Abstract
Purpose
To determine survivorship and functional outcomes of fixed and mobile-bearing designs in lateral unicompartmental knee arthroplasties (UKA).
Methods
Medline, EMBASE and Cochrane databases were searched. Annual revision rate and functional outcomes were assessed for both fixed and mobile-bearing designs.
Results
A total of 28 studies, of which 19 fixed-bearing and 9 mobile-bearing, representing 2265 lateral UKAs were included for survivorship and functional outcome analyses. The mean follow-up of fixed and mobile-bearing studies was 7.5 and 3.9 years, respectively. Annual revision rate of fixed-bearing designs was 0.94 (95% CI 0.66–1.33) compared to 2.16 (95% CI 1.54–3.04) for mobile-bearing. A subgroup analysis of the domed shaped mobile-bearing design noted an annual revision rate of 1.81 (95% CI 0.98–3.34). Good-to-excellent functional outcomes were observed following fixed and mobile-bearing lateral UKAs; no significant differences were found.
Conclusion
Mobile-bearing lateral UKAs have a higher rate of revision compared to fixed-bearing lateral UKAs with regard to short- to mid-term survivorship; however, the clinical outcomes are similar. Despite the introduction of the domed shaped mobile-bearing design, findings of this study suggest fixed-bearing implant design is preferable in the setting of isolated lateral osteoarthritis (OA). This systematic review was based on low to moderate evidence, therefore, future registry data are needed to confirm these findings. However, this study included a large number of patients, and could provide information regarding risk of revision and functional outcomes of mobile and fixed-bearing type lateral UKA.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) comprises 8–10% of all knee arthroplasties according to national registries [1,2,3,4]. Registries and cohort studies demonstrated lower survivorship of UKA compared to total knee arthroplasty (TKA) [5]. However, studies showed several advantages of UKA over TKA; lower infection and mortality rates, faster recovery, larger range of motion (ROM) and better patient-reported outcome measures (PROMs) [6,7,8,9]. Due to these advantages, as well as improvements in implant design and surgical techniques, and a better understanding of patient indications, UKA is gaining popularity [2,3,4]. The majority of all UKA procedures (85–95%) concern the medial compartment, while the surgical volume of the lateral UKA is limited [2, 4, 10]. Lateral UKA is performed less frequently as it is considered a more technically demanding surgical procedure and the prevalence of isolated lateral Osteoarthritis (OA) is lower compared to medial OA [11, 12].
The lateral tibiofemoral compartment has different anatomy and kinematics compared to the medial compartment, resulting in a greater anteroposterior translation during knee flexion. Furthermore, increased laxity in flexion is noted laterally [13,14,15]. Therefore, it has been suggested that implant design affects outcomes of lateral UKA to a greater extent than it may in medial UKA [16]. Currently, there are two bearing types available for UKA, mobile and fixed-bearing designs. Mobile-bearing designs have the theoretical advantage in restoring the biomechanics of the lateral compartment by allowing anteroposterior translation of the insert, which results in lower contact stresses on the polyethylene [14, 17]. However, due to the increased laxity, bearing dislocation has been reported frequently following lateral UKA surgery with mobile-bearing implants [16]. Therefore, in the setting of lateral UKA, the choice of bearing design remains controversial.
To our knowledge, limited evidence is available comparing outcomes of fixed and mobile-bearing lateral UKAs. Therefore, the primary aim of this study was to systematically assess survivorship of fixed and mobile-bearing lateral UKAs. Secondary, functional outcomes of both implant designs were evaluated. The hypothesis of this study was that fixed-bearing designs would show higher survivorship compared to mobile-bearing designs. Furthermore, it was expected that better functional outcomes would be reported following mobile-bearing lateral UKA.
