Abstract
Summary
Serum 25-OH vitamin D levels were compared in 254 hip fracture subjects and 2,402 matched control subjects. There was a significant inverse association between 25-OH vitamin D and hip fracture only between 0 and 70 nmol/L.
Introduction
Vitamin D is integral to bone metabolism, however the utility of serum 25-OH vitamin D as a risk marker for hip fractures is controversial.
Methods
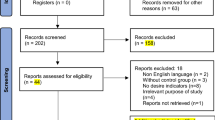
We conducted a case–control study of patients admitted to the hospitals with hip fractures in Calgary, Alberta, (catchment population 1.4 million) between January 1, 2007 and August 31, 2011. We searched the laboratory information system of Calgary Laboratory Services for serum 25-OH vitamin D levels within 6 months prior to admission on patients admitted to hospital with hip fractures. Cases were identified through the Calgary Laboratory Services laboratory information system and were matched to controls for age, sex, and month of testing. The hip fracture–25-OH vitamin D association was examined using multiple linear and spline regression.
Results
Of 305 subjects initially identified with hip fractures, serum 25-OH vitamin D levels were available for 254 (83 %). These were matched to 2,402 control subjects. We observed a significant (p < 0.01) non-linear relationship such that 25-OH vitamin D was inversely associated with hip fracture only below 70 nmol/L (odds ratio = 0.81 per 10 nmol/L increase; 95 % CI 0.86–0.93).
Conclusions
The utility of 25-OH vitamin D level as a risk marker for hip fracture depends on the cut-off level used and was of potential use only for lower levels of 25-OH vitamin D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Considerable clinical interest exists in the potential utility of serum 25-OH vitamin D (25-hydroxyvitamin D) levels as a risk factor for hip and other fractures. As a consequence of this as well as other potential health benefits of adequate 25-OH vitamin D levels, clinical laboratories in North America have seen a marked increase in requests for 25-OH vitamin D testing [1, 2].
Evidence for the utility of 25-OH vitamin D as a risk marker has come from large case series which have consistently reported low levels of 25-OH vitamin D in hip fracture patients [3–8]. Likewise, case–control studies have generally shown lower 25-OH vitamin D levels in hip fracture cases compared to controls [7, 9–15]. However, a recent case–control study of women by Cauley et al. [16] has yielded some contradictory results. In this study, 25-OH vitamin D was inversely associated with hip fracture among whites, but positively associated with hip fracture among African Americans and Asians. No relationship was observed among Hispanics or Native Americans.
The effect of vitamin D supplementation on fracture risk has also been controversial, with a number of clinical trials yielding negative results [17–19]. However, in a recent pooled analysis of seven randomized trials of vitamin D supplementation, the risk of hip and total fractures was lower among individuals taking vitamin D supplements provided that calcium supplements were also taken [20]. This protective effect was present regardless of the subject’s age, sex, or prior fractures.
Thus, while supplement use appears to be beneficial in primary and secondary prevention of fractures, the utility of serum 25-OH vitamin D levels as a risk marker for fracture is uncertain. We performed a case–control study on hip fractures and 25-OH vitamin D status using hospital admission data on hip fractures in a large, mostly urban population (1.4 million people) merged with pre-fracture 25-OH vitamin D data from our hospital laboratory information system. Our objective was to assess the utility of serum 25-OH vitamin D level using both linear and non-linear models as a risk marker for hip fractures. Furthermore, we explored the possibility of a non-linear relationship between 25-OH vitamin D level and hip fracture risk.
Methods
Ethics statement
The study protocol was approved by the University of Calgary Conjoint Health Review Ethics Board (Ethics ID 23919).
