Abstract
The lateral closing and medial opening wedge high tibial osteotomy can correct a varus malalignment of the knee caused by medial compartment osteoarthritis. These procedures have produced great short-term and mid-term results. As no systematic review has examined their long-term results yet, the goal of this article was to compare the results of all articles about lateral closing and medial opening wedge high tibial osteotomies, published after the year 2000, with a mean follow-up of more than 10 years. A systematic search of the Medline, Web of Science and Cochrane databases resulted in the inclusion of 30 articles. All these studies combined examined the results of 7087 high tibial osteotomies in a total of 6636 patients after a mean follow-up of more than 10 years. Primary outcome measures were the survival rate of the osteotomy, functional scores, patient satisfaction and pain scores. Secondary outcome measures were alignment correction and the identification of factors influencing the survival of the osteotomy. The 5-year, 10-year, 15-year and 20-year survival rates, respectively, ranged from 86 to 100%, 64–97.6%, 44–93.2% and 46–85.1%. The subjective scoring systems showed an improvement postoperatively that was maintained until final follow-up. The anatomical and mechanical tibiofemoral axis were, respectively, corrected to a mean of 7.3°–13.8° of valgus and 0.6°–4° of valgus. The results of the articles evaluating the influence of potential risk factors were contradictory. Despite the low quality of the available evidence, the lateral closing and medial opening wedge high tibial osteotomy seem to remain valid long-term treatment options for patients with painful varus malalignment caused by isolated medial compartment osteoarthritis of the knee. The available results indicate that the need for arthroplasty could be delayed for more than 15 years in the majority of patients. However, higher-quality studies are needed to confirm these findings. As a systematic review is assigned a level of evidence equivalent to the lowest level of evidence used from the analyzed manuscripts, the level of evidence of this systematic review is IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis most commonly affects the medial compartment, as the load on this compartment in healthy knees is about 2.5 times greater than on the lateral side [3, 33]. This can lead to the gradual development of a varus malalignment and a subsequent shift of the weightbearing line to pass more medially through the tibial plateau. A further increase of the load on the medial compartment and decrease of the load on the lateral compartment ensues [44].
Specific surgical options exist for medial compartment osteoarthritis of the knee, amongst which high tibial osteotomy and unicompartmental knee arthroplasty. The two most popular osteotomy techniques are the lateral closing wedge and medial opening wedge high tibial osteotomy [11, 13]. The purpose of these procedures is to redirect the weightbearing axis to a neutral or slightly more lateral position, aiming to interrupt and potentially reverse the pathological changes in the medial compartment [28]. Short- and mid-term results obtained with high tibial osteotomies are good to excellent, but the results gradually deteriorate over time [7, 12, 14, 34]. The excellent results of the unicompartmental knee arthroplasty resulted in a decline in the use of high tibial osteotomies [8, 57]. However, current developments like tissue engineering and meniscal transplants might revive the interest in the latter as the alignment of the knee will influence their results [31, 56].
The question remains whether there continues to be a place for isolated high tibial osteotomies as treatment for varus knees secondary to medial compartment osteoarthritis and whether the long-term results can justify their use. Many studies refer to the long-term results of a select number of publications. However, no prior study has systematically collected all the available long-term results.
Hence, the goal of this study is to systematically look at the published long-term results of the lateral closing and medial opening wedge technique. Less frequently performed techniques (e.g., the dome osteotomy) will not be discussed.
The hypothesis of this systematic review is that an isolated high tibial osteotomy remains a valid alternative for a unicompartmental knee arthroplasty, with good long-term outcomes in carefully selected patients suffering from medial compartment osteoarthritis of the knee.
Materials and methods
Search strategy
A systematic search of the Medline, Web of Science and Cochrane databases was conducted. The aim was to identify all the articles published between January 1, 2000 and February 20, 2020 presenting the long-term results of lateral closing and/or medial opening wedge high tibial osteotomies. The cut-off was arbitrarily set at the year 2000 to avoid potential skewing of the results by studies of osteotomies performed with early, less standardized techniques using less stable fixation material.
