Abstract
All hip fracture (HF) subjects are candidates for calcium and vitamin D (CaD) supplementation. Up to 50% of HF older adults present with secondary hyperparathyroidism (HPTH) resulting from hypovitaminosis D on hospital admission. To investigate the patterns and predictors of persistence with CaD supplementation in the elderly after HF, we considered all patients aged 70 years or older who were discharged alive after surgical repair of HF in the period of 1 year from an Orthopaedic Unit. Baseline characteristics of the subjects and osteoporosis treatment prescribed at discharge were retrieved from medical record review. A telephone interview at 6 months evaluated whether patients were currently taking CaD supplementation. Nonpersistence was defined when subjects ceased therapy within 6 months. Univariate and multivariate models were applied to determine the relationship between 6 months persistence with CaD and the variables collected: age, living situation, prescription of a bisphosphonate, baseline walking ability, number of drugs used, presence of dementia, number of active clinical issues at discharge (ACIs), discharge location, and being referred to a center for metabolic bone diseases (preplanned visit) at discharge. Of 428 subjects enrolled, 117 were excluded for different reasons (incomplete data, no therapy, death). A total of 311 subjects were discharged with a prescription of CaD (calcium 1,000 mg, cholecalciferol 800 UI, once daily) and were considered for the analysis. At 6 months, only 114 patients (36.7%) were currently taking CaD supplementation. In a univariate analysis, the following variables were significantly related with persistence: absence of dementia, prescription of a bisphosphonate, six or fewer drugs being used (drugs used ≤6), two or less ACIs (≤2 ACIs) at discharge, ability to walk without aid at baseline, being discharged home, and being referred to a preplanned visit. In a multivariate model, the prescription of a bisphosphonate at discharge (OR 3.178, 95% CI 1.477–6.836, P = 0.003), a preplanned visit (OR 1.953, 95% CI 1.066–3.514, P = 0.03), the absence of dementia (OR 1.877, 95% CI 1.021–3.451, P = 0.043), and ≤6 drugs used (OR 1.842, 95% CI 1.066–3.182, P = 0.029) remained the most significant predictors of persistence with CaD. In HF elderly, who are at high risk of hypovitaminosis D and HPTH, persistence with CaD supplementation is very low. The enrolment in a postsurgical program for the management of bone disease can significantly increase persistence. Moreover, factors related to the complexity of older adult patients (polypharmacotherapy, dementia) seem to be particularly important in compliance with prescribed drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture (HF) accounts for about 10% of all osteoporosis-related fractures [1]. About 6–10% of HF patients sustain a second HF within 4 years from the first [2, 3]. Incidence of a second HF tends to rise during the 8 months following the first HF, peaking at 8 months and then tapering off [3]. Johnell et al. [4] demonstrated that a prior HF is a significant risk factor not only for subsequent HF but even for spine and forearm fracture. Therefore, patients with severe osteoporosis who sustain HFs are candidates for osteoporosis therapy.
Vitamin D deficiency and secondary hyperparathyroidism (HPTH) are frequently present in the elderly, especially in patients with HF [5]. It has been recently reported that approximately 50% of HF patients acutely admitted to an orthopaedic unit presented with HPTH secondary to hypovitaminosis D at the time of hospital admission [6]. Vitamin D deficiency and secondary HPTH lead to an increase of bone turnover, which is usually associated with bone loss, primarily cortical [5]. Thus, secondary HPTH has been proposed as the principal mechanism whereby hypovitaminosis D could contribute to the pathogenesis of HF [5, 6] Consequently, calcium and vitamin D (CaD) are regarded as an essential first-line strategy in the management of osteoporosis, particularly in HF subjects, either alone or in combination with other therapies [7].
After prescription of an osteoporosis treatment, adequate persistence is required to reduce fracture risk [8, 9]. Adami et al. [10] demonstrated that in patients not taking, or with poor compliance to, CaD supplements there was an increased risk of inadequate clinical response to osteoporosis drug therapy, defined as the occurrence of a new fragility fracture while on treatment. A number of studies in the past few years examined risk factors for poor persistence with osteoporosis medications, mainly focusing on dosing regimens, cost of medication, and drug-related side effect [8]. Moreover, only one study evaluated factors that significantly influence the discontinuation of treatment after HF, including comorbidity as a potential cause of nonpersistence [11]. There is, however, an increasing awareness that nonpersistence with a prescribed therapy in the elderly may be related to more complex and “comprehensive” aspects than in younger adults [12]. The problem largely arises because there are a number of factors (e.g., polypharmacotherapy, disability in activities of daily living, dementia) that characterize the frail older adult and which may influence the compliance to prescribed drugs.