Data acquisition
Cases of hip fracture were identified by searching the Alberta Health Services Data Integration, Measurement & Reporting database for the city of Calgary, Alberta, for hospital discharges with the following associated ICD-10 codes: S72.0 (fracture of neck of femur), S72.1 (pertrochanteric fracture), and S72.2 (subtrochanteric fracture). Only discharge records from January 1, 2007 to August 31, 2011 were considered due to the limited availability of 25-OH vitamin D levels from our laboratory information system before January 1, 2007. For each case, we retrieved age, sex, date of admission, and provincial health card number. We included cases due to any cause, including trauma, in order to capture those due to osteoporotic fractures [7, 21].
The provincial health card number was used as a linking variable to search for a pre-fracture serum 25-OH vitamin D measurement in the laboratory information system of Calgary Laboratory Services (CLS). CLS is the sole provider of laboratory testing for the city of Calgary and surrounding areas, and therefore the laboratory information system contains essentially a complete record of laboratory test results for the entire city. In matching 25-OH vitamin D levels to individual patients, we considered only the most recent result prior to hip fracture (to eliminate any effect of trauma on serum 25-hydroxyvitamin D level) [8, 22, 23], with a maximum time interval of 12 months prior to admission. Cases were matched to control subjects from our laboratory information system who were tested during the same period (January 1, 2007–August 31, 2011) without a diagnosis of hip fracture. Initially, this group consisted of approximately 200,000 subjects. As 25-OH vitamin D level is associated with age, sex, and date of testing, we randomly matched cases by age (±90 days), sex, and testing month. We attempted to match 10 controls for each case; however, it was difficult to identify adequate numbers of controls for subjects over 90 years of age, so we relaxed the age matching in this subgroup to ±180 days. All records were de-identified by removing health card number, hospital admission date, and 25-OH vitamin D testing date from the data set.
Statistical analysis
We used Student’s t test to evaluate differences in continuous variables between cases and controls and the chi-squared test for dichotomous variables. Several different 25-OH vitamin D “exposure” levels have been used to evaluate fracture risk: 75 [24], 50 [25, 26], 37.5 [27], and 25 nmol/L [25, 26]. However, because 25-OH vitamin D level is best defined as a continuum [31], we first evaluated the continuous association of 25-OH vitamin D with hip fracture using logistic regression. We then employed a restricted cubic spline function to graphically explore the possibility of a non-linear relationship between varying 25-OH vitamin D levels and log odds of hip fracture. In this analysis, four knots were placed at the quartile midpoints of 25-OH vitamin D and we simultaneously adjusted for sex and age (also modeled as a four-knot cubic spline). We verified non-linear associations identified in the spline analysis using piecewise linear regression and interaction terms (25-OH vitamin D × cut point). Statistical analyses were performed using SPSS v. 19 for Windows, SAS v. 9.3, and R v. 2.25.1 (with rms package).
Results
The hospital discharge database contained 305 hip fracture cases during the study period. A serum 25-OH vitamin D level within 12 months prior to the hip fracture admission date was available for a total of 254 subjects (180 females and 74 males). The mean age of included cases was 78.3 years (range 44.1–99.7 years). For 235 of these subjects (93 %), 10 control subjects were identified. For the remaining 18 cases, between 1 and 9 control subjects were identified. This yielded a total of 2,402 control subjects matched for sex, age, and month of testing (mean of 9.5 controls per case). Baseline characteristics of cases and controls are given in Table 1. Overall, the linear association between 25-OH vitamin D and hip fracture after being adjusted for age, sex, and testing month was not significant (odds ratio per 10 nmol/L increase = 1.01; 95 % CI 0.97–1.04; p = 0.75). However, we observed a statistically significant (p < 0.01) complex non-linear association characterized by changes in the direction of the relationship at 70 and 120 nmol/L when using a cubic spline (Fig. 1, Table 2). We then used piecewise linear regression to verify that the inverse association between 25-OH vitamin D and hip fracture was significant only for 25-OH vitamin D levels below 70 nmol/L. Moreover, when we tested for differences in the piecewise associations below 70 nmol/L, between 70 and 120 nmol/L, and above 120 nmol/L, we saw a significant difference only between associations in the ranges of <70 nmol/L and 70–120 nmol/L (Table 3).
