinol Metab 15(6):809–816
Behan LA, Kelleher G, Hannon MJ, Brady JJ, Rogers B, Tormey W, Smith D, Thompson CJ, McKenna MJ, Agha A (2014) Low-dose hydrocortisone replacement therapy is associated with improved bone remodelling balance in hypopituitary male patients. Eur J Endocrinol 170(1):141–150
Ragnarsson O, Nyström HF, Johannsson G (2012) Glucocorticoid replacement therapy is independently associated with reduced bone mineral density in women with hypopituitarism. Clin Endocrinol 76(2):246–252
Hardy RS, Zhou H, Seibel MJ, Cooper MS (2018) Glucocorticoids and bone: consequences of endogenous and exogenous excess and replacement therapy. Endocr Rev 39(5):519–548
Toogood AA, Taylor NF, Shalet SM, Monson JP (2000) Modulation of cortisol metabolism by low-dose growth hormone replacement in elderly hypopituitary patients. J Clin Endocrinol Metab 85(4):1727–1730. https://doi.org/10.1210/jcem.85.4.6505
Frey KR, Kienitz T, Schulz J, Ventz M, Zopf K, Quinkler M (2018) Prednisolone is associated with a worse bone mineral density in primary adrenal insufficiency. Endocr Connect 7(6):811–818
Vestergaard P, Rejnmark L, Mosekilde L (2008) Fracture risk associated with different types of oral corticosteroids and effect of termination of corticosteroids on the risk of fractures. Calcif Tissue Int 82:249–257
Garton M, Reid I, Loveridge N, Robins S, Murchison L, Beckett G, Reid D (1994) Bone mineral density and metabolism in premenopausal women taking l-thyroxine replacement therapy. Clin Endocrinol 41(6):747–755
Sheng N, Xing F, Wang J, Duan X, Xiang Z (2023) T4 rather than TSH correlates with BMD among euthyroid adults. Front Endocrinol 9(13):1039079
de Bakker CM, Tseng WJ, Li Y, Zhao H, Liu XS (2017) Clinical evaluation of bone strength and fracture risk. Curr Osteoporos Rep 15:32–42
Riggs BL, Melton LJ III, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19(12):1945–1954
Mazziotti G, Frara S, Giustina A (2018) Pituitary diseases and bone. Endocr Rev 39(4):440–488
Giustina A, Mazziotti G, Canalis E (2008) Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev 29(5):535–559
Hyldstrup L, Conway GS, Racz K, Keller A, Chanson P, Zacharin M, Lysgaard AL, Andreasen AH, Kappelgaard AM (2012) Growth hormone effects on cortical bone dimensions in young adults with childhood-onset growth hormone deficiency. Osteoporos Int 23:2219–2226
Tanriverdi F, Unluhizarci KÜ, Kula MU, Guven M, Bayram FA, Kelestimur F (2005) Effects of 18-month of growth hormone (GH) replacement therapy in patients with Sheehan’s syndrome. Growth Hormon IGF Res 15(3):231–237
Balducci R, Toscano V, Pasquino AM, Mangiantini A, Municchi G, Armenise P, Terracina S, Prossomariti G, Boscherini B (1995) Bone turnover and bone mineral density in young adult patients with panhypopituitarism before and after long-term growth hormone therapy. Eur J Endocrinol 132(1):42–46
Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol 3(Supplement 3):S131–S139
Cheung WH, Hung VW, Cheuk KY, Chau WW, Tsoi KK, Wong RM, Chow SK, Lam TP, Yung PS, Law SW, Qin L (2021) Best Performance parameters of HR-pQCT to predict fragility fracture: systematic review and meta-analysis. J Bone Miner Res 36(12):2381–2398
Acknowledgements
We wish to acknowledge Mr. Nipun Chawla and Mr. Raman Saini for helping in the HRpQCT data acquisition.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Das, L., Laway, B.A., Sahoo, J. et al. Bone mineral density, turnover, and microarchitecture assessed by second-generation high-resolution peripheral quantitative computed tomography in patients with Sheehan’s syndrome. Osteoporos Int 35, 919–927 (2024). https://doi.org/10.1007/s00198-024-07062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07062-z