Abstract
Summary
Modifiable and non-modifiable predictors of mobility recovery were analyzed on a sample of 774 hip fracture patients according to pre-fracture abilities. Overall predictors were mostly non-modifiable factors related to frailty of patients with the exception of 25-hydroxyvitamin D concentration which significantly affected walking recovery, especially in patients with higher pre-fracture performance.
Introduction
This study aims to investigate mobility changes after hip fracture with the aim of identifying modifiable and non-modifiable predictors of mobility recovery according to different pre-fracture abilities.
Methods
This is a prospective inception cohort study of consecutive older patients, admitted with a fragility hip fracture in three Hospitals of Emilia Romagna (Italy). A sample of 774 patients alive at the sixth month was divided into three groups according to pre-fracture ambulation ability (group 1: mobile outdoors; group 2: mobile indoors; and group 3: mobile with help). The relationship between baseline characteristics of patients and the odds of walking recovery was analyzed using multivariate regression analysis.
Results
Mortality differed significantly among the three groups and was the highest in patients needing help to walk. Among the survivors, only 50.3 % of patients recovered walking ability. In a multivariate analysis, independent risk factors were different among the three groups. In group 1, older age, comorbidities, the use of walking devices before fracture, and low albumin level acted as negative factors while male gender, a pre-fracture high functional status, and higher 25-hydroxyvitamin D levels increased the probability of full recovery. In group 2, only pre-fracture functional status and 25-hydroxyvitamin D concentration were related to the recovery of walking ability. Pre-fracture functional status was also the only significant predictor for patients in group 3.
Conclusions
Several baseline characteristics of patients are related to the likelihood of recovering walking ability after hip fracture. The 25-hydroxyvitamin D level seems to be the only relevant modifiable factor even if the effectiveness of its supplementation has yet to be demonstrated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is a catastrophic event in older persons that often leads to disability and death [1]. Most of the surviving patients lose mobility functions and the ability to live independently [2, 3]. Several pre-fracture conditions were associated with walking recovery [4], but it is still debated which aspects of a comprehensive geriatric assessment influence mobility, in order to optimize in-hospital and out-hospital rehabilitation. Many studies showed that subjects with pre-fracture mobility limitations, reported indoors falls before fracture, and in need of walking aids have less probability to walk independently after hip fracture [5, 6]. Patients with prolonged pain after surgery were also more likely to show a catastrophic decline in the ability to walk outdoors [6]. Dementia is a known risk factor for negative outcomes after hip fracture, even if some studies showed that cognitive impairment per se does not significantly affect the functional gain if patients are referred to rehabilitation [7]. Muir et al. [8] in their systematic review concluded that there is some evidence that older adults with cognitive impairment who receive intensive inpatient rehabilitation after surgical repair may be able to gain benefits in physical function that are comparable with cognitively intact patients. Delirium has also been shown to predict negative rehabilitation outcomes mainly if superimposed on dementia [9].
On the other hand, it is an open question which type of rehabilitation program, in-hospital rehabilitation vs. out-hospital or home-rehabilitation program, should be recommended after hip fractures in older persons [10]. Optimal results could probably be obtained by tailoring a rehabilitation program to each patient, according to the level of cognitive or mobility disability even if there is not enough information to make recommendations for specific physical therapy interventions.
We investigate mobility changes after hip fracture with the aim of identifying modifiable and non-modifiable risk factors that can affect mobility recovery according to different pre-fracture abilities.