The Medline database was searched using the terms ‘high tibial osteotomy’, ‘varus gonarthrosis’ and ‘long term results’, which yielded 69 articles.
The Web of Science database was searched using ‘high tibial osteotomy osteoarthritis long term results’ as search criterium. With this method, 250 articles were identified.
The search strategy for the Cochrane database for systematic reviews was ‘high tibial osteotomy’, which yielded 3 reviews. The detailed search strategy can be found in Fig. 1. The articles initially identified with these three search methods were subsequently screened for inclusion in this systematic review in the following order: publication date, language, title, abstract and full text using the inclusion and exclusion criteria listed in Table 1.
Data collection
Two of the authors independently used the above strategy to screen the obtained articles for eligibility. A third author was consulted in case of disagreement. Thirty articles were eventually included, as can be seen in Fig. 1. All of them have a level of evidence of III or IV. Five articles present results of the medial opening wedge technique [21, 22, 24, 41, 43]. Nineteen articles report solely on the lateral closing wedge technique [1, 6, 9, 16, 18,19,20, 25, 26, 29, 30, 32, 36, 38, 39, 46, 48, 50, 51]. Six articles share the results of the medial opening and lateral closing wedge technique by either comparing or combining the outcomes [4, 15, 35, 40, 42, 52].
All these studies combined present the results of 7087 high tibial osteotomies performed between 1970 and 2012 in a total of 6636 patients.
Primary outcome measures were the survival rate of the osteotomy, functional scores (e.g., the Oxford Knee Score, the Hospital for Special Surgery score, the Knee Society Score, etc.), patient satisfaction and pain scores. Secondary outcome measures were the alignment correction and identification of factors influencing the survival.
Risk of bias
Every included study was subjected to a risk of bias analysis, which was done independently by two of the authors. A third author was consulted in case of disagreement. As none of the included studies were randomized and most lacked a control group, the ROBINS-I tool for uncontrolled before–after studies was chosen as evaluation method [49]. The results are presented in Table 2.
Results
Primary outcome measures
-
1.
Survival
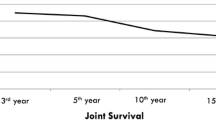
The survival rate was generally defined as the percentage of high tibial osteotomies that had not been converted to arthroplasty in function of time. Three articles broadened the definition of failure by adding re-osteotomy to it [19, 26, 41]. Akizuki et al. also labeled an HSS score of less than 70 as failure [1]. Polat et al. considered survival as the survival of the native joint, with radiological destruction without conversion to arthroplasty also being noted as failure [40].
Twenty-two articles reported a Kaplan–Meier survival analysis [1, 6, 15, 16, 18,19,20, 22, 25, 26, 29, 30, 35, 38, 41,42,43, 46, 48, 50,51,52]. The survival in the eight articles without a Kaplan–Meier analysis was calculated by dividing the number of high tibial osteotomies not converted to arthroplasty at final follow-up by the number of osteotomies included in the study [4, 9, 21, 24, 32, 36, 39, 40].
The 5-year, 10-year and 15-year survival rate in the studies, respectively, ranged from 86 to 100%, 64 to 97.6% and 44 to 93.2%. Only five studies reported a 20-year survival rate, ranging from 46 to 85.1% [6, 15, 19, 46, 48]. Table 3 lists the survival rates obtained with the lateral closing and medial opening wedge technique. The 15-year results were better in the lateral closing wedge group, but data for this length of follow-up were only available in two studies on the medial opening wedge technique.
The survival rates of the studies with and those without Kaplan–Meier survival analysis are presented in Tables 4, 5, respectively. These tables also contain information about the age of the patients at the time of surgery, ranging from 15 to 84 years.
Comparing the survival rate of subgroups was not possible given the large variety of characteristics between the articles, as illustrated by Tables 6, 7.
-
2.
Functional scores, patient satisfaction and pain scores
Several studies presented functional scores and/or information on patient satisfaction and pain levels preoperatively and at final follow-up. Many different functional scores were used in the articles, which made it difficult to compare the obtained results. However, all these scoring systems showed higher results, maintained until final follow-up, compared to preoperatively. Nine articles added a significance level to the change in functional scores and the improvement was significant in all of them [6, 9, 18, 21, 29, 32, 36, 39, 43].