The present study investigated factors related to the complexity of older adults potentially associated with nonpersistence with CaD supplementation in a cohort of 428 HF elderly enrolled in a postsurgical follow-up program after hospital discharge.
Methods
We considered all women aged 70 years and older, consecutively discharged with a prescription of calcium and cholecalciferol (CaD3), from one Acute Orthopaedic Ward within the same hospital in the period of 1 year (2004), after surgical repair of a nontraumatic HF. Patients with a major trauma, or metastatic or Paget disease of the bone, and already receiving an antiosteoporotic treatment or CaD supplements at the time of hospital admission were excluded.
Baseline prefracture and in-hospital characteristics of the subjects were retrieved from medical record review. The surgeon was responsible for the treatments prescribed at discharge (including the antiosteoporotic drugs) and for the choice of referring the women to a center for metabolic bone diseases at discharge.
The present investigation was performed using baseline and follow-up data from a project originally designed to evaluate functional recovery and 6-month survival in older adults after HF. Thus, as a part of the follow-up program, all patients received at 6 months a telephone interview to assess survival status, functional recovery, and the type of antiosteoporotic drugs used. Nonpersistence was defined as the condition of a patient who ceased following the prescribed therapy with CaD3 within 6 months from discharge [13]. The following variables from medical records were tested in an univariate analysis as potentially associated with persistence with CaD3: age, living situation (living alone, living with relatives), living in institution (yes or no), discharge destination (home, institution), premorbid (2 weeks before hospital admission) walking ability (walks without aid, walks with aid), number of drugs other than those for osteoporosis prescribed at discharge, prescription of a bisphosphonate associated with CaD3 supplementation at discharge, presence of cognitive impairment (defined as a Short Portable Mental Status Questionnaire score <8), number of active clinical issues (ACIs) at discharge and being referred to a center for metabolic bone disease at discharge (preplanned visit, yes or no) [14, 15]. All the independent variables, except for age, were expressed as dichotomic, with the categories selected on the basis of their clinical significance or distribution (median).
The dependent variable was the continuation of the CaD3 therapy, expressed as a binary value, at 6 months. We first analyzed bivariate association between the outcome and each of the independent variables by nonparametric Kruskal–Wallis test. Then, all the covariates significantly associated with persistence were retained for a logistic regression analysis.
All comparisons were two-tailed, and significance was set at P < 0.05. Odds ratios (ORs), 95% confidence intervals (CIs), and P values were calculated using standard formulae. Statistical analysis was performed using SPSS for Windows.
The hospital’s ethics committee reviewed and approved the study protocol. When the subjects were too confused to understand the informed consent process, proxy consent was obtained.
Results
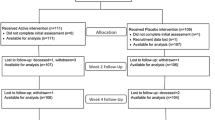
Of the 428 subjects initially considered for the study, 8 subjects (1.9%) were discharged without a prescription of calcium and cholecalciferol and were therefore excluded from the study. Of the remaining 420 patients, 109 had incomplete data (20 subjects) or died within 6 months (89 subjects) and were consequently excluded from the analysis. Overall, 311 patients who were prescribed CaD3 supplementation (calcium 1,000 mg + cholecalciferol 800 UI in a single combined daily dose) at discharge, alone or in combination with a bisphosphonate (46 patients, 14.8%), were included in the final analysis.
Mean age (±SD) was 83.7 ± 6.8 years (range, 68–100). Only 35 women (11.3%) were living in an institution at the time of fracture; of the noninstitutionalized patients (276), 95 lived alone and the others with relatives. The mean number (±SD) of drugs other than those for osteoporosis prescribed was 6.8 ± 2.0 (range, 2–16; median, 7), and at discharge, the patients presented a mean (±SD) of 2.2 ± 1.4 ACIs (range, 0–6; median, 2).
After 6 months, only 114 patients (36.7%) were currently taking CaD3 supplementation. As shown in Table 1, in a univariate analysis several variables were significantly related with persistence: absence of cognitive impairment (P < 0.001), number of drugs used ≤6 (P = 0.013), prescription of a bisphosphonate at discharge (P < 0.001), ACIs ≤ 2 at discharge (P = 0.005), premorbid ability to walk without aid (P < 0.001), being discharged home (P = 0.003), and being referred to a preplanned visit (P < 0.001). Age was at the limit of significance (P = 0.076), whereas institutionalization and living situation (cohabitation or living alone) were not significant. In a multivariate logistic regression analysis (Table 2), including all significant variables of univariate analysis and age, the prescription of a bisphosphonate at discharge (OR 3.178, 95% CI 1.477–6.836, P = 0.003), a preplanned visit (OR 1.953, 95% CI 1.066–3.514, P = 0.03), the absence of cognitive impairment (OR 1.877, 95% CI 1.021–3.451, P = 0.043) and drugs used ≤6 (OR 1.842, 95% CI 1.066–3.182, P = 0.029) remained the most significant predictors of persistence with CaD3.
