Abstract
Sleep abnormalities, such as insomnia, nightmares, hyper-arousal, and difficulty initiating or maintaining sleep, are diagnostic criteria of posttraumatic stress disorder (PTSD). The vivid dream state, rapid eye movement (REM) sleep, has been implicated in processing emotional memories. We have hypothesized that REM sleep is maladaptive in those suffering from PTSD. However, the precise neurobiological mechanisms regulating sleep disturbances following trauma exposure are poorly understood. Using single prolonged stress (SPS), a well-validated rodent model of PTSD, we measured sleep alterations in response to stressor exposure and over a subsequent 7-day isolation period during which the PTSD-like phenotype develops. SPS resulted in acute increases in REM sleep and transition to REM sleep, and decreased waking in addition to alterations in sleep architecture. The severity of the PTSD-like phenotype was later assessed by measuring freezing levels on a fear-associated memory test. Interestingly, the change in REM sleep following SPS was significantly correlated with freezing behavior during extinction recall assessed more than a week later. Reductions in theta (4–10 Hz) and sigma (10–15 Hz) band power during transition to REM sleep also correlated with impaired fear-associated memory processing. These data reveal that changes in REM sleep, transition to REM sleep, waking, and theta and sigma power may serve as sleep biomarkers to identify individuals with increased susceptibility to PTSD following trauma exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep impairments are a diagnostic criteria of posttraumatic stress disorder (PTSD) (American Psychiatric Association 2013), and self-reported poor sleep after trauma exposure has been identified as a predictor of subsequent disorder severity (Mellman et al. 1995, 2002; Brown et al. 2011). However, the precise electrophysiological properties of sleep that accompany trauma exposure remain poorly understood. Disturbances in REM sleep have been hypothesized to be a hallmark feature of PTSD (Ross et al. 1989; Germain 2013; Vanderheyden et al. 2014) due to the critical role of REM sleep in emotional regulation and memory consolidation (Walker 2009; Walker and van der Helm 2009; Wellman et al. 2013), both of which are impaired in PTSD. However, many trauma-exposed individuals never develop PTSD, and it is unknown whether sleep plays a role in mediating resilience or susceptibility to this disorder.
In addition to sleep disturbances, recent evidence suggests that frequency-specific EEG activity may also function as a biomarker of resilience and susceptibility to posttraumatic stress disorder (Cowdin et al. 2014). Specifically, theta band (4–10 Hz) activity during REM sleep is higher in humans who are resilient to PTSD acquisition following trauma exposure compared with those that develop PTSD. Theta band (Merica and Blois 1997; Mitchell et al. 2008) and sigma band (10–15 Hz) activity (Tamminen et al. 2010; Watts et al. 2012) play a critical role in sleep-dependent memory consolidation processes, making these EEG frequencies important candidate biomarkers of PTSD severity, though their link with PTSD development has only been posited thus far (Vanderheyden et al. 2014).
To date, most human studies of PTSD use a cross-sectional design since the unpredictable occurrence of trauma limits the ability to measure baseline sleep prior to trauma in the same subjects. In fact, studies that assess sleep in humans with PTSD often occur months to years after the original traumatic event. This temporal limitation prevents the capture of (1) sleep responses immediately following stress exposure and (2) the development of various sleep characteristics over time. Time likely plays a critical role in PTSD phenotype development as the disorder often does not manifest immediately following traumatic stress but develops in the days and months afterward (Knox et al. 2012; Ross 2014). Animal models, such as the one employed here, allow us to (1) assess baseline sleep (occurring prior to SPS), (2) assess sleep immediately following a stressful event (since the timing of the stressor is controlled), (3) assess sleep over the acquisition period of the PTSD-like phenotype development, and (4) use subjects as their own controls in longitudinal design and to compare changes in sleep characteristics along a spectrum of PTSD-like phenotypes. We concentrated on sleep changes from baseline (day 1) and between groups on the first (day 2) and last (day 9) days of exposure to SPS to assess changes in sleep as the PTSD-like phenotype developed.
The goal of our study was to assess changes in sleep time, sleep architecture, and EEG spectral power following SPS exposure and to correlate such changes with PTSD-like phenotype severity. First we assessed baseline sleep, then we performed SPS to induce a long-term PTSD-like phenotype (Liberzon et al. 1997, 1999; Yamamoto et al. 2009). Fear extinction testing was used to assess the severity of the PTSD-like phenotype. We hypothesized that sleep characteristics may serve as biomarkers of disorder susceptibility and that we may identify critical windows of time for the development of PTSD following stress exposure.
Methods and materials
General animal procedures
All animal procedures were carried out in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and with approval from the University of Michigan Committee on the Use and Care of Laboratory Animals. All animals were allowed ad libitum access to rat chow and housed individually in sound-attenuating boxes on a 12:12-light/dark schedule at constant temperature (23 °C) and humidity (20 %).