Twelve articles, representing a total of 1456 patients, separately mentioned the effect of the procedure on the satisfaction level [6, 9, 18, 19, 25, 26, 29, 38, 39, 41, 42, 48]. According to these studies, between 77 and 98% of patients were (very) satisfied after a mean follow-up of more than 10 years. Hui et al. showed that 68% of the subgroup who had to undergo a revision to arthroplasty was still satisfied [26]. The mean onset for dissatisfaction was 10.7 years in the study by Huang et al. and 14.2 years in the study by Flecher et al. [19, 25].
Four articles, representing a total of 308 patients, described a sustained improvement of the patient’s pain level at final follow-up, compared to preoperatively [6, 20, 38, 39].
Secondary outcome measures
-
1.
Alignment correction
The terms ‘femorotibial alignment’ and ‘anatomical tibiofemoral axis’ refer to the angle between the anatomical axis of the shaft of the femur and the tibia, which is approximately 5°–7° of valgus in healthy knees [37].
The terms ‘mechanical tibiofemoral axis’ and ‘hip–knee angle’ refer to the angle between the mechanical axis of the femur and the tibia, which is approximately 1° (± 3°) of varus in healthy knees [10].
In the studies using the mean femorotibial alignment or anatomical tibiofemoral axis, this angle ranged from 0.1° valgus to 9.6° varus preoperatively and was corrected to a mean of 7.3°–13.8° valgus postoperatively [1, 9, 18, 19, 25, 26, 29, 30, 32, 36, 39, 42, 46, 52]. The goal of most of these studies was to correct the alignment to a valgus angle of 8°–10° [9, 18, 25, 26, 29, 39].
In the studies using the mean mechanical tibiofemoral axis or hip–knee angle, this angle ranged from 5.8° to 18° varus preoperatively and was corrected to a mean of 0.6°–4° valgus postoperatively [4, 6, 15, 16, 20, 21, 24, 41, 43, 46, 51]. The aim of most of these studies was to correct the alignment to a valgus angle of 3°–6° [4, 22, 24, 41, 51].
Eight articles expressed the desired degree of overcorrection in a different way [1, 19, 21, 30, 32, 36, 40, 46]. The purpose in four of those articles was to redirect the alignment axis through the middle of the lateral tibial plateau [1, 30, 32, 36]. The other four articles wanted the alignment axis to pass through Fujisawa point, located at 62% of the tibial plateau width when measured from the medial side [19, 21, 40, 46].
-
2.
Factors influencing survival
The 21 articles that evaluated the impact of potential risk factors on the survival rate of high tibial osteotomies provided contradictory results. Table 8 presents the findings from the articles investigating commonly addressed risk factors [1, 6, 9, 16, 19, 20, 24,25,26, 29, 30, 35, 36, 38, 39, 41, 43, 48, 50,51,52]. In the studies that identified an influence of these risk factors, older age, female gender, higher BMI, higher preoperative degrees of osteoarthritis, larger preoperative varus angles and undercorrection of the alignment resulted in worse outcomes.
Table 9 shows the results from the seven articles that analyzed some other potential risk factors [1, 6, 9, 16, 26, 39, 43]. In the studies that found an impact of these additional risk factors, a lesser preoperative knee function, a history of knee surgery and a postoperative increase of osteoarthritis in the lateral knee compartment resulted in a worse outcome, whereas the absence of an anterior cruciate ligament led to better results.
Discussion
The most important findings of this systematic review were the good to excellent long-term survival rates and patient-reported outcomes obtained with the lateral closing and medial opening wedge high tibial osteotomy. The contribution of the Finnish registry-based study by Niinimäki et al. is noteworthy given its large sample size (3195 knees) and its study design that included patients from both state-funded and private hospitals [35]. They obtained a 5-year and 10-year survival rate of, respectively, 89% and 73%. Most other articles portrayed better results. A possible explanation for this difference could be the introduction of a bias in the other studies by only presenting results from very experienced professionals. Niinimäki et al. conducted their study to establish such a discrepancy [35]. A prior Swedish population-based study corroborates this statement by showing a 10-year survival rate of 70%, which is similar to the Finnish study [53].