Materials and methods
Search strategy
This systematic review was conducted according to PRISMA guidelines [18]. A comprehensive search was performed in Medline, EMBASE and Cochrane Library on February 12, 2018. Search terms included “unicompartmental”, “knee”, “arthroplasty” and the associated synonyms (“Appendix”). Additionally, common medical abbreviations and “lateral” were added. No limits on publication date or patient age were used. Search strategies are shown in “Appendix”. After removing duplicates, title and abstract of the studies were screened by two authors independently (JAB and LJK), considering the eligibility criteria (Table 1). References of included studies were checked for any missing studies. The third author (INS) was consulted in case of disagreement. Consensus was achieved with regard to inclusion or exclusion for all reviewed articles.
Data extraction
Data was extracted and collected in Microsoft Excel 2017 by one of the authors (JAB), and subsequently, checked for accuracy by another author (INS). The data from the included studies was divided into two groups based on bearing type: (1) fixed-bearing and (2) mobile-bearing lateral UKA. The first author, study design (retro- or prospective), study characteristics (publication year, country, time of inclusion, number of patients and knees), patient characteristics (age, sex, body mass index; BMI), arthroplasty (implant design, surgical approach, indication), implant survival data (revision, failure mode, follow-up) and functional outcomes (e.g., ROM, PROMs) were extracted. Authors were contacted for additional information when indication of the lateral UKA were unspecified. Results reported as medians were transformed to means by the method of Hozo et al. [19].
Implant survival data was transformed into annual revision rate to correct for different follow-up intervals between populations. This metric is defined as revision rate per observed component-year [5, 6]. Revision was defined as ‘a new operation in a previously resurfaced knee during which one or more of the components are exchanged, removed, or added’ according to the Swedish arthroplasty registry [4]. Therefore, additional medial UKA and patellofemoral arthroplasty for OA progression were both considered as a revision. Moreover, re-operations that were not clearly described were considered a revision.
Methodological quality assessment
Methodological quality assessment was performed independently by two authors (JAB and LJK) using the validated MINORS criteria (methodological index for non-randomized studies) [20]. The third author (INS) was consulted in case of disagreement.
Statistical analysis
Poisson-normal models with random effects were used to estimate pooled annual revision rate data separately for fixed and mobile-bearing lateral UKA cohorts. The log incidence rates of each cohort enabled the calculation of overall log incidence rates per bearing type. Pooled annual revision rates with 95% confidence intervals (CI) were obtained by back-transforming the log incidence rates. Analyses were conducted using R version 3.2.3 (R Foundation for Statistical Computing, Vienna, Austria) with Metafor version 1.9-8 (Maastricht University, Maastricht, Netherlands). In addition, a subgroup analysis was performed to determine the annual revision rate for the Oxford domed mobile-bearing design (Biomet UK ltd, Swindon, UK).
Primary lateral OA was the main indication in the majority of studies (> 75% of the cohort), however, in a proportion of the studies this information was lacking. A sensitivity analysis was conducted, as secondary OA could influence the result as it is associated with inferior outcomes [21, 22].
For pre- and postoperative functional outcomes, means and standard deviations (SD) for each bearing type were combined and reported as mean difference with 95% CI. These pooled analyses were performed with RevMan version 5.3 (Cochrane Reviews, London, UK) using the inverse variance method. If outcomes were reported with a range, the SD was calculated using the method by Walter and Yao [23]. A p value < 0.05 was considered to be statistically significant.
The heterogeneity between studies were determined by the χ2 and I2 statistic method in both the annual revision rate and functional outcome analyses. Heterogeneity was considered with a I2 value of 25% to be low; 50%, moderate; and 75%, high [5].
Results
A total of 28 studies were included, representing 2265 lateral UKAs (Fig. 1) in 19 fixed-bearing and nine mobile-bearing studies [11, 16, 17, 22, 24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. Seventy-eight percent of the mobile-bearing studies used the Oxford domed design, while a variety of fixed-bearing implants were used. Nineteen (70%) studies used a lateral parapatellar approach, and eight (30%) used another approach (e.g., medial parapatellar, traditional TKA) or included multiple approaches over the course of the study. There was female predominance (range 52–93%). Mean age ranged from 53 to 74 years and mean BMI from 25 to 33 kg/m2 (Table 2).