Electrophysiology
Surgical implantation of electrodes for sleep/waking analysis
Twenty-eight male Long Evans rats (250–300 g, 8–10 weeks old, Charles River) were anesthetized with ketamine (50 mg/kg)/xylazine (5 mg/kg) and placed into a stereotaxic frame. An incision was made on the top of the skull, and the skin was retracted. After cleaning the surface of the skull with 3 % hydrogen peroxide, four holes were drilled through the cranium, and screw electrodes (Plastics One, Roanoke, VA) were inserted. Two electrodes were implanted bilaterally over the dorsal hippocampus (2.5 mm lateral to midline, 3.5 mm posterior to bregma), and two electrodes were implanted bilaterally over the frontal cortical area (2.5 mm lateral to midline, 1.5 mm anterior to bregma) for electroencephalographic (EEG) recordings. Two flexible wire electrodes were threaded through the dorsal neck muscles for electromyographic (EMG) recordings. Gold pins were connected to the ends of each electrode and then placed into a six pin connector (Plastics One, Roanoke, VA) which was attached to the skull via dental acrylic. Animals were injected with subcutaneous Rimadyl (0.03 mL) to reduce inflammation and ciprofloxacin (1 mL) to counteract infection following surgery. All animals were given at least 10 days to recover from surgery prior to beginning the experiment. Animal well-being was assessed daily during the surgical recovery period. No sign of illness or pain, including decreased motility and responsiveness, vocalizations, lack of appetite, or decreased grooming, was found in any of the animals in this study.
EEG/EMG recording and analysis
Following recovery from surgery, animals were housed individually and connected to the recording system via a lightweight, flexible tether that was attached to a commutator, allowing relatively free movement within their home cage. The tether was connected to a Neuralynx EEG Reference Panel (Bozeman, MT) that was connected to an amplifier that fed the signals into a computer for data acquisition. The recording system (called AD, made by MA Wilson and L Frank, M.I.T., Cambridge, MA) sampled amplified signals at 1000 Hz and then filtered them between 0.1 and 100 Hz using a second-order Butterworth filter. Prior to analysis, signals were down-sampled to 250 Hz by taking every fourth data point. Hippocampal and frontal leads were referenced to their respective leads in the opposite hemisphere to obtain two channels of EEG, while the two EMGs were referenced together for one channel of EMG recording. Animals were given 2 days to acclimate to the tethers prior to baseline recordings. Each day, at the beginning of the sleep phase (lights on), animals were briefly assessed for food and water availability and general health. Animals were left undisturbed for the remainder of the day. Animals were continuously tethered and recorded across the 9-day recording period except when the SPS treatment group was removed for stressor exposure for 3 h on day 2.
Every 24 h, the data were transferred from the recording computer, stored on an external hard drive, and manually scored for sleep/waking state off-line by a human scorer, blind to the experimental group assignment of the animal, using custom MATLAB (Mathworks, Natick, MA) programs. EEG and EMG files were loaded into a Sleepscorer program (Gross et al. 2009) in which sleep states were manually assigned in 10-s epochs for each 24-h file. One of five sleep/waking states were assigned to each epoch. Active waking consists of visible theta activity and high EMG activity. Quiet waking consists of low amplitude, desynchronized EEG, and relatively little EMG activity. Non-rapid eye movement sleep (NREM sleep) consists of high amplitude, 0–3 Hz synchronized EEG, and low EMG activity. Transition to REM sleep consists of high amplitude, 10–15 Hz spindle activity, and low EMG activity. REM sleep consists of clear, sustained theta (4–10 Hz) activity, and phasic muscle twitches on a background of minimal EMG. When appropriate, time spent in active and quiet waking was combined into one waking state. The percent of each day spent in specific sleep/waking states was continually assessed over 9 days, including the baseline (day 1), the SPS exposure day (day 2), and the 7 days of isolation (days 3–9) (Fig. 1).
Experimental design. Following 10 days of recovery from surgery, all animals (N = 28) were recorded for one 24-h baseline day (day 1). The following day, at ZT 0 (lights on), animals were divided into two groups. SPS was performed on 17 animals, and the remainder served as controls (day 2). EEG/EMG recordings were made for the remainder of the SPS exposure day and the following 7 days (day 3–9). Fear conditioning experiments occurred at the conclusion of the EEG/EMG recording period
After 24 h of baseline recording (Baseline, day 1, Fig. 1), animals were unhooked from the recording system and single prolonged stress (SPS, described below) was performed. Following SPS exposure (SPS, Fig. 1), animals were reconnected to the recording system and eight subsequent days were recorded (SPS exposure day and seven isolation days, Fig. 1).
EEG power spectral analysis was performed using Fast Fourier transform (FFT) via MATLAB software. Average daily power spectrums are reported for each of the 9 days of the experiment. FFTs were performed on individual sleep-state data.
Single prolonged stress
Single prolonged stress was performed as previously described (Liberzon et al. 1997). The SPS rodent model of PTSD has shown good face and construct validity to the human disorder (Yamamoto et al. 2009; Pitman et al. 2012), making it a useful model to study the role of sleep in PTSD development. Eleven animals served as controls (non-SPS exposed), and 17 animals were exposed in batches of 6–8 to 3 successive stressors at the start of the circadian day (SPS exposure day, Fig. 1, at lights on, ZT 0). First, physical restraint was performed for 2 h in custom-built polymethyl methacrylate individual restraining devices. Next, the animals were placed in a (25 × 17 × 16 in.) plastic bin containing 21–24 °C water and were forced to swim together for 20 min. The batch swim technique increases the stressor challenge as animals attempt to exit the water by climbing over one another. A 15-min recuperation period, in a towel-lined bin, followed the forced swim. Lastly, in a lidded bell jar, the animals were placed on a Delrin® platform (DuPont, Parkersburg, WV), with eight 3-cm-diameter holes raised 10 cm above 75 ml ether (Sigma, Saint Louis) for group exposure to ether vapors until fully anesthetized (no more than 5 min). The animals were then returned to their home cage where they were singly housed and isolated while electrophysiological recordings were collected continuously for 8 days.
