Abstract
Background
This study aimed to assess the long-term survivorship and functional outcomes of fixed-bearing lateral unicompartmental knee arthroplasty (UKA) in a young patients’ population with osteoarthritis limited to the lateral compartment.
Methods
The study included a cohort of consecutive patients who underwent lateral UKA between January 2008 and December 2014 at a single high-volume surgical center. The surgical procedures were performed by experienced surgeons using a lateral parapatellar approach and fixed-bearing implants. Patient follow-up included a retrospective re-evaluation, clinical assessments, patient-reported outcome measures (PROMs), and X-ray analysis.
Results
A total of 40 lateral UKAs were analyzed, with 19 performed on the left and 21 on the right knee. The mean age of the patients at the time of surgery was 57.6 years, and the mean BMI was 24.8. At the final follow-up, 80% of patients achieved excellent outcomes (OKS > 41), and 20% had good outcomes (OKS: 34–41). No patients exhibited fair or poor outcomes. The mean FJS at the final follow-up was 82.8. The mean WOMAC was 10.5. Kaplan–Meier survival analysis revealed a survivorship rate of 93.1% at 10 years, considering revision for any reason as endpoint.
Conclusions
Lateral UKA proved to be an effective treatment option for osteoarthritis affecting the lateral compartment of the knee. The study demonstrated a high survivorship rate and favorable functional outcomes at a mean follow-up of 132.7 months. These findings highlight the potential benefits of fixed-bearing lateral UKA in selected patients with lateral compartment knee pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicompartmental knee arthroplasty (UKA) has emerged as a highly effective alternative to total knee arthroplasty (TKA) for the treatment of arthritis affecting either the medial or lateral compartment of the knee [1].
Specifically, for patients with osteoarthritis isolated to the lateral compartment, lateral unicompartmental knee arthroplasty offers a suitable treatment option when appropriate patient selection criteria are applied [2]. In comparison to TKA, UKA presents several advantages, including a bone-conserving and ligament-sparing surgical technique, faster recovery, improved range of motion and functional outcomes, as well as shorter hospital stays [3].
Despite these benefits, UKA procedures account for only a small percentage (8–12%) of knee arthroplasties, with a mere 10% of these cases addressing the lateral compartment [4]. Various factors contribute to this disparity. Firstly, lateral osteoarthritis is less prevalent, affecting approximately 1% of the population, compared to its medial counterpart [5].Additionally, there are distinct anatomic and kinematic differences between the medial and lateral compartments, such as increased laxity, smaller anteroposterior dimensions, and greater mediolateral length, which pose unique challenges for UKA designs [6]. Consequently, some UKA designs exhibit reduced adaptability and a higher incidence of bearing dislocation, particularly in the case of mobile bearing lateral UKA, leading to diminished confidence in lateral UKA procedures [7].
Nevertheless, when the correct surgical technique and implant design are employed, lateral UKA has demonstrated long-term survivorship rates comparable to those of medial UKA and TKA [8]. As a result, this procedure may be an underutilized solution for patients with osteoarthritis limited to the lateral compartment of the knee. Therefore, the objective of this study is to evaluate the clinical outcomes and long-term survivorship rates of lateral UKA with extended follow-up. We hypothesize that the survivorship rate and functional outcomes will be favorable at a minimum follow-up period of 10 years, and that they will also be comparable to the previously demonstrated results for the same procedure and prosthetic design used for medial osteoarthritis.
Methods
This study included a comprehensive analysis of patients who underwent lateral fixed-bearing unicompartmental knee arthroplasty (UKA) between January 1, 2008, and December 31, 2014, at a single high-volume surgical center. The patient cohort comprised individuals diagnosed with lateral osteoarthritis of the knee, either primary idiopathic or secondary (post-traumatic lateral arthrosis or resulting from osteonecrosis). A retrospective evaluation was conducted using long-term follow-up data.
The selection criteria for unicompartmental prosthesis implantation were as follows: lateral unicompartmental pain, an intact anterior cruciate ligament, knee flexion beyond 90°, extension limitation with a maximum deficit of 10°, correctable valgus deformity of maximum 15°, and a lateral minimum Kellgren–Lawrence (KL) grade 3 status indicating lateral osteoarthritis or signs of avascular osteonecrosis (AVN) observed on MRI. Exclusion criteria for UKA encompassed symptomatic patellofemoral osteoarthritis or evidence of medial compartment osteoarthritis greater than Kellgren–Lawrence grade 2. Minor cartilaginous lesions or fibrillation in other compartments were not considered contraindications. Furthermore, intraoperative evaluations of the patellofemoral compartment and the medial compartment were performed in all cases to exclude arthrosis or chondropathy.