Quality of the studies
Twenty (71%) retrospective and eight (29%) prospective studies were included. The mean MINORS score of the comparative studies was 16.1 (range 13–18), and 9.4 (range 7–12) for the non-comparative studies, representing 67% and 59% of the maximum score, respectively (Table 2). None of the studies were blinded and only three (11%) reported prospective calculation of the sample size.
Annual revision rates
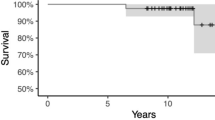
The overall annual revision rate of the fixed-bearing group was 0.94 (95% CI 0.66–1.33) and 2.16 (95% CI 1.54–3.04) for the mobile-bearing group (Table 3; Figs. 2, 3). A subgroup analysis was performed for the domed mobile-bearing design; showing an overall annual revision rate of 1.81 (Table 3; Fig. 4). Annual revision rates of each study were converted to survival rates and plotted (Fig. 5). Overall, heterogeneity was low among the fixed-bearing studies and moderate for mobile-bearing studies (Table 3). The sensitivity analysis for studies with unspecified indications for lateral UKA showed no differences in survival compared to studies that did specify their indication. The distribution of modes of failure is shown in Table 4. A total of seven fixed-bearing and five mobile-bearing studies specified the type of revisions performed [17, 24,25,26, 29, 31, 32, 35, 37, 38, 41, 42, 46]. It was noted that fixed-bearing lateral UKAs were more frequently converted to TKA (67.4% of mobile-bearing versus 41.9% of mobile-bearing), while tibial bearing or insert exchange was more commonly reported after mobile-bearing lateral UKA (29% of mobile-bearing versus 0% of fixed-bearing).
Functional outcomes
A total of 11 studies reported pre- and postoperative PROMs and 13 studies reported ROM [11, 16, 17, 24, 26,27,28,29, 32, 35, 37, 38, 40, 42, 43, 45]. Overall, no statistically significant differences were found in KSS (Knee Society Score) knee, KSS function, KSS total, OKS (Oxford Knee Scores), nor in ROM between the two designs. Overall, heterogeneity was high among the fixed-bearing studies and high to low for mobile-bearing studies (Table 5).
Discussion
The main finding of this study was that the risk of revision is lower after lateral UKA with fixed-bearing designs than mobile-bearing designs. The annual revision rate of the mobile-bearing was 2.16, domed mobile-bearing 1.81 and fixed-bearing designs 0.94, corresponding to extrapolated 5-year survival rates of 89%, 91% and 95%, respectively. This dissimilarity between the two bearing types could be a consequence of a higher proportion of dislocations after mobile-bearing lateral UKAs (44%) compared to fixed-bearing lateral UKAs, although the new domed mobile-bearing design reduces the number of bearing dislocations. Progression of OA in the medial compartment was observed as mode of failure in both fixed-bearing and mobile-bearing designs (53% and 19%, respectively). Furthermore, good-to-excellent PROMs and ROM were noted with both bearing types, which did not support our hypothesis favoring the use of mobile-bearing designs based on functional outcome. This study highlights the importance of assessing survivorship and functional outcomes in lateral UKAs per bearing type using a systematic approach, due to the low prevalence of this procedure.
Currently, studies comparing fixed and mobile-bearing lateral UKA survivorship are limited. One large registry-based study by Baker et al., including 2052 lateral UKAs, found no statistical difference in survival between fixed and mobile-bearing designs [10]. Contrary to our definition for revision, the authors did not differentiate between individual components for each prosthesis, which could lead to smaller differences in survival rates between the two bearing types. Therefore, it is important to bear in mind that the definition of revision could influence study results. Our extrapolated 5-year survival rate of domed mobile-bearing was higher when compared to a recent Danish registry, which included 52 domed mobile-bearing implants (91% versus 87.4%, respectively) [48]. To our knowledge, no other registry or systematic review has assessed lateral UKA survivorship per bearing type. In summary, this overview stresses the need for studies and registries to assess survivorship of lateral UKAs per bearing type, as data are very limited.