Restricted cubic spline function of the relationship between serum 25-OH vitamin D level and risk of hip fracture. The relationship is adjusted for age (set at a median of 81 years), sex (set as male), and testing month (set at May) and is modeled as a four-knot cubic spline. Log odds is calculated as the natural logarithm of the odds of hip fracture. The shaded area represents the 95 % confidence interval
Discussion
In a case–control study conducted in a major Canadian city and surrounding catchment area, we found an inverse association between pre-fracture 25-OH vitamin D levels and hip fracture only for 25-OH vitamin D levels of less than 70 nmol/L. For individuals in this range, a 10 nmol/L increase in 25-OH vitamin D was associated with 19 % lower odds of fracture.
Numerous randomized controlled trials suggest that vitamin D and calcium supplementation lead to lower fracture risk, but there is ongoing confusion as to the role of serum 25-hydroxyvitamin D as a risk marker. Our findings suggest that at the lower end of the spectrum of observed 25-OH vitamin D levels, there may be a modest role for the use of 25-OH vitamin D as a risk marker, but the presence or absence of a relationship is influenced by the cut-off level used.
Our results combined with other studies suggest that caution should be exercised in the interpretation of serum 25-OH vitamin D levels as a risk marker for hip fracture. In contrast, vitamin D supplementation has been shown to reduce fracture risk in multiple studies. Therefore, a strategy of supplementation without testing may be reasonable in some instances and has the benefit of reducing healthcare expenditures. Calcium and vitamin D supplementation are frequently not prescribed to post-hip fracture patients [28–32], and even when vitamin D supplements are prescribed, there is poor patient compliance [29, 30]. It would appear that this is an area where interest in vitamin D could be usefully applied, especially given the possible additional benefits of vitamin D supplementation [24, 31].
Our study has several strengths. The first is the relatively large sample size and catchment area, which suggests that our estimates are relatively stable and generalizable to a large geographic area. Second, our use of pre-fracture 25-OH vitamin D levels eliminated any possible reverse causality, as hip fracture is known to lower 25-OH vitamin D level. It also avoids capturing subjects who began supplementation following a fracture, which would produce a bias that would make it appear as if higher 25-OH vitamin D level is associated to hip fracture risk.
There are several limitations to this study. First, although our control subjects did not suffer a hip fracture in our jurisdiction within the study period, we did not contact the control subjects to ensure that they did not suffer a hip fracture in another jurisdiction during this time period or in our jurisdiction prior January 1, 2007 or after August 31, 2011. However, the small number of subjects with hip fractures during this period (305) compared to the large number of potential control subjects (200,000) makes it statistically unlikely that a significant number of control subjects would have suffered a hip fracture that did not appear in our hospital discharge database. We also do not know if the cases suffered from a previous fracture. Second, we looked only for an association between 25-OH vitamin D status and hip fracture and did not consider other fractures. This is a question for future study. Finally, an important limitation is that we do not know whether the cases or controls were being supplemented with vitamin D. It is possible that the lack of a significant relationship at higher 25-OH vitamin D levels may have been due in part to individuals with poor bone health (and therefore at higher risk for fractures) being more likely to take vitamin D supplements and therefore exhibiting higher serum 25-hydroxyvitamin D levels. In conclusion, we found that the utility of 25-OH vitamin D level as a risk marker for hip fracture depends on the cut-off level used and was of potential use only for lower serum levels of 25-OH vitamin D.