Three included studies (reporting on the lateral closing wedge technique) had remarkably better results than the other ones after 5, 10 and 15 years and the difference became more noticeable with increasing length of follow-up [1, 19, 29]. These articles demonstrated the possibility to maintain excellent results for longer than 15 years. However, these results should be interpreted with caution given the low quality of the studies included in this systematic review.
It remains unclear whether the lateral closing wedge and medial opening wedge technique are equivalent alternatives [2, 45]. Wang et al. conducted a meta-analysis of nine studies with short- to medium-term follow-up to answer this question, but they could not conclude which technique is superior [54]. In this systematic review, the results of the lateral closing wedge technique were slightly better than those of the medial opening wedge technique after 10 years. The results after 15 years of follow-up were also better in this group. However, drawing a definite conclusion remains difficult as information for this length of follow-up was only available in two articles on the medial opening wedge technique, presenting the results of 259 osteotomies.
The sole use of the survival rate to assess the outcome of high tibial osteotomies has been criticized in the past as the absence of conversion to arthroplasty does not necessarily equal a good result [15, 41]. Patients can be hesitant to undergo another operation, regardless of the persistence or recurrence of pain and doctors may be less inclined to perform an arthroplasty in younger patients [15, 35, 51]. However, several authors argued that this remains the most objective and valid outcome measure as delaying the need for arthroplasty is the main goal of performing a high tibial osteotomy [19, 51]. Functional scores and questionnaires about patient satisfaction and pain level changes are more subjective evaluation methods. In their review, Webb et al. concluded that good functional scores can be obtained with high tibial osteotomies after short- to medium-term follow-up [55]. This review evaluated the change in functional scores after a mean follow-up of more than 10 years. The studies that presented functional scores showed a considerable improvement postoperatively in most patients, which was maintained until final follow-up. Given that the natural course of osteoarthritis would result in a progressive deterioration of the joint quality and, therefore, also of the functional scores, one could assume that a high tibial osteotomy has a positive and long-lasting impact on the functional outcome [17].
The optimal correction angle has been a point of discussion since high tibial osteotomies were initially introduced. The general consensus is that an overcorrection to valgus alignment produces the best results, but the exact amount of correction remains debatable. An insufficient correction can result in the gradual recurrence of varus alignment [12, 23]. In the past, some authors insisted on performing large overcorrections [27, 48]. Others advised against it as it is cosmetically unpleasing and can lead to a faster progression of osteoarthritis in the lateral compartment [12, 23]. Therefore, surgeons, nowadays, mostly aim for a moderate overcorrection of the anatomical tibiofemoral axis to 8–10° of valgus or of the mechanical tibiofemoral axis to 3–6° of valgus, as was the case in most of the included studies.
In this systematic review, the difference in survival of the osteotomy between the studies became more pronounced with increasing length of follow-up. This could indicate an influence from certain factors that differed between the articles. Identifying these risk factors might make it possible to refine the indications for high tibial osteotomies and achieve even higher survival rates. Many authors already investigated the influence of age, BMI, gender, osteoarthritis grade, preoperative and postoperative alignment extensively in the past [5, 12, 27, 34, 47]. Their results were often contradictory, as was the case in this systematic review. One of the possible explanations for this discord might be the lack of extremes in certain studies. Huang et al. could not identify the preoperative grade of osteoarthritis as risk factor, but they only included patients with mild changes [25]. The same goes for the studies by Van Raaij et al. and Flecher et al. with respect to the effect of the preoperative alignment [19, 51].
Age at the time of surgery may only have had an influence in certain studies because surgeons were less inclined to perform a conversion to arthroplasty in younger patients [35, 51].
A strength of this systematic review is the large sample size through the inclusion of thirty articles, presenting results from 7087 high tibial osteotomies in a total of 6636 patients after a mean follow-up of more than 10 years. Another strength is the availability of results after more than 15 years of follow-up in nineteen studies, examining the results of a total of 2700 patients.