Regarding modes of failure, bearing dislocation was frequently noted in mobile-bearing designs (44%), whereas progression of OA in the medial compartment was common in both fixed and mobile-bearing designs (53% and 19%, respectively). Most of the included studies failed to report the time of revision with corresponding mode of failure. Therefore, in this study, modes of failure per bearing type could not be corrected by follow-up period. This may explain the higher percentage of progression of medial OA in the fixed-bearing group, as their average follow-up is longer and progression of OA often occurs later after the initial surgery. The high percentage of bearing dislocations in mobile-bearing lateral UKAs may be due to larger joint distraction in flexion laterally compared to medially (7 mm versus 2 mm) [15]. To lower the rates of bearing dislocation, the domed mobile-bearing tibial implant has been introduced. This implant potentially reduces the incidence, as it requires more distraction before the polyethylene insert dislocates, however, it does not eliminate the possibility of bearing dislocation [13, 16]. Overall, the available literature implicates that the benefit of using fixed-bearing designs is that bearing dislocation cannot occur.
When reviewing mobile-bearing results, surprisingly no dislocations were observed in two studies. Liebs et al. used a mobile-bearing of which the insert slides into a groove from anterior to posterior, while medial–lateral translation is restrained. Consequently, dislocation did not occur; however, aseptic loosening was frequently noted, and therefore, this implant is no longer used [30, 33, 49]. The study by Van Duren et al. used a trans-patellar approach to optimize the access for the vertical cut of the tibia [28]. This approach allows the surgeon to place the tibial component and bearing in a potentially more optimal position. No dislocations of the domed mobile-bearing were reported at a relatively short median follow-up of 27.4 months. Several studies suggested that component alignment is critical to reduce the risk of dislocation in mobile-bearing designs [50, 51]. Gulati et al. recommended after radiographic evaluation of knees with dislocated bearings that overstuffing should be avoided and the femoral component needs to be neutrally aligned in flexion.
Several mobile-bearing studies have managed bearing dislocation successfully by replacing the bearing with a thicker one. In addition, the revision method by Weston-Simons et al. was used, in which the bearing was exchanged and two to three screws were inserted with their heads above the medial wall of the tibial plateau to prevent recurrent dislocation [17]. According to the Australian registry, these types of revision are classified as a minor revision, but have a higher risk of re-revision compared to revision to TKA [2, 52]. Therefore, UKA surgeons need to carefully consider if bearing exchange is a useful option when revising a UKA on the lateral side for bearing dislocation.
To prevent progression of OA in the medial compartment following mobile and fixed-bearing lateral UKAs, it is generally stated that overcorrection should be avoided [24, 35, 38, 43]. Ohdera et al. suggested a valgus aligned mechanical axis between 5°–7° should be aimed in lateral UKA surgery [38]. Furthermore, Van der List et al. showed that postoperative valgus of 3°–7° was correlated with better functional outcomes than more neutral aligned knees [53]. However, a cautious approach is needed since MUKA studies reported that undercorrection is associated with polyethylene wear [54, 55]. Based on the results of this study and those reported by Baker et al., polyethylene wear was less frequently reported as a mode of failure after lateral UKA [10]. Future studies are necessary to evaluate the association between degree of valgus and polyethylene wear following lateral UKAs.
In the present study, no statistically significant differences were found in functional outcomes between both bearing types. Mobile-bearing UKAs may have theoretical biomechanical advantages; however, this did not affect the functional outcomes after surgery. Only two small comparative studies assessed functional outcomes, and similarly, showed no statistically significant differences in OKS and ROM between both designs [30, 36].