Methods
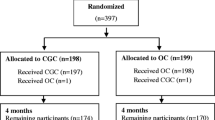
This study is a post hoc analysis of a larger prospective inception cohort study on consecutive patients, aged 75 years or older, admitted with a fragility hip fracture over a 1-year period in three General Hospitals of the Regional Healthcare System located in different districts of the Emilia Romagna Region. The samples represented unselected populations of comparable catchment areas of about 250,000 inhabitants with the exclusion of patients with fracture due to malignancy or who had sustained a fracture due to a major trauma. A detailed description of patients and data collection is presented elsewhere [5, 11]. For this study, pre-fracture wheel-chair or bedridden patients were also excluded leaving a sample of 774 patients for the analysis. Data on walking recovery were obtained through a structured telephone questionnaire to patient or caregiver after 3, 6, and 12 months. Data collected included a comprehensive geriatric assessment at admission, while during hospital stay we recorded surgical delay and the occurrence of delirium assessed by CAM tool [12]. Cognitive impairment was categorized into two groups on the basis of the number of errors at Short Portable Mental Status Questionnaire: mild-moderate for three to seven errors and severe for eight or more errors [13]. Medical burden and comorbidity were measured using the Charlson Index [14]. Severity of illness at admission was measured by the acute physiology score (APS) of APACHE II [15]. Pre-fracture functional status was also collected using the six-item Katz Index (bathing, dressing, toileting, transferring, continence, and feeding) for basic activities of daily living [16] and the eight-item Lawton Index (using the telephone, shopping, preparing food, housekeeping, doing laundry, using transportation, handling medications, and finances) for instrumental activities of daily living [17]. Each item was logged as zero in case of total or partial assistance and as one in case of complete independence.
Blood samples were also collected in the morning under fasting conditions within 24 h of hospital admission. Along with routine laboratory assessment, serum albumin and serum 25(OH) 25-hydroxyvitamin D were measured. Serum 25(OH)D was measured by radioimmunoassay (RIA) using a commercial kit (detection limit, 3.75 nmol/l; DiaSorin, Saluggia, Italy). The inter-assay coefficient of variation (CV) was between 8.2 and 11 % for 25-OHD (depending on the measured concentration).
On the basis of pre-fracture mobility, patients were categorized into three subgroups: patients able to walk independently outdoors (group 1), patients able to walk independently indoors but needing help or supervision for walking outdoors (group 2), and patients needing human help to walk (group 3). The level of dependence in walking was rated only on the basis of needing human help irrespective of the use of canes or walkers. However, the use of ambulatory devices was reported.
Categorical variables were expressed in percentages, and continuous variables were reported as mean ± standard deviation. One-way analysis of variance, Pearson’s c2 test, and the Mann–Whitney U test were used to examine differences in patients’ baseline characteristics or crude data between the groups.
Since the functional gain recovery peaked at the sixth month, we analyzed factors related to walking recovery at this point of follow-up. The main outcome was the recovery of pre-fracture walking ability: the ability to walk independently indoors and outdoors irrespective of the use of new ambulatory devices for patients in group 1; the ability to walk independently indoors with the use of ambulatory devices, if necessary, for patients in group 2; conservation of the ability to walk, even if with human help, for patients in group3.
A multivariate regression analysis was carried out in order to identify independent predictors. All variables found to be related to walking recovery were included in the multivariate analysis as continuous or dichotomous variables, as appropriate. Age was analyzed in 5-year ranks, 25-hydroxyvitamin D levels and albumin in tertiles. The interaction term between variables that are significantly associated with walking recovery from multivariate regression analysis, such as tertiles of 25-OHD*groups and 25-OHD*sex were used in a general linear model to compare the vitamin D-associated increments in walking recovery and 25-OHD between groups and the sex-associated increments in walking recovery and vitamin D between sexes.
Hazard ratios (HR) and 95 % confidence intervals (CIs) were calculated. Significance was set at p < 0.05. Statistical analysis was performed with SPSS 21.0 for Windows (SPSS Inc., Chicago, IL).
Results
Clinical characteristics of patients stratified by mobility categories before fracture are shown in Table 1. As expected, less mobile patients are slightly older, sicker, and in general with worse parameters than more independent patients. Even the type of fracture differed among groups, intracapsular fractures being significantly more frequent in mobile patients and extracapsular fracture in patients needing help to walk.
Walking recovery and mortality, according to pre-fracture mobility, at the three points of the study after surgical repair are shown in Fig. 1. As expected, mortality differed significantly among the three groups at each point and was higher in patients needing help to walk. At 1 year, mortality rates were 17 % in group 1, 30 % in group 2, and 43 % in group 3 (p < 0.01). On the other hand, patients with the highest pre-fracture performance recovered more slowly than patients with pre-fracture walking limitations. Among survivors at 3 months from fracture, only 14 % of group 1 acquired pre-fracture walking abilities compared with 35 % of group 2 and 65 % of group 3 (p < 0.0001). Even at the time of the peak of recovery at the sixth month, a significant difference in the achievement of pre-fracture functional ability was observed among the 3 groups (44, 47, and 67 %, p = 0.001).