References
CBC News () http://www.cbc.ca/news/canada/calgary/story/2011/01/28/calgary-vitamin-d-blood-testing.html. Accessed
Singh RJ (2008) Are clinical laboratories prepared for accurate testing of 25-hydroxy vitamin D? Clin Chem 54:221–223
Bischoff-Ferrari HA, Can U, Staehelin HB, Platz A, Henschkowski J, Michel BA, Dawson-Hughes B, Theiler R (2008) Severe vitamin D deficiency in Swiss hip fracture patients. Bone 42:597–602
Simonelli C, Weiss TW, Morancey J, Swanson L, Chen YT (2005) Prevalence of vitamin D inadequacy in a minimal trauma fracture population. Curr Med Res Opin 21:1069–1074
Khadgawat R, Brar KS, Gahlo M, Yadav CS, Malhotra R, Guptat N, Tandon N (2010) High prevalence of vitamin D deficiency in Asian-Indian patients with fragility hip fracture: a pilot study. J Assoc Physicians India 58:539–543
Nurmi I, Kaukonen JP, Lüthje P, Naboulsi H, Tanninen S, Kataja M, Kallio ML, Leppilampi M (2005) Half of the patients with acute hip fracture suffer from hypovitaminosis D: a prospective study in southeastern Finland. Osteoporois Int 16:2018–2024
Cauley JA, Parimi N, Ensrud KE, Bauer DC, Cawthon PM, Cummings SR, Hoffman AR, Shikany JM, Barrett-Connor E, Orwoll E, Osteoporotic Fractures in Men (MrOS) Research Group (2010) Serum 25 hydroxyvitamin D concentrations and the risk of hip and nonspine fractures in older men. J Bone Miner Res 25:545–553
Looker AC, Mussolino ME (2008) Serum 25 hydroxyvitamin D and hip fracture risk in older US white adults. J Bone Miner Res 23:143–150
Bakhtiyarova S, Lesnyak O, Kyznesova N, Blankenstein MA, Lips P (2006) Vitamin D status among patients with hip fracture and elderly control subjects in Yekaterinburg, Russia. Osteoporosis Int 17:441–446
Moniz C, Dew T, Dixon T (2005) Prevalence of vitamin D inadequacy in osteoporotic hip fracture patients in London. Curr Med Res Opin 21:1891–1894
Sakuma M, Endo N, Oinuma T, Hayami T, Endo E, Yazawa T, Watanabe K, Watanabe S (2006) Vitamin D and intact PTH status in patients with hip fracture. Osteoporosis Int 17:1608–1614
Jang WY, Chung MS, Baek GH, Song CH, Cho HE, Gong HS (2012) Vitamin D levels in post-menopausal Korean women with a distal radius fracture. Injury 43:237–241
Weatherall M (2000) A meta-analysis of 25 hydroxyvitamin D in older people with fracture of the proximal femur. N Z Med J 113:137–140
Nuti R, Martini G, Valenti R, Gambera D, Gennari L, Salvadori S, Avanzati A (2004) Vitamin D status and bone turnover in women with acute hip fracture. Clin Orthop Relat Res 422:208–213
Cauley JA, Lacroix AZ, Wu L, Horwitz M, Danielson ME, Bauer DC, Lee JS, Jackson RD, Robbins JA, Wu C, Stanczyk FZ, LeBoff MS, Wactawski-Wende J, Sarto G, Ockene J, Cummings SR (2008) Serum 25 hydroxyvitamin D concentrations and the risk of hip fractures. Ann Intern Med 149:242–250
Cauley JA, Danielson ME, Boudreau R, Barbour KE, Horwitz MJ, Bauer DC, Ensrud KE, Manson JE, Wactawski-Wende J, Shikany JM, Jackson RD (2011) Serum 25-hydroxyvitamin D and clinical fracture risk in a multiethnic cohort of women: the Women’s Health Initiative (WHI). J Bone Miner Res 26:2378–2388
Porthouse J, Cockayne S, King C, Saxon L, Steele E, Aspray T, Baverstock M, Birks Y, Dumville J, Francis R, Iglesias C, Puffer S, Sutcliffe A, Watt I, Torgerson DJ (2005) Randomized controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ 330:1003
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O’Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D, Investigators W’s H I (2006) Calcium plus vitamin D supplementation and the risks of fractures. N Engl J Med 354:669–683