This study has several limitations. Although the metric annual revision rate corrects for different follow-up intervals between studies, it relies on the assumption that the revision rate remains constant over time. Therefore, mobile-bearing findings have to be interpreted with more caution than those for fixed-bearing, because annual revision rate of mobile-bearing were only based on short- to mid-term results. Furthermore, despite the majority of studies having > 70% patients with primary OA and having performed a sensitivity analysis based on indication, considerable variability of the indication for each procedure existed. Another limitation is that a majority of the studies consisted of small cohorts with low to moderate quality. In addition, several cohort studies in the domed mobile-bearing group have led to concerns about the reliability due to developer bias, therefore, assessing survivorship and functional outcomes with registry data may be helpful. However, only one annual registry reported survivorship of the domed mobile-bearing design and one registry-based study reported results of both bearing types separately. Hence, this study provides insights to the current literature.
Conclusion
In conclusion, mobile-bearing lateral UKA have a higher rate of revision compared to fixed-bearing lateral UKA with regard to short- to mid-term survivorship; however, the clinical outcomes are similar. Despite the improvements in mobile-bearing implants with a domed shaped design, short- to mid-term survivorship remains inferior to the fixed-bearing designs due to a high percentage of bearing dislocations leading to revision. Other common failure modes in both the fixed and mobile-bearing designs were progression of OA. As a result of the moderate evidence included in this study, future registry data are needed to confirm these findings. Nonetheless, the results of this study suggest a preference of using fixed-bearing implants for isolated lateral knee OA.
Abbreviations
- UKA:
-
Unicompartmental knee arthroplasty
- ROM:
-
Range of motion
- PROMs:
-
Patient-reported outcome measures
- BMI:
-
Body mass index
- OA:
-
Osteoarthritis
- TKA:
-
Total knee arthroplasty
- MINORS:
-
Methodological index for non-randomized studies
- CI:
-
Confidence interval
- SD:
-
Standard deviations
- KSS:
-
Knee Society Score
- OKS:
-
Oxford Knee Scores
References
American Joint Registry (2017) Executive summary of 2017 annual report. Arthroplasty Today 3:315
Australian Joint Registry (2017) Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2017. https://aoanjrr.sahmri.com. Accessed 16 May 2018
British Joint Registry (2017) National Joint Registry for England, Wales and Northern Ireland 14th Annual Report 2017. http://www.njrcentre.org.uk/njrcentre/default.aspx. Accessed 16 May 2018
Swedish Joint Registry (2017) Swedish Knee Arthroplasty Register Annual Report 2017. http://www.myknee.se/en/. Accessed 16 May 2018
Chawla H, van der List JP, Christ AB et al (2017) Annual revision rates of partial versus total knee arthroplasty: a comparative meta-analysis. Knee 24(2):179–190
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2017) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(6):1811–1822
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384(9952):1437–1445
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14 076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B(6):793–801
Lombardi AV, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467(6):1450–1457
Baker PN, Jameson SS, Deehan DJ et al (2012) Mid-term equivalent survival of medial and lateral unicondylar knee replacement: An analysis of data from a National Joint Registry. Bone Joint J 94-B(12):1641–1648
Demange MK, Von Keudell A, Probst C, Yoshioka H, Gomoll AH (2015) Patient-specific implants for lateral unicompartmental knee arthroplasty. Int Orthop 39(8):1519–1526
Wise BL, Niu J, Yang M et al (2012) Patterns of compartment involvement in tibiofemoral osteoarthritis in men and women and in whites and African Americans. Arthritis Care Res 64(6):847–852