Factors affecting walking recovery were analyzed on living patients at the sixth month (n = 604, 78 % of initial sample). The results of multivariate analyses according to the three subgroups of patients are shown in Table 2. Several factors resulted as independent risk factors able to affect walking improvement after fracture in patients of the group 1. Older age, comorbidities, the use of walking devices before fracture, and low albumin level acted as a negative factor while male gender, a pre-fracture high functional status assessed as instrumental activities of daily living (IADL) Index, and higher 25-hydroxyvitamin D levels increased the probability of full recovery to pre-fracture independence in walking. In group 2, whose subjects had limited walking abilities before fracture and needed help or supervision outdoors, only two variables seem to affect walking recovery, i.e., the pre-fracture functional status assessed as basic ADL Index, and again 25-hydroxyvitamin D level. ADL Index was also the only significant predictor of full recovery for patients in group 3. Overall independent variables affecting walking recovery were mostly non-modifiable factors in all three groups with the exception of 25-hydroxyvitamin D levels. Pre-fracture functional status is one of the most consistent variables. In the highly performing patients of group 1, who are generally fully independent in basic ADL, the IADL score was significantly related to the probability of walking recovery (per each IADL point score: HR, 1.24 (95 % CI, 1.01–1.53); p = 0.042), while in patients with some pre-fracture functional impairment, the ADL score was mainly related to the likelihood of walking recovery (per each ADL point score in group 2: HR, 1.46 (95 % CI, 1.07–2.00); p = 0.017; in group 3: HR, 1.54 (95 % CI, 1.03–2.32); p = 0.037). The serum concentration of 25-hydroxyvitamin D was quite low in this sample (mean ± SD, 10.7 ± 8.7 ng/ml) as most of the patients were below the reference range. However, ranking patients into tertiles, we found that the odds of recovering previous ambulation was about three times greater in patients with 25-hydroxyvitamin D >11 ng/ml (upper tertile) compared with patients with 25-hydroxyvitamin D <6 ng/ml (lower tertile) both in group 1 (HD, 2.9 (95 % CI, 1.23–6.85); p = 0.015) and group 2 (HD, 3.66 (95 % CI, 1.47–9.11); p = 0.005). No significant relationship was found with 25-hydroxyvitamin D level in group 3. However, 33 patients in group 3 showed at the sixth month a walking ability beyond pre-fracture ability, and these patients had slightly higher 25-hydroxyvitamin D levels than other patients in group 3 (12.2 ± 11.8 vs. 10.0 ± 7.4; p = 0.055).
Table 3 shows the relationship between walking recovery at the follow-up and the interaction term between variables significantly associated with walking recovery from multiple regression analysis and groups. By analyzing the interaction between tertiles of 25-hydroxyvitamin D and groups, we found a statistically significant interaction term regarding mobility recovery (tertiles of 25-hydroxyvitamin D*groups, β ± SE, 0.04 ± 0.02; p = 0.041). A statistically significant interaction term between 25-hydroxyvitamin D*sex was also found for mobility recovery (β ± SE, 0.14 ± 0.06; p = 0.033). Serum 25-hydroxyvitamin D levels were a little higher in men than in women (12.0 ± 10.6 vs. 10.3 ± 8.0; p = 0.030). Figure 2 shows the raw proportion of patients recovering ambulation at the sixth month by pre-fracture mobility and 25-hydroxyvitamin D tertile.
Discussion
Our results showed that patients with pre-fracture limitations in mobility had a greater rate of mortality during the first year after hip fracture than patients fully independent outdoors. At the same time, among survivors, a full mobility recovery to pre-fracture level is relatively harder to achieve in subjects with higher pre-fracture mobility performance compared with those with mobility limitations. Among the group of patients needing help to walk before fracture, about one third became immobile while the rest, probably because a sort of “floor effect,” re-gained a similar pre-fracture functional status. On the contrary, even at the peak of recovery at the sixth month, only 40 % of mobile patients outdoors regained their mobility and this figure is in line with other studies [18, 19] even if the definitions of walking ability is partially different. Vochteloo [19] found a higher rate of patients who became immobile in the group with a lower pre-fracture mobility, but the high rate of mortality may be a misleading variable in the evaluation of functional outcomes in this group.