Control animals were handled in a similar fashion as the SPS-exposed animals except they did not receive the restraint, swim, and ether stressors. Control animals were singly housed for the 9-day recording period. EEG/EMG recordings in control animals were continuously assessed for sleep states and verified to not change over the course of the 9-day experiment (Fig. 2a–d).
SPS-induced sleep changes (assessed in 24-h epochs). EEG/EMG recordings occurred for 9 days, from baseline (day 1) to SPS exposure (day 2) and during the week of isolation (days 3–9). Comparisons were made between baseline day and all other experimental days. REM sleep, transition to REM sleep, and waking (a, c, d, respectively) were significantly altered on the SPS exposure day (measured as a percentage of the 24 h day) (* = p value < 0.05). Control animals were exposed to 9 days of EEG/EMG recording in the same manner as SPS-exposed animals. An additional two-way ANOVA comparing sleep between the control animals shown here and the SPS-exposed animals in the figure revealed a significant effect of SPS on REM sleep on the SPS exposure day [F(1, 170) = 3.03, p = 0.008] (# = p value < 0.05 for the comparison of control animals to SPS-treated animals). Control animals did not show significant alterations in sleep over the 9-day testing period (a–d)
Fear conditioning, fear extinction, and extinction recall
At the conclusion of the 9 days of EEG/EMG recording, fear conditioning experiments were conducted using 15 SPS-exposed and 11 control rats. Fear conditioning, extinction, and extinction recall were performed as previously published (experiment 3 from Knox et al. 2012). All fear conditioning, extinction, and extinction recall experiments were performed in four identical Coulbourn Instruments Rat Test Cages (12″W × 10″D × 12″H) (Whitehall, PA) containing a Shock Floor with 18 current-carrying metal bars, a wall-mounted speaker, and in-chamber lighting. Test cages were housed in wooden sound-attenuating boxes. Tones were delivered via speakers mounted in the housing of the test cages and controlled by FreezeFrame data acquisition software (Coulbourn Instruments). Shocks were delivered through precision animal shockers (Coulbourn Instruments) also controlled by FreezeFrame software. Ceiling-mounted cameras recorded behavior for analysis, and FreezeFrame was used to assess freezing levels.
As previously published (Knox et al. 2012), two unique contexts were created using two different sets of olfactory and visual cues. Context A consists of 50 ml of 1 % acetic acid solution placed in a small dish above the test cage and standard lighting which illuminates the chamber walls of the Rat Test Cages. Context B consists of 50 ml of a 1 % ammonium hydroxide solution placed in a small dish above the test cage along with patterned paper placed on the chamber walls to alter the visual context. Other laboratories, as well as our own, have used these specific methods repeatedly in the past and found no evidence of increased stress with these concentrations of acetic acid or ammonium hydroxide; i.e., they show no effects on behavior or HPA response (Knox et al. 2012). To fully replicate extinction recall deficits following SPS, we used identical manipulations to those used earlier.
Fear-conditioned animals were exposed to five, 1-mA, 1-s foot-shocks paired with the cessation of a 10-s 80-dB tone in Context A. The first tone was presented 180 s after the animal was placed in the test cage, and the subsequent tones occurred with a 60-s inter-tone interval. Sixty seconds after the last tone, animals were removed from their home cages. Fear extinction was conducted 24 h after fear conditioning and was performed in the distinctly different Context B. Fear extinction consisted of 180-s acclimation to the new context and presentation of 30 10-s tones without the paired foot-shock, with each tone followed by a 60-s inter-tone interval. Extinction recall was assessed 24 h after extinction and consisted of the animals being placed back into the same fear extinction context (Context B) for 180-s acclimation followed by 10 tones (60-s inter-tone interval), again without foot-shock. The percent time spent immobile (freezing) within each 70-s-long block (the 10-s tone and 60-s inter-tone interval combined) was assessed by setting threshold values of movement (number of pixels which moved between frames) via FreezeFrame software. Threshold values were verified to be similar to experimenter-confirmed immobility times.
Statistical analysis
Changes in sleep/wake parameters were assessed using a repeated-measures one-way analysis of variance (ANOVA) with assumed sphericity followed by Bonferroni-corrected post hoc tests via the GraphPad Prism software statistical package. Sleep states are reported as the percent of the day or percent of the sleep or active phase spent in each state. REM sleep, NREM sleep, transition to REM sleep, and waking states are reported as mean (M) percent of recording time.
The mean bout length and mean bout number per hour (sleep architecture) for each of the states was averaged over the sleep and active phases and was also analyzed using a repeated-measures one-way ANOVA followed by Bonferroni-corrected post hoc tests.
