Abstract
Summary
Hip fractures are common in the elderly, and many patients with hip fractures have low vitamin D levels. This study found that severe vitamin D deficiency is linked to poorer recovery of function and quality of life after hip fracture surgery.
Introduction
Vitamin D deficiency is prevalent in hip fracture patients and associated with increased mortality and complications. However, there is limited long-term data on how vitamin D levels affect functional outcomes after hip fracture surgery. The aim of this study is to ascertain the association between vitamin D levels and recovery from hip surgery.
Methods
Patients who underwent hip fracture surgery from January 2012 to December 2016 and had vitamin D levels assessed during admission were included. Retrospective analysis was performed on patients’ demographic data such as age, gender and clinical parameters such as preoperative vitamin D, haemoglobin levels, Charlson Comorbidity Index (CCI), and type and site of surgery. Patients were divided according to four different vitamin D levels—severe vitamin D deficiency (≤10 ng/mL), mild deficiency (10-20 ng/ml), insufficiency (20-30 ng/ml), and normal (>30ng/ml). Functional outcomes were measured by Harris Hip Score (HHS), Parker Mobility Score (PMS), and individual domains of 36-Item Short Form Health Survey (SF36). Univariate and multivariate analyses were conducted to examine the association between vitamin D deficiency and functional outcome scores.
Results
Out of 664 patients identified, 9% had severe vitamin D deficiency and 39% mild deficiency. Patients with severe vitamin D deficiency had significantly poorer baseline and 6-month PMS and SF36 Physical Functioning (PF). In multivariate analysis, severe vitamin D deficiency was associated with lower 6-month PMS and SF36 PF.
Conclusion
Preoperative severe vitamin D deficiency is an independent risk factor for poorer recovery of function and quality of life after hip fracture surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is an important primary cause of disability in the elderly, increasing the burden of disease in the population and leading to substantial loss of healthy life-years in elderly people [1]. Hip fracture patients have a high prevalence of vitamin D deficiency which has been associated with osteoporosis, muscle weakness, higher fall, and fracture risk in the elderly population [2, 3]. In patients with hip fractures, vitamin D deficiency has also been associated with increased short-term and long-term mortality [4,5,6,7,8], increased complications [5], and poorer cognitive status [9].
There are controversies in the literature concerning vitamin D, and the definition of optimal vitamin D status is still unclear in the literature [10]. There is also no defined link between vitamin D levels and propensity for other metabolic bone diseases apart from rickets, such as osteoporosis which is a well-established risk factor for hip fracture.
Currently, studies have demonstrated that low vitamin D levels are associated with poorer functional outcomes, but some of these studies only assessed short-term outcomes [11, 12], had population sizes less than two hundred patients [12,13,14], did not account for pre-fracture baseline function [11], and importantly, did not assess patients utilizing previously defined vitamin D thresholds [12, 14, 15]. Evaluating serum vitamin D thresholds through studying the effect of vitamin D on functional outcomes may help define target levels of serum vitamin D to optimize recovery of hip fracture patients.
Aim
The aim of this study is to assess for any association between vitamin D levels on admission, stratified along previously defined vitamin D thresholds, and 6-month functional outcome scores after hip fracture surgery, after adjusting for baseline function and other confounders.
Hypothesis
Our hypothesis is that severe vitamin D deficiency is an independent risk factor for poorer 6-month functional outcome after surgery for hip fractures.
Methods
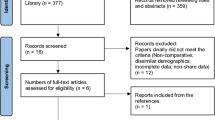
Patient selection
The medical records of patients who underwent hip fracture surgery in our institution, Singapore General Hospital, from January 2012 to December 2016, and had vitamin D levels assessed during admission, were reviewed.
We excluded patients who had pathological fractures, prior surgeries in involved hips, and those resulting from high energy trauma.
Retrospective analysis was performed on patients’ demographic data such as age, gender, and clinical parameters such as preoperative vitamin D and haemoglobin levels measured on admission, co-morbidity burden as assessed by Charlson Comorbidity Index (CCI), and type and site of surgery.
Vitamin D definition
Vitamin D in this paper refers to total serum 25-hydroxycholecalciferol, which is reported elsewhere as 25-hydroxyvitamin D or 25(OH) vitamin D or calcifediol. Vitamin D levels were assessed on admission together with other parameters such as serum calcium for bone health assessment and osteoporosis workup.