Baré JVV, Gill HSS, Beard DJJ, Murray DWW (2006) A convex lateral tibial plateau for knee replacement. Knee 13(2):122–126
Hill PF, Vedi V, Williams A et al (2000) Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg 82(8):1196–1198
Tokuhara Y, Kadoya Y, Nakagawa S, Kobayashi A, Takaoka K (2004) The flexion gap in normal knees. J Bone Joint Surg 86(8):1133–1136
Pandit H, Jenkins C, Beard DJ et al (2010) Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee 17(6):392–397
Weston-Simons JS, Pandit H, Kendrick BJL et al (2014) The mid-term outcomes of the Oxford Domed Lateral unicompartmental knee replacement. Bone Joint J 96 B(1):59–64
Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma group (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6(7):e1000097
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13
Slim K, Nini E, Forestier D et al (2003) Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716
El-Galaly A, Haldrup S, Pedersen AB et al (2017) Increased risk of early and medium-term revision after post-fracture total knee arthroplasty: results from the Danish Knee Arthroplasty Register. Acta Orthop 88(3):263–268
Sah AP, Scott RD (2007) Lateral unicompartmental knee arthroplasty through a medial approach: study with an average five-year follow-up. J Bone Joint Surg Am 89(9):1948–1954
Walter SD, Yao X (2007) Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol 60(8):849–852
Argenson JNA, Parratte S, Bertani A, Flecher X, Aubaniac JM (2008) Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res 466(11):2686–2693
Ashraf T, Newman JH, Evans RL, Ackroyd CE (2002) Lateral unicompartmental knee replacement: survivorship and clinical experience over 21 years. J Bone Joint Surg 84(8):1126–1130
Berend KR, Kolczun MC, George JW, Lombardi AV (2012) Lateral unicompartmental knee arthroplasty through a lateral parapatellar approach has high early survivorship. Clin Orthop Relat Res 470(1):77–83
Dejour H, Neyret P, Donell ST (1998) Tibial tubercle osteotomy for access in lateral unicompartmental knee replacement. Knee 5(1):33–36
van Duren BH, Pandit H, Hamilton TW et al (2014) Trans-patella tendon approach for domed lateral unicompartmental knee arthroplasty does not increase the risk of patella tendon shortening. Knee Surg Sports Traumatol Arthrosc 22(8):1887–1894
Edmiston TA, Manista GC, Courtney PM et al (2017) Clinical outcomes and survivorship of lateral unicompartmental knee arthroplasty: does surgical approach matter? J Arthroplasty 33(2):362–365
Forster MC, Bauze AJ, Keene GCR (2007) Lateral unicompartmental knee replacement: fixed or mobile bearing? Knee Surg Sports Traumatol Arthrosc 15(9):1107–1111
Heyse TJ, Khefacha A, Peersman G, Cartier P (2012) Survivorship of UKA in the middle-aged. Knee 19(5):585–591
Kim KT, Lee S, Kim J, Kim JW, Kang MS (2016) Clinical results of lateral unicompartmental knee arthroplasty: minimum 2-year follow-up. Clin Orthop Surg 8(4):386–392
Liebs TR, Herzberg W (2013) Better quality of life after medial versus lateral unicondylar knee arthroplasty knee. Clin Orthop Relat Res 471(8):2629–2640
van der List JP, Chawla H, Zuiderbaan HA, Pearle AD (2016) Patients with isolated lateral osteoarthritis: unicompartmental or total knee arthroplasty? Knee 23:968–974
Lustig S, Lording T, Frank F et al (2014) Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 21(S1):S26–S32
Marson B, Prasad N, Jenkins R, Lewis M (2014) Lateral unicompartmental knee replacements: early results from a District General Hospital. Eur J Orthop Surg Traumatol 24(6):987–991
Newman SDS, Altuntas A, Alsop H, Cobb JP (2017) Up to 10 year follow-up of the Oxford Domed Lateral Partial Knee Replacement from an independent centre. Knee 24(6):1414–1421
Ohdera T, Tokunaga J, Kobayashi A (2001) Unicompartmental knee arthroplasty for lateral gonarthrosis: midterm results. J Arthroplasty 16(2):196–200
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2006) Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty 21(1):13–17
Romagnoli S, Verde F, Zacchetti S (2013) Lateral unicompartmental knee replacement: long-term survival study. In: Confalonieri N, Romagnoli S (eds) Small implants in knee reconstruction. Springer, New York, pp 59–70