Statistical comparison of time spent freezing on the fear conditioning, extinction, and extinction recall tasks was made between SPS-exposed and control groups using an unpaired two-tailed Student’s t test. Average freezing levels between groups were analyzed independently on fear conditioning, extinction, and extinction recall days.
Pearson correlations of freezing behavior on extinction recall day compared to sleep changes from baseline to days 2–9 and to the changes in spectral power from baseline to day 9 were performed via GraphPad Prism software to quantify R 2 and p values with an N = 10 per control and SPS groups. Average 0.1–30 Hz power spectrum value changes over time were assessed by one-way ANOVA.
Results
Single prolonged stress increases REM sleep and transition to REM sleep and reduces wake time
Animals exposed to SPS showed significantly altered total percentage of the day (in 24-h epochs) spent in the states of REM sleep [F(8, 128) = 7.123, p < 0.0001], transition to REM sleep [F(8, 128) = 3.391, p = 0.0015], and waking [F(8, 128) = 4.392, p = 0.0001] (Fig. 2a, c, d) (* = p value < 0.05) compared with baseline. NREM sleep time [F(8, 128) = 1.075, p = 0.39] was not significantly altered by SPS exposure (Fig. 2b).
Post hoc analysis revealed that SPS exposure significantly altered REM sleep (M = 13.02 %), transition to REM sleep (M = 5.8 %), and waking (M = 56.34 %) time during SPS day compared to baseline (M = 10.07 %, M = 4.4 %, M = 60.41 %, respectively) (Fig. 2a, c, d) (* = p value < 0.05).
No significant changes in sleep/wake behavior were observed over the 9-day recording procedure in tethered control animals as assessed by one-way ANOVA: REM sleep [F(8, 26) = 1.04, p = 0.43], NREM sleep [F(8, 26) = 0.63, p = 0.74], transition to REM sleep [F(8, 26) = 0.34, p = 0.94], and waking [F(8, 128) = 0.54, p = 0.81] (Fig. 2a–d). Two-way ANOVA revealed a significant difference in REM sleep between control and SPS-exposed animals (# = p value < 0.05).
Active phase versus sleep phase: differences in sleep time during the incubation period of SPS
Animals exposed to SPS showed significantly altered sleep/waking states compared to baseline over the 9-day experiment differentially during the sleep phase (ZT 0–12 = white bars) and active phase (ZT 12–24 = black bars) (Fig. 3). Significant increases in REM sleep [F(8, 128) = 27.09, p < 0.0001] and transition to REM sleep [F(8, 128) = 4.721, p < 0.0001], and an acute reduction in waking [F(8, 128) = 19.18, p < 0.0001] (Fig. 3a, c, d) were found during the active phase on the SPS exposure day. NREM sleep was reduced [F(8, 128) = 8.127, p < 0.0001] during the active phase on days 5, 6, 7, and 8 compared to baseline (Fig. 3b).
Time-of-day specific acute and long-term changes in sleep following SPS. Sleep/waking states following SPS during the sleep phase (ZT 0–12, white bars) and active phase (ZT 12–24, black bars). SPS exposure resulted in significant, time-of-day dependent changes in sleep over the 9-day experimental period. SPS exposure resulted in acute, significant increases in REM sleep, transition to REM sleep, and an acute reduction in waking (a, c, d SPS day) relative to baseline, which were only significant during the active phase following trauma. NREM sleep was reduced during the active phase on days 5, 6, 7, and 8 compared to baseline (b). Significant long-term increases in REM sleep were found on day 7 during the sleep phase (a). Neither NREM sleep nor waking during the sleep phase was significantly altered (b, d). Transition to REM sleep varied significantly over time during the sleep phase, but no days differed from baseline (c). * = p value < 0.05, via Bonferroni-corrected post hoc comparisons
Significant increases in REM sleep time were found on day 7 during the sleep phase [F(8, 128) = 3.019, p = 0.56] (Fig. 3a). However, neither NREM sleep [F(8, 128) = 0.847, p = 0.56] nor waking [F(8, 128) = 0.85, p = 0.56] during the sleep phase was significantly altered following SPS exposure (Fig. 3b, d). Transition to REM sleep varied over time during the sleep phase [F(8, 128) = 2.78, p = 0.007], but unlike transition to REM sleep during the active phase, did not differ from baseline (Fig. 3c).
Active phase versus sleep phase: differences in sleep architecture
In addition to measuring how SPS changes the percent of time spent in each state, we also assessed changes in sleep architecture (bout length and bout number) during the sleep phase (ZT 0–12, lights on, white bars in Fig. 4) and active phase (ZT 12–24, lights off, black bars in Fig. 4) over all nine experimental days.