According to definitions by the Endocrine Society [2], total serum 25-hydroxycholecalciferol levels between of 20–30 ng/ml is termed as vitamin D insufficiency, and that of below 20 ng/ml is termed as deficiency.
Our study utilized ≤10 ng/ml to define severe deficiency; this measure was used in previous studies [4, 5, 16, 17]. Thus, we defined mild vitamin D deficiency using levels of 10–20ng/ml in this study and previous definitions of vitamin D insufficiency (20–30 ng/ml) and normal vitamin D (>30 ng/ml) were retained.
Anaemia definition
Anaemia was defined according to World Health Organization (WHO) gender-based classification. In men, mild anaemia was defined at haemoglobin 11.0–12.9 g/dL; in women, mild anaemia was defined at haemoglobin 11.0–11.9 g/dL. While for both genders, moderate anaemia was defined at haemoglobin 8.0–10.9g/dL and severe anaemia was defined at haemoglobin < 8.0g/dL
Charlson Comorbidity Index
This study used Charlson Comorbidity Index (CCI) to assess co-morbidity burden in hip fracture patients. The CCI score is based on number of conditions including previous myocardial infarction, stroke, and liver disease that are each assigned different weights, with a higher weight representing more severe morbidity. The summation of the weighted comorbidity scores results in a summary score. For statistical analysis, patients in this study were divided into two groups according to their CCI score, CCI 0–1 and CCI ≥2.
Functional outcomes
Functional outcome was measured by the Harris Hip Score and the Parker Mobility Score, while quality of life was assessed using the various domains of the 36-Item Short Form Health Survey (SF36). Harris Hip Score is an assessment of patients’ hip with a maximum score of 100 points. Greater emphasis is placed on function as assessed by activities of daily living, gait (47 points), and pain (44 points), while range of motion (5 points) and absence of deformity (4 points) have less weightage in the Harris Hip Score. Parker Mobility Score measures patients’ ambulatory status in different situations—indoors, outdoors, or whilst doing shopping, and scores patients from 0 to 9. The use of SF36, Parker Mobility Score, and Harris Hip Score to evaluate outcomes after hip fracture surgery has been validated in previous recent studies [13, 18]. Assessment was performed by independent third-party trained physiotherapists from our Orthopaedic Diagnostic Centre. These assessments were done at baseline on admission and at follow up at 6 months post-discharge at the outpatient clinic. Assessments were done independent of the study and were routinely done in all hip fracture patients.
The duration of 6 months was chosen in view of previous studies which show that functional recovery after hip fracture may be largely complete in the first 6 months [13] and is sufficient to assess midterm recovery from a hip fracture.
For the SF36, patients are assessed using eight different domains divided into two groups: four physical health domains which include physical functioning (SF36 PF), role limitations as a result of physical health problems (SF36 RP), bodily pain (SF36 BP), and general health (SF36 GH), as well as four mental health domains which include vitality (SF36 VI), social functioning (SF36 SF), role limitations as a result of emotional problems (SF36 RE), and mental health perceptions (SF 36 MH).
Baseline pre-operative Harris Hip Score was unavailable, and Harris Hip Score was only assessed at 6 months, as it is not practical to assess pre-operative deformity and range of motion upon admission, due to acute pain.
Statistical analysis
Analysis was performed to determine any correlation between vitamin D levels, and various demographic and clinical parameters. Spearman correlation was performed between two continuous/ordinal variables to determine any monotonic relationships, while the Mann-Whitney U test was used to determine if median vitamin D levels were similar between groups of different demographic or clinical parameters.
Patients were subsequently divided into 4 groups according to the vitamin D levels previously defined. Univariate analysis was performed using one-way ANOVA to determine if there was any difference in baseline and 6-month functional outcome scores among the different vitamin D groups.
Multivariate analysis with general linear model was performed on the respective 6-month scores that demonstrate statistically significant differences in outcome amongst vitamin D groups, in order to ascertain the association between vitamin D and recovery from hip surgery, while accounting for other confounders.
All analyses were conducted using SPSS Statistics for Windows version 22.0 (IBM Corp., Armonk, NY). A p < 0.05 is considered statistically significant.