Saxler G, Temmen D, Bontemps G (2004) Medium-term results of the AMC-unicompartmental knee arthroplasty. Knee 11(5):349–355
Schelfaut S, Beckers L, Verdonk P, Bellemans J, Victor J (2013) The risk of bearing dislocation in lateral unicompartmental knee arthroplasty using a mobile biconcave design. Knee Surg Sports Traumatol Arthrosc 21(11):2487–2494
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605
Volpi P, Marinoni L, Bait C, Galli M, Denti M (2007) Lateral unicompartmental knee arthroplasty: indications, technique and short-medium term results. Knee Surg Sports Traumatol Arthrosc 15(8):1028–1034
Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR (2015) Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(11):3281–3287
Walker T, Zahn N, Bruckner T et al (2018) Mid-term results of lateral unicondylar mobile bearing knee arthroplasty: a multicentre study of 363 cases. Bone Joint J 100B(1):42–49
Xing Z, Katz J, Jiranek W (2012) Unicompartmental knee arthroplasty: factors influencing the outcome. J Knee Surg 25(5):369–374
Danish Joint Registry (2017) Dansk Knaealloplastikregister Årsrapport 2017. https://www.sundhed.dk/sundhedsfaglig/kvalitet/kliniske-kvalitetsdatabaser/planlagt-kirugi/knaealloplastikregister/. Accessed 16 May 2018
Australian Joint Registry (2017) Australian Orthopaedic Association National Joint Replacement Registry Annual Report 2017: preservation mobile unicompartmental knee investigation supplementary. https://aoanjrr.sahmri.com. Accessed 16 May 2018
Gulati A, Weston-Simons S, Evans D et al (2014) Radiographic evaluation of factors affecting bearing dislocation in the domed lateral Oxford unicompartmental knee replacement. Knee 21(6):1254–1257
Robinson BJ, Rees JL, Price AJ, Beard DJ, Murray DW (2002) Dislocation of the bearing of the Oxford lateral unicompartmental arthroplasty. Bone Joint J 84(5):653–657
Hang JR, Stanford TE, Graves SE, Davidson DC, De Steiger RN et al (2010) Outcome of revision of unicompartmental knee replacement: 1,948 cases from the Australian Orthopaedic Association National Joint Replacement Registry, 1999–2008. Acta Orthop 81(1):95–98
van der List JP, Chawla H, Villa JC, Pearle AD (2016) Different optimal alignment but equivalent functional outcomes in medial and lateral unicompartmental knee arthroplasty. Knee 23(6):987–995
Hernigou P, Deschamps G (2004) Alignment Influences Wear in the Knee after Medial Unicompartmental Arthroplasty. Clin Orthop Relat Res 423(423):161–165
Vasso M, Del Regno C, D’Amelio A et al (2015) Minor varus alignment provides better results than neutral alignment in medial UKA. Knee 22(2):117–121
Acknowledgements
We would like to thank Willy Salemink from the Spaarne Gasthuis library for her assistance in the literature search.
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Contributions
JB performed the literature search, scanned all abstracts and full texts of the included articles, determined the quality of the studies and wrote the manuscript. LK screened all abstracts, full texts and determined the quality of the studies as a second author; and helped to draft the manuscript. IS provided suggestions on the review process, statistical analyses and manuscript; and checked the data extraction. HG participated in the design of the study and revised the manuscript. PN coordinated this study, participated in its design and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical approval
No ethical approval was obtained because this study was a systematic review using de-identified data from other cohort studies.
Appendix
Rights and permissions
About this article
Cite this article
Burger, J.A., Kleeblad, L.J., Sierevelt, I.N. et al. Bearing design influences short- to mid-term survivorship, but not functional outcomes following lateral unicompartmental knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 27, 2276–2288 (2019). https://doi.org/10.1007/s00167-019-05357-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05357-x