SPS-induced significant alterations in sleep architecture. Bout length and bout number are shown for each of the 5 sleep states recorded during the sleep (ZT 0–12, lights on, white bars in the figure) and active (ZT 12–24, lights off, black bars in the figure) phases over the 9-day experiment. SPS increased REM sleep bout length during the sleep phase on days 6–9 (a). REM sleep bout number acutely decreased during the sleep phase on the SPS exposure day, and bout number increased over baseline during the active phase (b); bout number returned to baseline on subsequent days. NREM sleep bout length was not significantly altered following SPS during the sleep or active phase (c). Sleep-phase and active-phase NREM sleep bout number was significantly altered by SPS exposure (d). Active-phase transition to REM sleep bout number increased the day following SPS exposure (f), and sleep-phase transition to REM sleep bout number was increased on the day after the SPS exposure (f). Active waking bout length increased during the active phase and became statistically significant by day 8 (g). Active waking bout length was acutely increased during the sleep phase following SPS exposure (g) whereas both active and quiet waking bout numbers were acutely reduced during the sleep phase following SPS exposure (h, j) (* = p value < 0.05, via Bonferroni-corrected post hoc comparisons)
SPS-exposed animals showed increased REM sleep bout length during the sleep phase on days 6–9 [F(8, 128) = 5.95, p < 0.0001] (Fig. 4a) relative to baseline. REM sleep bout number acutely decreased from baseline during the sleep phase on the SPS exposure day [F(8, 128) = 3.798, p = 0.0005], and bout number increased over baseline during the active phase [F(8, 128) = 15.59, p < 0.0001] (Fig. 4b). NREM sleep bout length was not altered following SPS during the sleep or active phase (Fig. 4c). Sleep-phase NREM sleep bout number was significantly decreased and then increased [F(8, 128) = 8.6, p < 0.0001] (Fig. 4d) relative to baseline, while active-phase NREM sleep bout number was acutely increased [F(8, 128) = 5.01, p < 0.0001] (Fig. 4d). Active-phase transition to REM sleep bout number increased over baseline on the day of SPS exposure [F(8, 128) = 3.52, p = 0.001] (Fig. 4f), and sleep-phase transition to REM sleep bout number was increased on the day after the SPS exposure (day 3) [F(8, 128) = 7.57, p < 0.0001] (Fig. 4f). Active waking bout length increased during the active phase and became significantly different from baseline by day 8 [F(8, 128) = 2.99, p = 0.0042] (Fig. 4g). Active waking bout length was acutely increased from baseline during the sleep phase [F(8, 128) = 11.88, p < 0.0001] following SPS exposure, whereas both active [F(8, 128) = 9.44, p < 0.0001] and quiet waking [F(8, 128) = 9.00, p < 0.0001] bout numbers were acutely reduced during the sleep phase following SPS exposure (Fig. 4h, j).
Single prolonged stress leads to fear extinction recall impairments
We used a fear conditioning paradigm to determine the severity of the SPS-induced PTSD-like phenotype. Fifteen previously SPS-exposed animals and 11 control (non-SPS exposed) animals underwent fear conditioning (described in the “Methods and materials”), followed 24 h later by extinction training and, 24 h after extinction, by fear extinction recall testing (see experimental protocol in Fig. 1) as previously described (Knox et al. 2012). Average freezing levels following fear conditioning did not differ between control animals (M = 43.7, SD = 5.08) and SPS-exposed animals (M = 41.8, SD = 3.98); t(24) = 0.305; p = 0.76 (Fig. 5a). Freezing was also not significantly different on the fear extinction day between control animals (M = 25.4, SD = 4.98) and SPS-exposed animals (M = 37.7, SD = 4.03); t(24) = 1.94; p = 0.064 (Fig. 5b). Extinction recall (Fig. 5c) replicated previous work showing extinction recall deficits in SPS-exposed animals (Knox et al. 2012). SPS-exposed rats (M = 18.1, SD = 4.6) froze significantly more than control animals (M = 6.0, SD = 2.0); (t(24) = 2.12, p = 0.04) during extinction recall, indicating impaired recall of the extinction memory (Fig. 5c).
SPS impairs fear extinction recall. SPS-exposed and control animals displayed similar levels of freezing following fear conditioning (a) and extinction (b). However, SPS-exposed animals show impaired extinction recall and significantly greater freezing on the extinction recall task (c) (* = p value < 0.05)
Baseline sleep does not predict freezing responses to fear conditioning
We hypothesized that the impairment of fear-related memories on the fear extinction recall testing day that we see in SPS-exposed animals may correlate with their baseline sleep parameters. Baseline percentages of time spent in the states of REM sleep, NREM sleep, transition to REM sleep, and waking were calculated for (1) the entire day (24 h), (2) for the sleep phase (12 h), and (3) for the active phase (12 h). These sleep parameters were then correlated with the average percent time each animal froze during (1) fear conditioning, (2) fear extinction, and (3) fear extinction recall. Linear regression correlation coefficients and p values are reported in Table 1. Baseline REM sleep, NREM sleep, transition to REM sleep, and wake times did not correlate with freezing values on the fear conditioning, fear extinction, or extinction recall days.
The change in REM sleep from baseline following SPS exposure predicts fear-associated memory impairments
Freezing responses in individual SPS-exposed animals on the fear extinction recall day were correlated with individual differences in the sleep response immediately following SPS to determine whether PTSD-like phenotype susceptibility could be predicted by sleep changes after SPS exposure. Changes in REM sleep amounts from baseline during the sleep phase (ZT 0–12) immediately following SPS exposure correlated with freezing on the extinction recall task a week later (R 2 = 69.3 %, p = 0.0001) (Fig. 6a). Individual increases in REM sleep amounts during the next active phase after SPS, however, did not correlate with freezing levels on the extinction recall day (R 2 = 0.02 %, p = 0.96) (Fig. 6b). Other than the correlation with REM sleep amounts following SPS exposure during the sleep phase, no other sleep phase or active phase change in sleep-state percent time significantly correlated with freezing levels on the extinction recall day (data not shown).