Discussion
In this study, we examined patterns and factors, poorly evaluated in previously published reports on this topic (such as walking ability, polypharmacotherapy, cognitive impairment, and being referred to a center for metabolic bone diseases), potentially associated with persistence with calcium and cholecalciferol supplementation in a cohort of elderly women, discharged alive after surgical repair of a nontraumatic HF [11–13]. The issue appears relevant, taking into account that combined CaD supplementation is an essential component in the management of osteoporosis, particularly in subjects with HF who frequently (up to 50%) present secondary HPTH and hypovitaminosis D at the time of hospital admission [6, 7]. Moreover, compliance with CaD has a key role in optimizing clinical efficacy of antiresorpive agents, as it has been recently demonstrated that poor compliance to CaD supplementation or persistence of secondary HPTH over the period of treatment may increase the risk of inadequate clinical response to a bisphosphonate [10, 16].
In the present nonintervention observational study, more than 95% of the subjects were discharged with CaD3 supplementation, while only 15% received a bisphosphonate associated with CaD3 (Table 1). The number of subjects treated with some antiosteoporotic drugs was much higher compared to previous reports, even though only a very small proportion of women received a bisphosphonate [8, 9]. As expected, at 6 months more than one-half of the patients had ceased the antiosteoporotic treatment prescribed at discharge. Such a proportion of nonpersistence is similar to that found in the general population and in another study carried out in HF patients [8, 9, 17].
The univariate analysis demonstrated that medical, functional, and sociodemographic characteristics (premorbid walking ability, cognitive function, polypharmacotherapy, discharge location, and ACIs) usually linked with the frailty phenotype are important variables related to persistence with CaD3 [18, 19]; age, living situation, and premorbid institutionalization demonstrated no relationship.
Indeed, in a multivariate analysis a small number of drugs used at discharge and the absence of cognitive impairment remained, together with the prescription of a bisphosphonate and a preplanned visit, the most significant predictors of persistence with CaD3 supplementation. A large number of drugs used as well as cognitive decline are considered comprehensive parameters of functional status, of somatic and cognitive comorbidity, that in general are coexisting conditions in frail older adults and are associated with negative outcomes [18, 19]. The relationship between these parameters and persistence with CaD3 may indirectly indicate that those subjects with “a lower degree of frailty” (absence of dementia, using fewer drugs) are the most compliant to a prescribed drug.
Interestingly, the prescription of a more active agent (bisphosphonate) in association with CaD3 resulted in a higher rate of persistence with CaD3. This finding is quite surprising and, to our knowledge, it has never being described before. One reason of such correlation may reside in the fact that CaD are perceived more as a simple supplementation rather than as a true treatment. Thus, the prescription of an agent that is regarded as a more effective and powerful therapy in the management of osteoporosis and secondary prevention of fractures may improve persistence with CaD3 by increasing motivation of the patients. In this case, a limitation largely arises from the study, because we did not consider underlying motivation and psychological features potentially related to persistence that could give more insight into the interaction between the different factors considered.
One of the most relevant findings of our data is the fact that subjects referred to a center for metabolic bone diseases at discharge showed an higher rate of persistence with CaD3, demonstrating, in the multivariate model, about a twofold increased probability of continuing prescribed therapy. In this context, a similar result found in a smaller sample by Segal et al. [17] showed an increased adherence to CaD supplementation in elderly HF patients enrolled in a specially designed postsurgical follow-up program. A possible explanation of this association is suggested by Carnevale and colleagues, who found a twofold risk of stopping antiosteoporosis medications in patients who had not undergone a diagnostic test for osteoporosis, emphasizing the role of motivation and disease awareness [11]. This results highlight the importance of referring patients who sustain a fragility fracture to centers skilled in the management of metabolic bone diseases to improve persistence with antiosteoporotic drugs. However, given the observational nature of our study, a further “ad hoc designed” randomized controlled intervention trial is needed to evaluate the cost-effectiveness and support with a higher level of evidence the role of close follow-up monitoring visit in improving compliance with prescribed drugs and reducing subsequent fracture risk in elderly after HF.
Our study has two important strengths. First, we investigated the effects of some characteristics linked to the complexity of older adults and with the frailty phenotype (cognitive function, walking ability, and polypharmacotherapy) on persistence with CaD supplementation. These factors frequently characterize older adults. Thus, our study by considering this variables has faced an extremely important aspect of pharmacological management in elderly subjects. Furthermore, the study focused on the persistence with calcium and cholecalciferol supplementation, independently of the use of a bisphosphonate. Actually, several studies have highlighted the importance of CaD supplementation during antiresorptive treatment, for the management of osteoporosis and reduction of fracture risk in the elderly, particularly in HF subjects, given the high prevalence of hypovitaminosis D in this vulnerable population [6, 7, 10].