Preoperative data collection involved anteroposterior, lateral, and Rosenberg weight-bearing X-rays, as well as MRI scans, for all patients. The surgical procedures were carried out by two experienced surgeons, utilizing a lateral parapatellar approach and two types of fixed-bearing implants: the ZUK (Zimmer® Unicompartmental High Flex Knee Zimmer Warsaw US, Now LimaCorporate® San Daniele del Friuli IT) and the Accuris Unicompartmental Knee (Smith and Nephew® Warsaw US).
The ZUK implant is a fixed-bearing unicompartmental prosthesis designed for use in both the medial and lateral compartments. It consists of a polyradial cobalt-chrome alloy femoral component with twin pegs, a titanium tibial tray with two lugs and a keel, and a polyethylene liner comprising anterior and posterior flaps that securely fit into the tibial tray. The liner is flat, resulting in a noncongruent round-on-flat articulation.
The Accuris implant, on the other hand, is a fixed-bearing femoral resurfacing implant performed with a reaming system referencing off the cut surface of the tibia. It is available in cobalt-chrome or Oxinium® (used in this study) femoral components with a single peg and keel, and a titanium tibial tray with a single keel and a polyethylene liner (an all-poly tibial component, although not used in this study, is also available). Like the ZUK, the Accuris implant features a flat liner for a noncongruent round-on-flat articulation.
A standardized surgical technique utilizing a mini lateral parapatellar approach was employed in all patients. An extramedullary tibial guide was utilized for the tibial cut, while a dedicated distal femoral cutting system (spacer block technique) and a dedicated femoral cutting guide were used for the ZUK implant. For the Accuris implant, a “shim-based” tibial cut was performed to resurface the femur. Cementation was performed for all components, with the femoral component positioned as laterally as possible and the tibial component chosen to ensure maximum coverage without protrusions. The polyethylene insert was placed at the end of cementation, with the thickness selected to ensure optimal articulation and stability. A tourniquet was utilized during all procedures. Postoperative rehabilitation protocols included immediate full weight-bearing supported by crutches during the first 4 weeks, with physiotherapy focused on immediate active extension and flexion.
All patients received venous thromboembolism (VTE) prophylaxis with low-molecular-weight heparin for 30 days following surgery. Alternatively, patients who were already on chronic anticoagulant therapy resumed their regular treatment immediately after the procedure. Routine perioperative prophylactic antibiotic therapy was administered to all patients using cefazolin, with the exception of individuals with allergies.
During the study period the percentage of lateral UNIs accounted for 10% of the total amount of UNIs performed, which were 20–25% of the total amount of knee arthroplasties performed.
Clinical outcomes
All patients were prospectively followed up both clinically and radiographically, at 3–6 months and then yearly. For all the patients, at the end of follow up, were collected “the Western Ontario and McMaster Universities Arthritis Index” (WOMAC score) [9], “Oxford Knee Score” (OKS) [10] and the “Forgotten Joint Score” (FJS-12) [11]. In the cases undergoing prosthetic revision, all the information relating to the indication for revision and the revision procedure were collected.
Concerning the Radiological evaluation, standard A-P x-rays, lateral view and long standing x-rays.
were analyzed at all follow-ups to evaluate the presence of radiolucent lines according to the Knee Society radiological analysis [12]. Standing long alignment radiographs to include hip/knee/ankle were evaluated for the overall limb alignment. The evaluation was performed on digital picture archiving and communication system PACS (Carestream, USA) on calibrated Digital Imaging and Communications in Medicine (DICOM) radiographs. The study was approved by the local institutional review board (number 2015001968).
Statistical analysis
Statistical analysis was carried out by an independent statistician. Categorical variables were described using frequency and percentage distributions. Continuous variables were described using arithmetic mean and standard deviation (SD).
Results
Between January 1, 2008, and December 31, 2014, a total of 51 lateral UKA were implanted in 51 patients (38 ZUK and 13 Accuris unicompartmental lateral knee prostheses). 11 patients were excluded from the study for different causes: 3 patients died due to causes unrelated to the implant, 3 patients were not available for final follow-up and 5 patients were excluded as they underwent simultaneous medial UKA or patello-femoral joint implantation (2 and 3 patients, respectively). Thus, a total of 40 unicompartmental lateral prostheses were included in this retrospective evaluation.