This is the first study that systematically presents the long-term results of high tibial osteotomies in that many patients after a mean follow-up of more than 10 years.
The main limitation of this systematic review is the low quality of the included articles. Almost all are retrospective studies without a control group and the follow-up rate is low in some articles. Another weakness is the pronounced lack of uniformity between the included studies and their contradictory results regarding the influence of potential risk factors. These major limitations somewhat impede drawing definite conclusions about the position of high tibial osteotomies in current practice and emphasize the need for prospective studies of higher quality in the future. However, the results of this systematic review are encouraging and suggest that the lateral closing and medial opening wedge high tibial osteotomy remain valid treatment options for patients with isolated medial compartment osteoarthritis of the knee.
Conclusion
Despite the low quality of the available evidence, the lateral closing and medial opening wedge high tibial osteotomy seem to remain valid long-term treatment options for patients with painful varus malalignment caused by isolated medial compartment osteoarthritis of the knee. This is demonstrated by the good to excellent long-term survival rates and functional scores obtained in this systematic review. The ideal candidate appears to be a non-obese male who is less than 65 (and preferably even less than 50) years old, with a low grade of medial osteoarthritis and a limited preoperative varus angle. However, good results still seem to be achievable in patients with some potential risk factors for failure [24, 26, 36, 43]. The results of this systematic review indicate that the need for arthroplasty could be delayed for more than 15 years in the majority of patients, but higher-quality studies are needed to confirm these findings.
References
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Jt Surg Br 90:592–596
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34:155–160
Andriacchi TP (1994) Dynamics of knee malalignment. Orthop Clin North Am 25:395–403
Benzakour T, Hefti A, Lemseffer M, El Ahmadi JD, Bouyarmane H, Benzakour A (2010) High tibial osteotomy for medial osteoarthritis of the knee: 15 years follow-up. Int Orthop 34:209–215
Berman AT, Bosacco SJ, Kirshner S, Avolio A Jr (1991) Factors influencing long-term results in high tibial osteotomy. Clin Orthop Relat Res 272:192–198
Berruto M, Maione A, Tradati D, Ferrua P, Uboldi FM, Usellini E (2020) Closing-wedge high tibial osteotomy, a reliable procedure for osteoarthritic varus knee. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-05890-0
Bode G, von Heyden J, Pestka J, Schmal H, Salzmann G, Sudkamp N et al (2015) Prospective 5-year survival rate data following open-wedge valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 23:1949–1955
Bruni D, Iacono F, Akkawi I, Gagliardi M, Zaffagnini S, Marcacci M (2013) Unicompartmental knee replacement: a historical overview. Joints 1:45–47
Choi HR, Hasegawa Y, Kondo S, Shimizu T, Ida K, Iwata H (2001) High tibial osteotomy for varus gonarthrosis: a 10- to 24-year follow-up study. J Orthop Sci 6:493–497
Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P (1997) Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthr Cartil 5:39–47
Coventry MB (1965) Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. a preliminary report. J Bone Jt Surg Am 47:984–990
Coventry MB, Ilstrup DM, Wallrichs SL (1993) Proximal tibial osteotomy. a critical long-term study of eighty-seven cases. J Bone Jt Surg Am 75:196–201
Debeyre J, Patte D (1962) Value of corrective osteotomies in the treatment of certain knee diseases with axial deviation. Rev Rhum Mal Osteoartic 29:722–729
Duivenvoorden T, Brouwer RW, Baan A, Bos PK, Reijman M, Bierma-Zeinstra SM et al (2014) Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up. J Bone Jt Surg Am 96:1425–1432