There are several potentials limitations of the study as well. First of all, as just pointed out, we did not consider the effect of underlying motivation and psychological features that could give more insight into the interaction between the different factors considered. In addition, the particular type of patients considered (hip fractured) limit inferring our results to the general population. Finally, as compared to other reports carried out in the general population, our sample was relatively small and follow-up time quite limited.
In conclusion, our work demonstrates that, at least in the elderly population, other factors than those usually considered, but related to the complexity of older adults, influence compliance to a prescribed drug.
References
Eastell R, Reid DM, Compston J, Cooper C, Fogelman I, Francis RM, Hay SM, Hosking DJ, Purdie DW, Ralston SH, Reeve J, Russell RG, Stevenson JC (2001) Secondary prevention of osteoporosis: when should a non-vertebral fracture be a trigger for action? Q J Med 94:575–597
Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR (2003) Incidence and risk factors for a second hip fracture in elderly women. The Study of Osteoporotic Fractures. Osteoporos Int 14:130–136
Yamanashi A, Yamazaki K, Kanamori M, Mochizuki K, Okamoto S, Koide Y, Kin K, Nagano A (2005) Assessment of risk factors for second hip fracture in Japanese elderly. Osteoporos Int 16:1239–1246
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
Giusti A, Barone A, Razzano M, Pizzonia M, Oliveri M, Palummeri E, Pioli G (2006) High prevalence of secondary hyperparathyroidism due to hypovitaminosis D in hospitalized elderly with and without hip fracture. J Endocrinol Invest 29:809–813
Boonen S, Vanderschueren D, Haentjens P, Lips P (2006) Calcium and vitamin D in the prevention and treatment of osteoporosis: a clinical update. J Intern Med 259:539–552
Cramer JA, Gold DT, Silverman SL, Lewiecki EM (2007) A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int 18:1023–1031
Seeman E, Compston J, Adachi J, Brandi ML, Cooper C, Dawson-Hughes B, Jönsson B, Pols H, Cramer JA (2007) Non-compliance: the Achilles’ heel of anti-fracture efficacy. Osteoporos Int 18:711–719
Adami S, Isaia G, Luisetto G, Minisola S, Sinigaglia L, Gentilella R, Agnusdei D, Iori N, Nuti R, ICARO Study Group (2006) Fracture incidence and characterization in patients on osteoporosis treatment: the ICARO study. J Bone Miner Res 21:1565–1570
Carnevale V, Nieddu L, Romagnoli E, Bona E, Piemonte S, Scillitani A, Minisola S (2006) Osteoporosis intervention in ambulatory patients with previous hip fracture: a multicentric, nationwide Italian survey. Osteoporos Int 17:478–483
Kruse WH (1995) Comprehensive geriatric assessment and medication compliance. Z Gerontol Geriatr 28:54–61
Lekkerkerker F, Kanis JA, Alsayed N, Bouvenot G, Burlet N et al (2007) Adherence to treatment of osteoporosis: a need for study. Osteoporos Int 18:1311–1317
Pfeiffer E (1975) A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Halm EA, Magaziner J, Hannan EL, Wang JJ, Silberzweig SB, Boockvar K, Orosz GM, McLaughlin MA, Koval KJ, Siu AL (2003) Frequency and impact of active clinical issues and new impairments on hospital discharge in patients with hip fracture. Arch Intern Med 163:107–112
Barone A, Giusti A, Pioli G, Girasole G, Razzano M, Pizzonia M, Palummeri E, Bianchi G (2007) Secondary hyperparathyroidism due to hypovitaminosis D affects bone mineral density response to alendronate in elderly women with osteoporosis: a randomized controlled trial. J Am Geriatr Soc 55:752–757
Segal E, Zinnman H, Raz B, Tamir A, Ish-Shalom S (2004) Adherence to vitamin D supplementation in elderly patients after hip fracture. J Am Geriatr Soc 52:474–475
Volpato S, Onder G, Cavalieri M, Guerra G, Sioulis F, Maraldi C, Zuliani G, Fellin R, Italian Group of Pharmacoepidemiology in the Elderly Study (GIFA) (2007) Characteristics of nondisabled older patients developing new disability associated with medical illnesses and hospitalization. J Gen Intern Med 22:668–674
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56:M146–MI56
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Giusti, A., Barone, A., Razzano, M. et al. Persistence with calcium and vitamin D in elderly patients after hip fracture. J Bone Miner Metab 27, 95–100 (2009). https://doi.org/10.1007/s00774-008-0007-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-008-0007-9