Table 1 displays the baseline demographics of the 40 patients at the time of surgery. Of these patients, 15 were males and 25 were females. There were 19 left UKAs and 21 right UKAs. The mean age of the patients at the time of the operation was 57.6 years (range 40–68, SD 9.1), and the mean BMI was 24.8 (SD 3.1). Among the UKAs performed, 10 were for condylar osteonecrosis, 10 for post-traumatic lateral arthritis (secondary to fracture or ligamentous injury), and 20 for lateral femoro-tibial osteoarthritis (including post lateral meniscectomy) with a Kellgren–Lawrence grade ≥ 3 on X-rays. Three prosthetic implants required revision. Clinical outcomes and radiological data were collected for 37 patients after accounting for deaths, revisions, and exclusion criteria. The patients’ outcomes were assessed at a mean follow-up of 132.7 months (SD 22.8). The average time to revision, in the three identified cases, was 112 months (SD 48.1). The three revisions were performed due to the progression of osteoarthritis in other joint compartments (Table 2) in two cases by implanting another small implant (one medial UKA and one patello-femoral arthroplasty) and in one case with a primary total knee replacement (Table 2). The mean Oxford Knee Score (OKS) at the final follow-up was 42.8 (SD 4.0). At the last follow-up, 32 patients (80%) achieved excellent outcomes (OKS > 41), while eight patients (20%) achieved good outcomes (OKS: 34–41). No patient exhibited fair outcomes (OKS: 27–33) or poor outcomes (OKS < 27). The mean Forgotten Joint Score (FJS) at the final follow-up was 82.8 (SD 5.2) (Table 3). The mean WOMAC score at the final follow-up was 10.5 (SD 10.2). The survival analysis demonstrated an implant survival rate of 93.1% at 10 years (Fig. 1).
Radiographic results
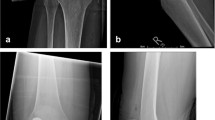
No progressive radiolucent lines were found around the implants. In four cases (10%), non-significant early static radiolucent lines were found underneath the tibial plate in postoperative radiographs (Fig. 2).
Standing long alignment radiographs to include hip/knee/ankle showed a mean preoperative valgus alignment of 8.7° (SD 4°) and a mean postoperative valgus alignment of 3.7° (SD 1°). (Fig. 3).
Discussion
The primary finding of this study is that lateral unicompartmental knee arthroplasty (UKA) is an effective treatment option for patients with lateral osteoarthritis of the knee, either primary idiopathic or secondary (post-traumatic lateral arthrosis or resulting from osteonecrosis). In the analyzed cohort, lateral UKA demonstrated an overall survivorship higher than 90% at 10 years, with successful patient-reported outcomes over a mean follow-up period of 132.7 months. This survivorship rate is comparable to other studies in the literature. The drop evident in the survival curve at 12 years is related to the fact that not all patients reach a follow-up over 12 years so the curve after that timeline drops as survivorship data are not available for all the analyzed patients (Fig. 2). This is not related to a failure of the implants. A review of 47 studies encompassing 2,162 patients reported a mean survivorship of 88.6% (range 74.5–100) with a minimum follow-up of 60.7 months (range 7–204) [13]. Additionally, Plancher et al. reported an overall survivorship of 98% at 5 years and 96% at 10-year follow-up for 61 patients who underwent lateral fixed-bearing non-robotic UKA [14].
In this study, a fixed-bearing unicompartmental prosthesis was used in all patients. When comparing the results of this series to studies on mobile-bearing implants, it has been observed that implant survivorship and clinical outcomes are similar. However, a fixed-bearing design is preferred due to the higher revision rate associated with bearing dislocations in mobile-bearing UKAs [15, 16].
Despite the advantages of unicompartmental arthroplasty over total knee arthroplasty (TKA), many surgeons still favor TKA over UKA for lateral osteoarthritis. However, the benefits of UKA, such as less invasive surgery, reduced blood loss, faster recovery, and superior functional outcomes, make it a favorable option. Only a limited number of studies have compared TKA and lateral UKA. Van der List et al. evaluated 82 patients with isolated lateral osteoarthritis, of whom 48 underwent lateral UKA and 34 underwent TKA. Their findings indicated that the UKA group exhibited better functional outcomes, particularly in younger patients and women [3].