A very interesting result of our study concerns the differences among the predictors of late walking after hip fracture among patients with different pre-fracture abilities. In patients with the highest pre-fracture performance (group 1), a number of independent variables seems to affect the probability of walking recovery at the sixth month. Taken together, all these factors are markers of frailty, which is theoretically defined as a clinical state of increased vulnerability, resulting from aging-associated decline in reserve and function and therefore the ability to cope with acute stressors [20]. The catastrophic effect of hip fracture may be particularly relevant in subjects who are still independent but with some decline in their physiological capacities reflected by an impairment in instrumental activities, use of walking devices, older age, comorbidities, or low albumin. On the contrary, in subjects with overt pre-fracture disability, a poor recovery after hip fracture seems related to few variables and mainly to the degree of pre-fracture functional abilities in basic activities. Functional status before fracture is the most potent predictive factor for functional recovery for all groups of patients, regardless of the severity of cognitive impairment [21, 22]. Patients independent outdoors are usually independent in basic activities of daily living but our study showed that even a small impairment in more complex activities such as instrumental ones greatly affected the recovery to pre-fracture levels. Similarly, the probability of recovering walking abilities in patients with pre-fracture impairment is significantly related to the level of pre-fracture basic abilities. On the contrary, cognitive impairment and, in particular, mild to moderate deficiency, was not an independent factor influencing mobility recovery in older persons who had hip fracture after six months. Only severe cognitive impairment may be a negative prognostic factor. However, hip fracture subjects with dementia can regain pre-fracture walking abilities in the same proportion as non-demented people. The effect of cognitive impairment seems to act mainly on pre-fracture functional status. On the other hand, it is well established that cognitively impaired patients gain from rehabilitative treatment [23, 24] and only severe dementia [25] or prolonged post-operative delirium [26] could influence negatively any rehabilitative approach. In our patients delirium was not significantly related to walk recovery at the six month in the multivariate analyses but we recorded only the occurrence of delirium in the peri-operative phase and not its persistence during hospital stay. Most of the significant variables in this study are non-modifiable risk factors and can be used to develop prognostic indices or tailored rehabilitation interventions targeted on a specific risk profile. On the contrary, the concentration of 25-hydroxyvitamin D is a potentially modifiable risk factor through a direct treatment.
In our cohort of patients, the mean levels of 25-hydroxyvitamin D are largely below the optimal status confirming early study on older Italian hip fracture patients [27]. However, patients with 25-hydroxyvitamin D levels higher than 11 ng/ml had a higher probability to recover pre-fracture walking ability. These findings are in accordance with other studies [28] that found 25-hydroxyvitamin D levels at the time of fracture higher than 9 ng/ml were associated with better lower extremity task performance and a reduced likelihood of falling during the year following a hip fracture. Bischoff-Ferrari et al. [29] reported that walking speed and proximal muscle strength were markedly improved when 25-hydroxy25-hydroxyvitamin D levels increased from 4 to 16 ng/ml and continued to improve as the levels increased to more than 40 ng/ml. The simple relationship between pre-fracture 25-hydroxyvitamin D concentration and the odds of walking after fracture do not make it possible to directly presume the effectiveness of vitamin D supplementation which largely remains to be demonstrated. However, on a cohort of subject taken from the same survey, we demonstrated that the highest 25-hydroxyvitamin D levels are closely related to 25-hydroxyvitamin D supplementation [30], therefore our findings indirectly support a positive effect of 25-hydroxyvitamin D optimization on walking recovery after fracture.
Moreover, we found a significant interaction between 25-hydroxyvitamin D and sex for mobility recovery according to other studies that observed an association between 25-hydroxyvitamin D and physical function in women but not in men [31].
The poor rate of full recovery in pre-fracture independent patients finally raises the question of the suitability of the regular programs of rehabilitation. More intensive rehabilitation interventions [32] and extended rehabilitation programs [33] have both been demonstrated to improve long-term outcome in selected patients. However, studies focusing on elderly subjects walking independently before fracture but with some frailty characteristics such as slight impairment in complex activities, using devices, poor nutrition, low 25-hydroxyvitamin D or very old age should be designed to look for the most effective intervention to regain full independence after hip fracture.