Changes in REM sleep during the inactive phase predict severity of PTSD-like symptoms. Correlation of freezing with the change in REM sleep during the sleep phase and active phase revealed that the animals with the highest amount of freezing also had the greatest increases in REM sleep during the sleep phase immediately after SPS exposure (R 2 = 69.3 %, p = 0.0001) (a). No correlation exits between REM sleep during the active phase and subsequent performance on fear extinction recall (b)
Theta and spindle power during transition to REM predicts fear-associated memory impairments
We calculated daily averages of EEG spectral power in SPS-exposed rats (N = 10) for each sleep state over the entire 9-day experiment. One-way ANOVA revealed no significant alterations in overall spectral power (0.1–30 Hz) over the 9 days of recording during REM sleep [F(8, 90) = 0.70, p = 0.68], NREM sleep [F(8, 90) = 0.78, p = 0.62], transition to REM sleep [F(8, 90) = 0.88, p = 0.54], active waking [F(8, 90) = 0.13, p = 0.99], or quiet waking [F(8, 90) = 0.43, p = 0.89]. Representative data from one animal are shown in Supplemental Figure S1A–E.
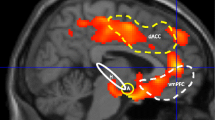
Changes in theta power (4–10 Hz) and spindle power (10–15 Hz) spectral values were additionally assessed from baseline to day 9 (100 × (power day 9/power day 1) − 100) and were found to correlate with freezing values on the fear extinction recall day. Transition to REM sleep showed a significant negative correlation of both theta (R 2 = 55.5 %, p = 0.013, Fig. 7a) and spindle power (R 2 = 39.9 %, p = 0.037, Fig. 7b) with freezing levels on the extinction recall day. Bigger reductions in theta and spindle power corresponded with more freezing. Comparison of average theta power (R 2 = 27.0 %, p = 0.12), and spindle power (R 2 = 7.3 %, p = 0.42), during REM sleep to freezing on the extinction recall task approached, but did not reach, statistical significance. Values of theta and spindle power during wake and NREM sleep also did not correlate with freezing on the extinction recall task (data not shown).
Discussion
We found that changes in REM sleep during the sleep phase that immediately follows SPS exposure predict PTSD-like phenotype development. Increased REM sleep within 8 h of SPS exposure correlated with the PTSD-like phenotype of impaired fear extinction recall. These results are, at first glance, somewhat paradoxical. REM sleep plays an important role in processing emotional experiences (Levin and Nielsen 2007; Walker 2009, 2010; Walker and van der Helm 2009; van der Helm et al. 2011). Therefore, if increased REM sleep improves the processing of emotions, then the increase we see following SPS should be working to preserve fear memory function. However, fear extinction recall is most impaired in the animals with the largest increase in REM sleep following traumatic experience. These data may be resolved if one considers the possibility that immediate increases in REM sleep by trauma might be maladaptive relative to REM sleep that occurs well after a traumatic event. Additionally, changes in REM sleep in response to stress have been shown to be sensitive to previous stressor exposure (Greenwood et al. 2014). Further experimentation is required to understand the role of REM sleep immediately following a stressful event in processing emotional memories.
In addition, theta and sigma power during sleep once the PTSD phenotype was established also predicted susceptibility to emotional learning impairments that characterize PTSD. Indeed, humans susceptible to acquiring PTSD show lower REM sleep theta power compared to resilient individuals in the months following trauma exposure (Cowdin et al. 2014). Earlier evidence indicates that reduced theta power interferes with memory processing (Vanderwolf and Stewart 1986). Thus, theta power reductions may limit the effectiveness of the limbic system in balancing emotional memories. Similarly, spindles characterizing the transition to REM sleep state have been correlated with the ability to consolidate memories across sleep in multiple studies (Fogel et al. 2007; Fogel and Smith 2011). Our finding that reductions in sleep spindles after SPS predict reductions in fear extinction recall concur with the finding that transition to REM sleep serves to integrate new information into old schema and the idea that sleep spindles serve memory consolidation (Poe et al. 2010; Tamminen et al. 2010; Watts et al. 2012).
Assessing sleep alterations after trauma exposure may help to identify sleep characteristics in clinical populations susceptible to acquiring PTSD. Indeed, these sleep biomarkers may serve to improve clinical interventions, improve outcomes after trauma exposure, or enhance resilience to PTSD. The data presented here show that SPS results in both acute and long-term changes in sleep, sleep architecture, and fear-related memory function. These sleep changes may serve as targets for behavioral or pharmacological interventions in the future. For example, the increase in REM sleep bout length during the sleep phase (shown on days 6, 7, 8, and 9; Fig. 4), the decreases in transition to REM theta and spindle spectral power on day 9, and the increase in the amount of REM sleep that permeates the sleep phase immediately following SPS exposure (Fig. 6) identify both early and delayed time windows which may be critical for PTSD onset. In line with this hypothesis, sleep deprivation performed immediately following a traumatic experience (Cohen et al. 2012) has been shown to ameliorate stress-induced impairments in biological and behavioral function. Further experimentation is required to understand the significance of sleep alterations following stress. However, identification of sleep differences in adaptive and maladaptive responses to stress is a critical first step in understanding the role that sleep plays in mediating PTSD onset.