Medial UKA has been widely adopted as a surgical solution for osteoarthritis limited to the medial compartment of the knee, demonstrating excellent clinical outcomes. In 2022, Rossi et al. published prospective data on 148 medial UKAs using the ZUK implant, showing an overall survivorship of 89.52% at 173 months of follow-up. Comparing the clinical outcomes of the lateral UKA cohort in this study with the results reported for the ZUK implant in the medial compartment, the mean Oxford Knee Score (OKS) was slightly higher in the medial UKA patients (43.02 in the medial compartment and 42.7 in the lateral compartment), while the Forgotten Joint Score (FJS) was better in the lateral UKA cohort (77.6 in the medial compartment and 82.9 in the lateral compartment) [17].
Comparing lateral to medial unicompartmental knee arthroplasty, a systematic review conducted by Van der List et al. found no statistically significant difference in survivorship between the two procedures at a 10-year follow-up (88.9% for medial UKAs and 89.4% for lateral UKAs) [4]. Another Kaplan–Meier analysis based on data from the Register of Orthopaedic Prosthetic Implants (RIPO) in Emilia Romagna, Italy, involving 5571 UKAs (5215 medial UKAs and 356 lateral UKAs), revealed a higher survivorship rate in lateral UKAs (95.2%) compared to medial UKAs (87.5%) at a 10-year follow-up [18].
The data presented in this study, with a similar case mix in terms of indications, are in line with those recently presented by Marullo et al. [19] that showed good outcomes of lateral UKA in patients with a posttraumatic arthritis of the lateral compartment comparing to a matched group operated for primary OA. The same group recently published a study [20] showing that a postoperative residual mild valgus of less than 3° on the HKA drives to lower outcomes and survivorship comparing to a moderate valgus of more than 3°; the postoperative results in this study showed a mean of 3.7° of residual valgus with 1° standard deviation that puts the majority of the patients in the safer and better performing group according to Marullo et al.
It is important to note that this study has limitations, including the small sample size, the retrospective nature (despite prospective data collection), and the use of two different implants without a comparison with a mobile bearing lateral UKA design or with a TKA group.
The choice to evaluate two different implants was justified by several reasons: first of all to reach a consistent number of patients to be analyzed, second as both implants had a fixed bearing and similar features and third because, despite two different specific surgical techniques, both prostheses were implanted respecting the same principles by the senior authors, who performed the surgeries.
Conclusions
Fixed bearing lateral UKA demonstrated excellent clinical outcomes and survivorship at 10 years in a young patients’ population.
Lateral UKA can be an effective treatment option for lateral osteoarthritis of the knee, either primary idiopathic or secondary (post-traumatic lateral arthrosis or resulting from osteonecrosis in a patients’ population younger than 60 years old with a survival rate of 93.1%.
References
Johal S, Nakano N, Baxter M et al (2018) Unicompartmental knee arthroplasty: the past, current controversies, and future perspectives. J Knee Surg 31:992–998. https://doi.org/10.1055/s-0038-1625961
Smith E, Lee D, Masonis J, Melvin JS (2020) Lateral unicompartmental knee arthroplasty. JBJS Rev 8:e0044. https://doi.org/10.2106/JBJS.RVW.19.00044
van der List JP, Chawla H, Zuiderbaan HA, Pearle AD (2016) Patients with isolated lateral osteoarthritis: unicompartmental or total knee arthroplasty? Knee 23:968–974. https://doi.org/10.1016/j.knee.2016.06.007
van der List JP, McDonald LS, Pearle AD (2015) Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee 22:454–460. https://doi.org/10.1016/j.knee.2015.09.011
Buzin SD, Geller JA, Yoon RS, Macaulay W (2021) Lateral unicompartmental knee arthroplasty: a review. World J Orthop 12:197–206. https://doi.org/10.5312/wjo.v12.i4.197
Kamenaga T, Hiranaka T, Hida Y et al (2020) Morphometric analysis of medial and lateral tibia plateau and adaptability with Oxford partial knee replacement in a Japanese population. J Orthop Surg (Hong Kong) 28:2309499020919309. https://doi.org/10.1177/2309499020919309
Pandit H, Jenkins C, Beard DJ et al (2010) Mobile bearing dislocation in lateral unicompartmental knee replacement. Knee 17:392–397. https://doi.org/10.1016/j.knee.2009.10.007