Duivenvoorden T, van Diggele P, Reijman M, Bos PK, van Egmond J, Bierma-Zeinstra SMA et al (2017) Adverse events and survival after closing- and opening-wedge high tibial osteotomy: a comparative study of 412 patients. Knee Surg Sports Traumatol Arthrosc 25:895–901
Efe T, Ahmed G, Heyse TJ, Boudriot U, Timmesfeld N, Fuchs-Winkelmann S et al (2011) Closing-wedge high tibial osteotomy: survival and risk factor analysis at long-term follow up. BMC Musculoskelet Disord 12:46
Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman BN, Aliabadi P et al (1995) The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 38:1500–1505
Flamme CH, Ruhmann O, Schmolke S, Wichmann R (2003) Long-term outcome following high tibial osteotomy with tension bend principle. Arch Orthop Trauma Surg 123:12–16
Flecher X, Parratte S, Aubaniac JM, Argenson JN (2006) A 12–28-year followup study of closing wedge high tibial osteotomy. Clin Orthop Relat Res 452:91–96
Gstottner M, Pedross F, Liebensteiner M, Bach C (2008) Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 128:111–115
Hantes ME, Natsaridis P, Koutalos AA, Ono Y, Doxariotis N, Malizos KN (2018) Satisfactory functional and radiological outcomes can be expected in young patients under 45 years old after open wedge high tibial osteotomy in a long-term follow-up. Knee Surg Sports Traumatol Arthrosc 26:3199–3205
Hernigou P, Ma W (2001) Open wedge tibial osteotomy with acrylic bone cement as bone substitute. Knee 8:103–110
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. a ten to thirteen-year follow-up study. J Bone Jt Surg Am 69:332–354
Hernigou P, Roussignol X, Flouzat-Lachaniette CH, Filippini P, Guissou I, Poignard A (2010) Opening wedge tibial osteotomy for large varus deformity with Ceraver resorbable beta tricalcium phosphate wedges. Int Orthop 34:191–199
Huang TL, Tseng KF, Chen WM, Lin RM, Wu JJ, Chen TH (2005) Preoperative tibiofemoral angle predicts survival of proximal tibia osteotomy. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000149818.70975.07188-195
Hui C, Salmon LJ, Kok A, Williams HA, Hockers N, van der Tempel WM et al (2011) Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med 39:64–70
Insall JN, Joseph DM, Msika C (1984) High tibial osteotomy for varus gonarthrosis. A long-term follow-up study. J Bone Jt Surg Am 66:1040–1048
Koshino T, Wada S, Ara Y, Saito T (2003) Regeneration of degenerated articular cartilage after high tibial valgus osteotomy for medial compartmental osteoarthritis of the knee. Knee 10:229–236
Koshino T, Yoshida T, Ara Y, Saito I, Saito T (2004) Fifteen to twenty-eight years’ follow-up results of high tibial valgus osteotomy for osteoarthritic knee. Knee 11:439–444
Kuwashima U, Okazaki K, Iwasaki K, Akasaki Y, Kawamura H, Mizu-Uchi H et al (2019) Patient reported outcomes after high tibial osteotomy show comparable results at different ages in the mid-term to long-term follow-up. J Orthop Sci 24:855–860
Liu JN, Agarwalla A, Gomoll AH (2019) High tibial osteotomy and medial meniscus transplant. Clin Sports Med 38:401–416
Majima T, Yasuda K, Katsuragi R, Kaneda K (2000) Progression of joint arthrosis 10 to 15 years after high tibial osteotomy. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200012000-00021177-184
Morrison JB (1970) The mechanics of the knee joint in relation to normal walking. J Biomech 3:51–61
Naudie D, Bourne RB, Rorabeck CH, Bourne TJ (1999) The install award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 367:18–27
Niinimaki TT, Eskelinen A, Mann BS, Junnila M, Ohtonen P, Leppilahti J (2012) Survivorship of high tibial osteotomy in the treatment of osteoarthritis of the knee: finnish registry-based study of 3195 knees. J Bone Jt Surg Br 94:1517–1521
Omori G, Koga Y, Miyao M, Takemae T, Sato T, Yamagiwa H (2008) High tibial osteotomy using two threaded pins and figure-of-eight wiring fixation for medial knee osteoarthritis: 14 to 24 years follow-up results. J Orthop Sci 13:39–45
Oswald MH, Jakob RP, Schneider E, Hoogewoud HM (1993) Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty 8:419–426