This study has limitations. In particular, the design of the study is not a randomized controlled study and other factors that are not included in the analysis could influence our results. Nonetheless, one of the strengths of this study is the fact that the sample includes a large number of unselected patients who are representative of the real-world populations with hip fractures, even if limited to a single country. A second important limitation is the lack of details about rehabilitation intervention administered to each patient. No data are available in this study for defining duration, intensity, and type of physical therapy, all of which are probably important factors in functional recovery.
In conclusion, our data showed that the catastrophic effect of hip fracture in producing mobility disability occurs even in highly independent patients if they have some initial characteristics of frailty. The pre-fracture functional status is the main predictor of walking recovery after hip fracture while cognitive impairment seems to act as an independent factor only in case of severe dementia. 25-hydroxyvitamin D deficiency appears to be an important modifiable component of the global assessment that influences walking recovery, especially in patients with higher pre-fracture performance. If confirmed, our data would suggest that tailored rehabilitative interventions should be an essential part of any plan for maximizing recovery.
References
Ferrucci L, Guralnik JM, Simonsick E, Salive ME, Corti C, Langlois J (1996) Progressive versus catastrophic disability: a longitudinal view of the disablement process. J Gerontol A Biol Sci Med Sci 51(3):M123–30
Hung WW, Egol KA, Zuckerman JD, Siu AL (2012) Hip fracture management: tailoring care for the older patient. JAMA 307(20):2185–94
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, Kenzora J (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55(9):M498–507
Lee D, Jo JY, Jung JS, Kim SJ (2014) Prognostic factors predicting early recovery of pre-fracture functional mobility in elderly patients with hip fracture. Ann Rehabil Med 38(6):827–35
Pioli G, Frondini C, Lauretani F, Davoli ML, Pellicciotti F, Martini E, Zagatti A, Giordano A, Pedriali I, Nardelli A, Zurlo A, Ferrari A, Lunardelli ML (2012) Time to surgery and rehabilitation resources affect outcomes in orthogeriatric units. Arch Gerontol Geriatr 55(2):316–22
Salpakoski A, Törmäkangas T, Edgren J, Sihvonen S, Pekkonen M, Heinonen A, Pesola M, Kallinen M, Rantanen T, Sipilä S (2014) Walking recovery after a hip fracture: a prospective follow-up study among community-dwelling over 60-year old men and women. Biomed Res Int 2014:289549. doi:10.1155/2014/289549
Al-Ani AN, Flodin L, Söderqvist A, Ackermann P, Samnegård E, Dalén N, Sääf M, Cederholm T, Hedström M (2010) Does rehabilitation matter in patients with femoral neck fracture and cognitive impairment? A prospective study of 246 patients. Arch Phys Med Rehabil 91(1):51–7. doi:10.1016/j.apmr.2009.09.005
Muir SW, Yohannes AM (2009) The impact of cognitive impairment on rehabilitation outcomes in elderly patients admitted with a femoral neck fracture: a systematic review. J Geriatr Phys Ther 32(1):24–32
Morandi A, Davis D, Fick DM, Turco R, Boustani M, Lucchi E, Guerini F, Morghen S, Torpilliesi T, Gentile S, MacLullich AM, Trabucchi M, Bellelli G (2014) Delirium superimposed on dementia strongly predicts worse outcomes in older rehabilitation inpatients. J Am Med Dir Assoc 15(5):349–54. doi:10.1016/j.jamda.2013.12.084
Mallinson T, Deutsch A, Bateman J, Tseng HY, Manheim L, Almagor O, Heinemann AW (2014) Comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after hip fracture repair. Arch Phys Med Rehabil 95(2):209–17
Pioli G, Lauretani F, Davoli ML, Martini E, Frondini C, Pellicciotti F, Zagatti A, Giordano A, Pedriali I, Nardelli A, Zurlo A, Ferrari A, Lunardelli ML (2012) Older people with hip fracture and IADL disability require earlier surgery. J Gerontol A Biol Sci Med Sci 67(11):1272–7
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113(12):941–8