Results
Hospital surgical logs identified 664 patients who underwent surgical treatment of osteoporotic hip fractures with available serum total 25-hydroxyvitamin D level recorded between January 2012 and December 2016. The characteristics of our cohort can be seen in Table 1. This study population had a mean age of 77 years; 29% were male and 71% female. Joint-replacing procedures were performed in 55%, and joint-preserving (fixation) procedures in 45%. Of these 664 patients, 9% had severe vitamin D deficiency (≤10 ng/mL), 39% mild vitamin D deficiency (10–20 ng/ml), 42% vitamin D insufficiency (20–30 ng/ml), and 10% normal vitamin D levels (>30ng/ml). Univariate analysis using one-way ANOVA demonstrated that there was a significant difference in 6-month outcome across vitamin D groups as assessed by Parker Mobility Score (p =.003) and SF36 PF (p=.047) (Table 2). There was no significant difference found among vitamin D groups for the other outcome scores.
In a separate analysis, increasing age was significantly correlated to poorer Parker Mobility Score and SF36 PF at 6 months. Parker Mobility Score and SF36 PF were both inversely associated with increasing age (p<0.001 for both), and thus, an initial multivariate analysis investigating the association between vitamin D level, age, and functional outcomes was performed which demonstrated that there is a significant difference in both 6-month PMS and SF36 PF between patients in severe vitamin D deficiency group and patients in all the other vitamin D groups when corrected only for patient’s age (Table 3).
After further multivariate analysis, adjusting also for preoperative anaemia, type of surgery, gender, other co-morbidities, and baseline score, severe vitamin D deficiency was found to be an independent risk factor for lower 6-month Parker Mobility Score and SF36 PF(Table 4). Severe vitamin D deficiency was still found to be an independent risk factor for lower 6-month Parker Mobility Score and SF36 PF in the multivariate analysis when baseline scores were excluded from the analysis. Preoperative anaemia, age, and baseline score were found to be independent risk factors for poorer Parker Mobility Score and SF36 PF after hip fracture surgery. Additionally, CCI was found to be an independent risk factor for Parker Mobility Score after hip fracture surgery.
Discussion
The prevalence of vitamin D deficiency (<20ng/ml) in our cohort of surgically treated hip fracture is 48%, which is significantly lower than reported rates of vitamin D deficiency in other study populations (77–87%) [4, 5, 7]. We postulate that this could be due to our equatorial climate. Vitamin D supplementation, type of dwelling, and seasonality have been shown to affect vitamin D levels of hip fracture patients [19]. There was no association between serum vitamin D levels and other clinical parameters such as age, comorbidities, anaemia, and gender (Table 5), which is consistent with the literature [20].
Our study found an association between lower vitamin D levels and poorer baseline ambulatory function based on Parker Mobility Score and quality of life in physical functioning (Tables 2 and 3). The latter measure encompasses carrying out activities of daily living such as groceries, bathing, and dressing. In addition, severe vitamin D deficiency (<10ng/ml) was an independent risk factor for lower Parker Mobility Score and SF36 PF at 6 months after hip fracture surgery in this group, even after accounting for the baseline differences above, meaning that the detrimental effect of severe vitamin D is sustained till at least midterm recovery after a hip fracture.
Our findings build upon the findings of previous studies. Pioli found an association between severe vitamin D deficiency and recovery of pre-fall ambulatory status at 6 months [15]. Di Monaco found an association between severe vitamin D deficiency and a poorer Barthel Index score, which assesses independence in activities of daily living (ADL), after discharge from rehabilitation facilities [11]. Other studies by Leboff and Fischer found associations between severe vitamin D deficiency and poorer lower limb strength over 1 year, and this may indirectly affect ambulatory function and quality of life [13, 14].
While the above studies were able to demonstrate an association between vitamin D deficiency and outcomes after hip fracture surgery, most of these studies were only able to demonstrate this association at a single cut-off value around the range of 6–10ng/ml or severe vitamin D deficiency, similar to that found in our study [12,13,14,15].