Papachristou G, Plessas S, Sourlas J, Levidiotis C, Chronopoulos E, Papachristou C (2006) Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int Orthop 30:403–408
Pfahler M, Lutz C, Anetzberger H, Maier M, Hausdorf J, Pellengahr C et al (2003) Long-term results of high tibial osteotomy for medial osteoarthritis of the knee. Acta Chir Belg 103:603–606
Polat G, Balci HI, Cakmak MF, Demirel M, Sen C, Asik M (2017) Long-term results and comparison of the three different high tibial osteotomy and fixation techniques in medial compartment arthrosis. J Orthop Surg Res 12:44
Saragaglia D, Blaysat M, Inman D, Mercier N (2011) Outcome of opening wedge high tibial osteotomy augmented with a Biosorb(R) wedge and fixed with a plate and screws in 124 patients with a mean of ten years follow-up. Int Orthop 35:1151–1156
Schallberger A, Jacobi M, Wahl P, Maestretti G, Jakob RP (2011) High tibial valgus osteotomy in unicompartmental medial osteoarthritis of the knee: a retrospective follow-up study over 13–21 years. Knee Surg Sports Traumatol Arthrosc 19:122–127
Schuster P, Gesslein M, Schlumberger M, Mayer P, Mayr R, Oremek D et al (2018) Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med 46:1362–1370
Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N et al (2010) Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis 69:1940–1945
Smith TO, Sexton D, Mitchell P, Hing CB (2011) Opening- or closing-wedged high tibial osteotomy: a meta-analysis of clinical and radiological outcomes. Knee 18:361–368
Song SJ, Bae DK, Kim KI, Park CH (2019) Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surg Sports Traumatol Arthrosc 27:1310–1319
Spahn G, Kirschbaum S, Kahl E (2006) Factors that influence high tibial osteotomy results in patients with medial gonarthritis: a score to predict the results. Osteoarthr Cartil 14:190–195
Sprenger TR, Doerzbacher JF (2003) Tibial osteotomy for the treatment of varus gonarthrosis. Survival and failure analysis to twenty-two years. J Bone Jt Surg Am 85:469–474
Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919
Trieb K, Grohs J, Hanslik-Schnabel B, Stulnig T, Panotopoulos J, Wanivenhaus A (2006) Age predicts outcome of high-tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 14:149–152
van Raaij T, Reijman M, Brouwer RW, Jakma TS, Verhaar JN (2008) Survival of closing-wedge high tibial osteotomy: good outcome in men with low-grade osteoarthritis after 10–16 years. Acta Orthop 79:230–234
van Wulfften Palthe AFY, Clement ND, Temmerman OPP, Burger BJ (2018) Survival and functional outcome of high tibial osteotomy for medial knee osteoarthritis: a 10–20-year cohort study. Eur J Orthop Surg Traumatol 28:1381–1389
W-Dahl A, Robertsson O, Lohmander LS (2012) High tibial osteotomy in Sweden, 1998–2007: a population-based study of the use and rate of revision to knee arthroplasty. Acta Orthop 83:244–248
Wang Z, Zeng Y, She W, Luo X, Cai L (2018) Is opening-wedge high tibial osteotomy superior to closing-wedge high tibial osteotomy in treatment of unicompartmental osteoarthritis? A meta-analysis of randomized controlled trials. Int J Surg 60:153–163
Webb M, Dewan V, Elson D (2018) Functional results following high tibial osteotomy: a review of the literature. Eur J Orthop Surg Traumatol 28:555–563
Wong KL, Lee KB, Tai BC, Law P, Lee EH, Hui JH (2013) Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years’ follow-up. Arthroscopy 29:2020–2028
Wright J, Heck D, Hawker G, Dittus R, Freund D, Joyce D et al (1995) Rates of tibial osteotomies in Canada and the United States. Clin Orthop Relat Res 319:266–275
Acknowledgements
None
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
The contribution of each author meets the requirements for authorship as defined by the ICMJE guidelines.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ollivier, B., Berger, P., Depuydt, C. et al. Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surg Sports Traumatol Arthrosc 29, 3569–3584 (2021). https://doi.org/10.1007/s00167-020-06262-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06262-4