Pfeiffer EA (1975) Short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Knaus WA, Draper EA, Wagner DP et al (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Katz S, Ford AB, Moskowitz RW et al (1963) Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Rosell PA, Parker MJ (2003) Functional outcome after hip fracture. A 1-year prospective outcome study of 275 patients. Injury 34(7):529–32
Vochteloo AJ, Moerman S, Tuinebreijer WE, Maier AB, de Vries MR, Bloem RM, Nelissen RG, Pilot P (2013) More than half of hip fracture patients do not regain mobility in the first postoperative year. Geriatr Gerontol Int 13(2):334–41
Xue QL (2011) The frailty syndrome: definition and natural history. Clin Geriatr Med 27(1):1–15
Dubljanin-Raspopovic E, Markovic-Denic L, Matanovic D et al (2012) Is pre-fracture functional status better than cognitive level in predicting short-term outcome of elderly hip fracture patients? Arch Med Sci 8:115e122
Uriz-Otano F, Uriz-Otano JI, Malafarina V (2014) Factors associated with short-term functional recovery in elderly people with a hip fracture. Influence of cognitive impairment. J Am Med Dir Assoc. doi:10.1016/j.jamda.2014.09.009
Rolland Y, Pillard F, Lauwers-Cances V et al (2004) Rehabilitation outcome of elderly patients with hip fracture and cognitive impairment. Disabil Rehabil 26:425e431, Seitz DP
Gill SS, Gruneir A et al (2014) Effects of dementia on postoperative outcomes of older adults with hip fractures: a population-based study. J Am Med Dir Assoc 15:334e341
Morghen S, Gentile S, Ricci E et al (2011) Rehabilitation of older adults with hip fracture: cognitive function and walking abilities. J Am Geriatr Soc 59:1497e1502
Bellelli G, Mazzola P, Morandi A, Bruni A, Carnevali L, Corsi M, Zatti G, Zambon A, Corrao G, Olofsson B, Gustafson Y, Annoni G (2014) Duration of postoperative delirium is an independent predictor of 6-month mortality in older adults after hip fracture. J Am Geriatr Soc 62(7):1335–40
Giusti A, Barone A, Razzano M, Pizzonia M, Oliveri M, Palummeri E, Pioli G (2006) High prevalence of secondary hyperparathyroidism due to hypovitaminosis D in hospitalized elderly with and without hip fracture. J Endocrinol Invest 29(9):809–13
LeBoff MS, Hawkes WG, Glowacki J, Yu-Yahiro J, Hurwitz S, Magaziner J (2008) Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int 19(9):1283–90
Bischoff-Ferrari HA, Dietrich T, Orav EJ, Hu FB, Zhang Y, Karlson EW, Dawson-Hughes B (2004) Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr 80(3):752–8
Lauretani F, Frondini C, Davoli ML, Martini E, Pellicciotti F, Zagatti A, Giordano A, Zurlo A, Pioli G (2012) Vitamin D supplementation is required to normalize serum level of 25OH-vitamin D in older adults: an observational study of 974 hip fracture inpatients. J Endocrinol Invest 35(10):921–4. doi:10.3275/8457
Dam TT, von Mühlen D, Barrett-Connor EL (2009) Sex-specific association of serum vitamin D levels with physical function in older adults. Osteoporos Int 20(5):751–60
Ponten JB, Krug E, van Baardewijk LJ, van der Linden EH, Haas R, Krijnen P, Schipper IB (2015) Intensive rehabilitation in selected hip fracture patients may optimize care efficiency: a retrospective comparison study. J Rehabil Med 47(3):278–81
Auais MA, Eilayyan O, Mayo NE (2012) Extended exercise rehabilitation after hip fracture improves patients’ physical function: a systematic review and meta-analysis. Phys Ther 92(11):1437–51. doi:10.2522/ptj.20110274
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Funding
The study was funded by the Emilia Romagna Region (Region-University Research Program 2007–2009).
Additional information
Authorship
All authors had access to the data and played a role in writing this manuscript.
Rights and permissions
About this article
Cite this article
Pioli, G., Lauretani, F., Pellicciotti, F. et al. Modifiable and non-modifiable risk factors affecting walking recovery after hip fracture. Osteoporos Int 27, 2009–2016 (2016). https://doi.org/10.1007/s00198-016-3485-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3485-y