Grant AM, Avenell A, Campbell MK, McDonald AM, MacLennan GS, McPherson GC, Anderson FH, Cooper C, Francis RM, Donaldson C, Gillespie WJ, Robinson CM, Torgerson DJ, Wallace WA, RECORD Trial Group (2005) Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomized placebo-controlled trial. Lancet 365:1621–2628
DIPART (Vitamin D Individual Patient Analysis of Randomized Trials) Group (2010) Patient level pooled analysis of 68,500 patients from seven major vitamin D fracture trials in US and Europe. BMJ 340:b5463
Sanders KM, Pasco JA, Ugoni AM, Nicholson GC, Seeman E, Martin TJ, Skoric B, Panahi S, Kotowicz MA (1998) The exclusion of high trauma fractures may underestimate the prevalence of bone fragility fractures in the community: the Geelong Osteoporosis Study. J Bone Miner Res 13:1337–1342
Lips P, Bouillon R, Jongen MJ, van Ginkel FC, van der Vijgh WJ, Netelenbos JC (1985) The effect of trauma on serum concentrations of vitamin D metabolites in patients with hip fracture. Bone 6:63–67
Mak JCS, Stuart-Harris J, Cameron ID, Mason RS (2010) Oral vitamin D replacement after hip fracture: a comparative review. J Am Geriatr Soc 58:382–417
Lüthje P, Nurmi-Lüthje I, Kaukonen JP, Kuurne S, Naboulsi H, Kataja M (2009) Undertreatment of osteoporosis following hip fracture in the elderly. Arch Gerontol Geriatr 49:153–157
Byszewski AM, Cranney A, Man-Son-Hing M, Azad N, Amos S (2006) Evaluation of in-hospital management of fracture risk in older patients: a chart review study of tertiary prevention. Arch Gerontol Geriatr 42:319–328
Carnevale V, Nieddu L, Romagnoli E, Bona E, Piemonte S, Scillitani A, Minisola S (2006) Osteoporosis intervention in ambulatory patients with previous hip fracture: a multicentric, nationwide Italian study. Osteoporosis Int 17:478–483
Jennings LA, Auerbach AD, Maselli J, Pekow PS, Lindenauer PK, Lee SJ (2010) Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc 58:650–657
Harrington JT, Broy SB, Derosa AM, Licata AA, Shewmon DA (2002) Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum 47:651–654
Giusti A, Barone A, Razzano M, Oliveri M, Pizzonia M, Palummeri E, Pioli G (2009) Persistence with calcium and vitamin D in elderly patients after hip fracture. J Bone Miner Metab 27:95–100
Segal E, Zinman C, Raz B, Ish-Shalom S (2009) Low patient compliance—a major negative factor in elderly hip fracture patients supplemented with 800 IU of vitamin D3 daily. Arch Gerontol Geriatr 49:364–367
Hanley DA, Cranney A, Jones G, Whiting SJ, Leslie WD, Cole DE, Atkinson SA, Josse RG, Feldman S, Kline GA, Rosen C, Guidelines Committee of the Scientific Advisory Council of Osteoporosis Canada (2010) Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada. CMAJ 182:E610–E618
Rosen CJ, Adams JS, Bikle DD, Black DM, Demay MB, Manson JE, Murad MH, Kovacs CS (2012) The nonskeletal effects of vitamin D: an Endocrine Society scientific statement. Endocr Rev 33:456–492
Acknowledgments
CN was supported by research grants from the University of Calgary and Calgary Laboratory Services. We thank Megan Joy-Rockey for her assistance in this project.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Koning, L., Henne, D., Hemmelgarn, B.R. et al. Non-linear relationship between serum 25-hydroxyvitamin D concentration and subsequent hip fracture. Osteoporos Int 24, 2061–2065 (2013). https://doi.org/10.1007/s00198-012-2249-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2249-6