In the current study, all animals were allowed to sleep ad libitum. No constraints were placed on their sleep time prior to or after SPS, and, as a result, most of these animals slept similarly at baseline. In human populations, however, the time spent asleep per day can vary significantly due to task demands imposed by school, work, or self-selected entertainment that limit our sleep opportunities. It has been hypothesized that poor sleep and nightmares prior to trauma exposure may increase susceptibility to PTSD in military personnel (van Liempt 2012; van Liempt et al. 2013). The data shown here suggest that baseline sleep prior to SPS is not predictive of PTSD-like phenotype development. However, there were no manipulations performed to assess the role of poor sleep (fragmentation or short sleep duration, for example) prior to or after experiencing trauma. Future studies are required to assess the role of sleep prior to experiencing stress in facilitating the development of PTSD.
To our knowledge, these data are the first of their kind to suggest that sleep changes following stress exposure may predict adaptability of learning systems. The fear extinction recall phenotype reported here and in previous work (Knox et al. 2012) mimics that in humans with PTSD (Milad et al. 2009) and suggests that sleep is playing a critical role in regulating the neural circuitry of fear-associated memory processing.
Stress is uniquely perceived, processed, and regulated by individuals (Charney 2004). Risk factors and resilience factors have been identified that facilitate our understanding of how traumatic events lead to PTSD (Brewin et al. 2000). Indeed, resilience may lie in biological mechanisms unique to these individuals or some combination of unknown factors (Koenen et al. 2009). However, if biological mechanisms exist which regulate how stress is perceived and regulated, they are currently poorly understood. Interestingly, sleep disturbances are a nearly ubiquitous feature of PTSD, making sleep and sleep disturbances unique candidates for understanding how stress is regulated. We have identified features of sleep that may serve as biomarkers of sensitivity to PTSD acquisition and have identified windows of time that may be critical for the development of PTSD. These findings serve as a foundation for the further elucidation of the molecular and anatomical mechanisms that regulate the interaction between sleep and stress.
Abbreviations
- SPS:
-
Single prolonged stress
- REM sleep:
-
Rapid eye movement sleep
- NREM sleep:
-
Non-rapid eye movement sleep
- PTSD:
-
Posttraumatic stress disorder
- EEG:
-
Electroencephalographic
- EMG:
-
Electromyographic
References
American Psychiatric Association (2013) Trauma- and stressor-related disorders. In: Diagnostic and statistical manual of mental disorders, 5th edn. doi:10.1176/appi.books.9780890425596.dsm07
Brewin CR, Andrews B, Valentine JD (2000) Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 68:748–766
Brown TH, Mellman TA, Alfano CA, Weems CF (2011) Sleep fears, sleep disturbance, and PTSD symptoms in minority youth exposed to Hurricane Katrina. J Trauma Stress 24:575–580. doi:10.1002/jts.20680
Charney DS (2004) Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry 161:195–216
Cohen S, Kozlovsky N, Matar MA, Kaplan Z, Zohar J, Cohen H (2012) Post-exposure sleep deprivation facilitates correctly timed interactions between glucocorticoid and adrenergic systems, which attenuate traumatic stress responses. Neuropsychopharmacology 37:2388–2404. doi:10.1038/npp.2012.94
Cowdin N, Kobayashi I, Mellman TA (2014) Theta frequency activity during rapid eye movement (REM) sleep is greater in people with resilience versus PTSD. Exp Brain Res. doi:10.1007/s00221-014-3857-5
Fogel SM, Smith CT (2011) The function of the sleep spindle: a physiological index of intelligence and a mechanism for sleep-dependent memory consolidation. Neurosci Biobehav Rev 35:1154–1165. doi:10.1016/j.neubiorev.2010.12.003
Fogel SM, Nader R, Cote KA, Smith CT (2007) Sleep spindles and learning potential. Behav Neurosci 121:1–10
Germain A (2013) Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry 170:372–382. doi:10.1176/appi.ajp.2012.12040432
Greenwood BN, Thompson RS, Opp MR, Fleshner M (2014) Repeated exposure to conditioned fear stress increases anxiety and delays sleep recovery following exposure to an acute traumatic stressor. Front Psychiatry 5:146. doi:10.3389/fpsyt.2014.00146
Gross BA, Walsh CM, Turakhia AA, Booth V, Mashour GA, Poe GR (2009) Open-source logic-based automated sleep scoring software using electrophysiological recordings in rats. J Neurosci Methods 184:10–18. doi:10.1016/j.jneumeth.2009.07.009
Knox D, George SA, Fitzpatrick CJ, Rabinak CA, Maren S, Liberzon I (2012) Single prolonged stress disrupts retention of extinguished fear in rats. Learn Mem 19:43–49. doi:10.1101/lm.024356.111