However, the study by Di Monaco was able to demonstrate a difference in outcome between mild vitamin D deficiency and vitamin D insufficiency, as they used validated vitamin D classes to determine their prognostic capability of the functional recovery after hip fracture [11]. They found that there was a stepwise decrease in ADL when comparing patients with vitamin D insufficiency to those with mild deficiency, and then again between patients who had mild deficiency to those with severe deficiency. There was however no difference in ADL between patients with insufficiency and normal vitamin D levels. Hence, they recommended that patients with vitamin D deficiency should receive supplementation but that there was minimal evidence from their study to increase the threshold for vitamin D supplementation beyond 20ng/ml [11].
We were unable to demonstrate such a difference in outcome between patients with mild vitamin D deficiency and vitamin D insufficiency. This may be due to the fact that their outcomes were assessed at discharge from rehabilitation facility, whilst ours were assessed at 6 months post-operatively. Their study also utilized a different set of validated outcome scores from this study.
In patients who sustain hip fractures, the majority of which require surgical intervention, Vitamin D deficiency is related to increased complications including pneumonia [5], thromboembolic events [5], and poorer cognitive status [9] which affects rehabilitation after hip fracture surgery. Baseline vitamin D function may also affect recovery after hip fracture through its skeletal and extra-skeletal effects. Vitamin D deficiency is linked to reduced muscle strength and function [3], increased fracture comminution and hence slower recovery [20], impaired bone formation in patients with hip fracture [21], and altered bone turnover markers which are surrogate measures of fracture healing [22]. Our study consolidates the point that pre- and post-hip fracture quality of life is affected by severe Vitamin D deficiency, largely in the domains of physical functioning, consistent with the known effects of Vitamin D on the musculoskeletal system. This is especially important as we strive to develop a healthy and active aging population who may remain socioeconomically viable well into their senior years.
Hence, understanding the association between low vitamin D levels and recovery from hip fracture can help clinicians to identify patients who are at risk for poorer recovery as a target for focused rehabilitation and potentially nutritional supplementation. Further studies are still required to confirm the benefit of vitamin D supplementation in the hip fracture population, many of whom have severe vitamin D deficiency.
Strengths and limitations
This is the study of a large cohort of elderly adults with hip fracture that demonstrates the negative association between severe preoperative serum vitamin D deficiency and midterm functional recovery after hip fracture surgery even after accounting for other confounders. Functional recovery and quality of life were assessed using validated tools. We have a follow-up rate of about 92% of patients who were able to return for assessment at 6 months.
This study however was unable to account for patients who received vitamin D supplementation before their fracture and was also unable to study the effect of vitamin D supplementation after surgical treatment for hip fractures. Our study design was only able to elucidate the association between vitamin D at admission and functional recovery, but unable to determine causality.
Conclusion
Prevalence of vitamin D deficiency is high in surgically treated hip fracture patients. Preoperative severe vitamin D deficiency has been shown to be an independent risk factor for slower recovery of function and quality of life after hip fracture surgery. Prospective studies are required to confirm the association between vitamin D and outcomes after hip fracture surgery, to re-define optimal vitamin D levels, and to investigate if vitamin D supplementation can improve recovery in patients with hip fractures.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Papadimitriou N, Tsilidis KK, Orfanos P, Benetou V, Ntzani EE, Soerjomataram I, Künn-Nelen A, Pettersson-Kymmer U, Eriksson S, Brenner H, Schöttker B, Saum KU, Holleczek B, Grodstein FD, Feskanich D, Orsini N, Wolk A, Bellavia A, Wilsgaard T, Jørgensen L, Boffetta P, Trichopoulos D, Trichopoulou A (2017) Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health 2:e239–e246
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J (2019) Skeletal and extraskeletal actions of vitamin d: current evidence and outstanding questions. Endocr Rev 40:1109–1151