Burger JA, Kleeblad LJ, Sierevelt IN et al (2020) A comprehensive evaluation of lateral unicompartmental knee arthroplasty short to mid-term survivorship, and the effect of patient and implant characteristics: an analysis of data from the dutch arthroplasty register. J Arthroplasty 35:1813–1818. https://doi.org/10.1016/j.arth.2020.02.027
McConnell S, Kolopack P, Davis AM (2001) The Western Ontario and mcmaster universities osteoarthritis index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 45:453–461. https://doi.org/10.1002/1529-0131(200110)45:5%3c453::aid-art365%3e3.0.co;2-w
Whitehouse SL, Blom AW, Taylor AH et al (2005) The Oxford knee score; problems and pitfalls. Knee 12:287–291. https://doi.org/10.1016/j.knee.2004.11.005
Kacmaz IE, Gezer MC, Basa CD et al (2022) Use of the forgotten joint score (FJS)-12 to evaluate knee awareness after isolated anterior cruciate ligament reconstruction with and without meniscus repair or partial meniscectomy. Eur J Orthop Surg Traumatol 32:413–418. https://doi.org/10.1007/s00590-021-02991-5
Ewald FC (1989) The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 248:9–12
Bonanzinga T, Tanzi P, Altomare D et al (2021) High survivorship rate and good clinical outcomes at mid-term follow-up for lateral UKA: a systematic literature review. Knee Surg Sports Traumatol Arthrosc 29:3262–3271. https://doi.org/10.1007/s00167-020-06129-8
Plancher KD, Briggs KK, Chinnakkannu K et al (2022) Isolated lateral tibiofemoral compartment osteoarthritis: survivorship and patient acceptable symptom state after lateral fixed-bearing unicompartmental knee arthroplasty at mean 10-year follow-up. J Bone Joint Surg Am 104:1621–1628. https://doi.org/10.2106/JBJS.21.01523
Hariri M, Zahn N, Mick P et al (2023) Fixed-bearing is superior to mobile-bearing in lateral unicompartmental knee replacement: a retrospective matched-pairs analysis. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-023-07417-9
Abu Al-Rub Z, Lamb JN, West RM et al (2020) Survivorship of fixed vs mobile bearing unicompartmental knee replacement: a systematic review and meta-analysis of sixty-four studies and national joint registries. Knee 27:1635–1644. https://doi.org/10.1016/j.knee.2020.09.004
Rossi S, Sangaletti R, Nesta F et al (2022) A well performing medial fixed bearing UKA with promising survivorship at 15 years. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04562-7
Alesi D, Bordini B, Fratini S et al (2022) Lateral unicompartmental knee arthroplasty (UKA) showed a lower risk of failure compared to medial unicompartmental knee arthroplasty in the register of prosthetic orthopedic implants (RIPO). Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04631-x
Romagnoli S, Vitale JA, Marullo M (2020) Outcomes of lateral unicompartmental knee arthroplasty in post-traumatic osteoarthritis, a retrospective comparative study. Int Orthop (SICOT) 44:2321–2328. https://doi.org/10.1007/s00264-020-04665-z
Marullo M, Russo A, Spreafico A, Romagnoli S (2023) Mild valgus alignment after lateral unicompartmental knee arthroplasty led to lower functional results and survivorship at mean 8-year follow-up. J Arthroplasty 38:37–42. https://doi.org/10.1016/j.arth.2022.07.009
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
SMPR and RS designed and were responsible for the study; LA, AM and RS contributed to write the manuscript and finalize the statistical section; LA and LA were responsible for the clinical follow-up of the patients; SMPR and FB revised the manuscript. The study was approved by the local ethical committee with IRB Approval No. 2015001968.
Corresponding author
Ethics declarations
Conflict of interest
FB declares a teaching contract with the manufacturer (Zimmer Biomet and Limacorporate). No conflict of interest to be declared by any of the authors for the current study. FB is Consultant for Zimmer Biomet and Limacorporate; Grants from Limacorporate; Royalties from Zimmer Biomet and Limacorporate. The other authors have no disclosures.
Ethical approval
This study obtained IRB Approval (No. 2015001968) and written consent was obtained from all patients.
Informed consent
Written consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sangaletti, R., Andriollo, L., Montagna, A. et al. Lateral UKA can be a safe solution in a young patients’ population: a 10-year follow-up report. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-023-05189-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-023-05189-y