Koenen KC, Amstadter AB, Nugent NR (2009) Gene–environment interaction in posttraumatic stress disorder: an update. J Trauma Stress 22:416–426. doi:10.1002/jts.20435
Levin R, Nielsen TA (2007) Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull 133:482–528. doi:10.1037/0033-2909.133.3.482
Liberzon I, Krstov M, Young EA (1997) Stress–restress: effects on ACTH and fast feedback. Psychoneuroendocrinology 22:443–453
Liberzon I, Lopez JF, Flagel SB, Vazquez DM, Young EA (1999) Differential regulation of hippocampal glucocorticoid receptors mRNA and fast feedback: relevance to post-traumatic stress disorder. J Neuroendocrinol 11:11–17
Mellman TA, David D, Kulick-Bell R, Hebding J, Nolan B (1995) Sleep disturbance and its relationship to psychiatric morbidity after Hurricane Andrew. Am J Psychiatry 152:1659–1663
Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B (2002) REM sleep and the early development of posttraumatic stress disorder. Am J Psychiatry 159:1696–1701
Merica H, Blois R (1997) Relationship between the time courses of power in the frequency bands of human sleep EEG. Neurophysiol Clin 27:116–128. doi:10.1016/S0987-7053(97)85664-X
Milad MR, Pitman RK, Ellis CB et al (2009) Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder. Biol Psychiatry 66:1075–1082. doi:10.1016/j.biopsych.2009.06.026
Mitchell DJ, McNaughton N, Flanagan D, Kirk IJ (2008) Frontal-midline theta from the perspective of hippocampal “theta”. Prog Neurobiol 86:156–185. doi:10.1016/j.pneurobio.2008.09.005
Pitman RK, Rasmusson AM, Koenen KC et al (2012) Biological studies of post-traumatic stress disorder. Nat Rev Neurosci 13:769–787. doi:10.1038/nrn3339
Poe GR, Walsh CM, Bjorness TE (2010) Both duration and timing of sleep are important to memory consolidation. Sleep 33:1277–1278
Ross RJ (2014) The changing REM sleep signature of posttraumatic stress disorder. Sleep 37:1281–1282. doi:10.5665/sleep.3912
Ross RJ, Ball WA, Sullivan KA, Caroff SN (1989) Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry 146:697–707
Tamminen J, Payne JD, Stickgold R, Wamsley EJ, Gaskell MG (2010) Sleep spindle activity is associated with the integration of new memories and existing knowledge. J Neurosci 30:14356–14360. doi:10.1523/JNEUROSCI.3028-10.2010
van der Helm E, Yao J, Dutt S, Rao V, Saletin JM, Walker MP (2011) REM sleep depotentiates amygdala activity to previous emotional experiences. Curr Biol 21:2029–2032. doi:10.1016/j.cub.2011.10.052
van Liempt S (2012) PhD summary: sleep disturbances and PTSD: a perpetual circle?
van Liempt S, van Zuiden M, Westenberg H, Super A, Vermetten E (2013) Impact of impaired sleep on the development of PTSD symptoms in combat veterans: a prospective longitudinal cohort study. Depress Anxiety. doi:10.1002/da.22054
Vanderheyden WM, Poe GR, Liberzon I (2014) Trauma exposure and sleep: using a rodent model to understand sleep function in PTSD. Exp Brain Res. doi:10.1007/s00221-014-3890-4
Vanderwolf CH, Stewart DJ (1986) Joint cholinergic–serotonergic control of neocortical and hippocampal electrical activity in relation to behavior: effects of scopolamine, ditran, trifluoperazine and amphetamine. Physiol Behav 38:57–65
Walker MP (2009) The role of sleep in cognition and emotion. Ann N Y Acad Sci 1156:168–197. doi:10.1111/j.1749-6632.2009.04416.x
Walker MP (2010) Sleep, memory and emotion. Prog Brain Res 185:49–68. doi:10.1016/B978-0-444-53702-7.00004-X
Walker MP, van der Helm E (2009) Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull 135:731–748. doi:10.1037/a0016570
Watts A, Gritton HJ, Sweigart J, Poe GR (2012) Antidepressant suppression of non-REM sleep spindles and REM sleep impairs hippocampus-dependent learning while augmenting striatum-dependent learning. J Neurosci 32:13411–13420. doi:10.1523/Jneurosci.0170-12.2012
Wellman LL, Yang L, Ambrozewicz MA, Machida M, Sanford LD (2013) Basolateral amygdala and the regulation of fear-conditioned changes in sleep: role of corticotropin-releasing factor. Sleep 36:471–480. doi:10.5665/sleep.2526
Yamamoto S, Morinobu S, Takei S, Fuchikami M, Matsuki A, Yamawaki S, Liberzon I (2009) Single prolonged stress: toward an animal model of posttraumatic stress disorder. Depress Anxiety 26:1110–1117. doi:10.1002/da.20629
Acknowledgments
This work was funded by NIHRO1-MH60670 (G.P.), T32HL110952-01A1 (W.V.), and the Department of Anesthesiology at the University of Michigan.
Conflict of interest
The authors disclose no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vanderheyden, W.M., George, S.A., Urpa, L. et al. Sleep alterations following exposure to stress predict fear-associated memory impairments in a rodent model of PTSD. Exp Brain Res 233, 2335–2346 (2015). https://doi.org/10.1007/s00221-015-4302-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-015-4302-0