Lee G-H, Lim J-W, Park Y-G, Ha Y-C (2015) Vitamin D deficiency is highly concomitant but not strong risk factor for mortality in patients aged 50 year and older with hip fracture. J Bone Metab 22:205–209
Fakler JKM, Grafe A, Dinger J, Josten C, Aust G (2016) Perioperative risk factors in patients with a femoral neck fracture - influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord 17:51
Nurmi-Lüthje I, Lüthje P, Kaukonen J-P, Kataja M (2015) Positive effects of a sufficient pre-fracture serum vitamin D level on the long-term survival of hip fracture patients in finland: a minimum 11-year follow-up. Drugs Aging 32:477–486
Schaller F, Sidelnikov E, Theiler R, Egli A, Staehelin HB, Dick W, Dawson-Hughes B, Grob D, Platz A, Can U, Bischoff-Ferrari HA (2012) Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture. Bone 51:347–352
Fisher A, Fisher L, Srikusalanukul W, Smith PN (2018) Usefulness of simple biomarkers at admission as independent indicators and predictors of in-hospital mortality in older hip fracture patients. Injury 49:829–840
Carrillo González I, Martínez-Ramírez MJ, Tenorio Jiménez C et al (2020) 25-hydroxyvitamin D levels in the early healing of osteoporotic hip fracture and their relationship with clinical outcome. Nutr Hosp 37(2):327–334. https://doi.org/10.20960/nh.02427
Giustina A, Adler RA, Binkley N, Bouillon R, Ebeling PR, Lazaretti-Castro M, Marcocci C, Rizzoli R, Sempos CT, Bilezikian JP (2019) Controversies in vitamin D: summary statement from an international conference. J Clin Endocrinol Metab 104:234–240
Di Monaco M, Castiglioni C, Di Carlo S et al (2019) Classes of vitamin D status and functional outcome after hip fracture: a prospective, short-term study of 1350 inpatients. Eur J Phys Rehabil Med 55:56–62
Toldy E, Salamon A, Kálmán B et al (2018) Prognostic relevance of circulating 25OHD fractions for early recovery and survival in patients with hip fracture. J Clin Med Res 7:193. https://doi.org/10.3390/jcm7080193
Fischer K, Trombik M, Freystätter G, Egli A, Theiler R, Bischoff-Ferrari HA (2019) Timeline of functional recovery after hip fracture in seniors aged 65 and older: a prospective observational analysis. Osteoporos Int 30:1371–1381
LeBoff MS, Hawkes WG, Glowacki J et al (2008) Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int 19:1283–1290
Pioli G, Lauretani F, Pellicciotti F, Pignedoli P, Bendini C, Davoli ML, Martini E, Zagatti A, Giordano A, Nardelli A, Zurlo A, Bianchini D, Sabetta E, Ferrari A, Tedeschi C, Lunardelli ML (2016) Modifiable and non-modifiable risk factors affecting walking recovery after hip fracture. Osteoporos Int 27:2009–2016
Bolland MJ, Grey A, Avenell A (2018) Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol 6:847–858
Kennel KA, Drake MT, Hurley DL (2010) Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc 85:752–757 quiz 757–8
Sim YE, Sim S-ED, Seng C, Howe TS, Koh SB, Abdullah HR (2018) Preoperative anemia, functional outcomes, and quality of life after hip fracture surgery. J Am Geriatr Soc 66:1524–1531
Bischoff-Ferrari HA, Can U, Staehelin HB, Platz A, Henschkowski J, Michel BA, Dawson-Hughes B, Theiler R (2008) Severe vitamin D deficiency in Swiss hip fracture patients. Bone 42:597–602
Lakkireddy M, Mudavath SV, Karra ML, Arora AJ (2019) Hypovitaminosis D in patients with osteoporotic hip fractures. J Clin Orthop Trauma 10:768–773
Sharma DK, Sawyer RK, Robertson TS et al (2019) Elevated serum 25-hydroxyvitamin D levels are associated with improved bone formation and micro-structural measures in elderly hip fracture patients. J Clin Med Res 8:–1988. https://doi.org/10.3390/jcm8111988
Stewart CC, O’Hara NN, Orwig D et al (2019) Serum 25(OH)D is associated with an altered bone turnover marker response after a hip fracture. J Orthop Res 37:535–540
Code availability
Not applicable
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study involves human data, and institutional review board approval was obtained (Singhealth CIRB 2015/2134) before the start of this single-centre retrospective cohort study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Waiver of consent was approved for this type of retrospective study with anonymized patient records.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sim, D., Tay, K., Howe, T. et al. Preoperative severe vitamin D deficiency is a significant independent risk factor for poorer functional outcome and quality of life 6 months after surgery for fragility hip fractures. Osteoporos Int 32, 2217–2224 (2021). https://doi.org/10.1007/s00198-021-05970-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-05970-y