Abstract
Purpose
Total knee arthroplasty (TKA) leaves 11–25% of the patients unsatisfied, and patellofemoral joint pain is one cause. This study aimed to compare the differences between kinematics and load transfer in the same knee with axial internal/external rotation of the femoral component (CoRo) versus a separate axial internal/external trochlear groove rotation (TrRo) which is included in the TKA trochlea design.
Methods
A validated weight-bearing finite element model with modifications of the TKA axial femoral component rotation (CoRo) and a modified trochlear rotation (TrRo) was calculated and analysed.
Results
Compared to the neutrally implanted TKA at 105° of flexion, a 6° external rotation of the trochlear groove reduced the retropatellar stress by 7%, whereas a 3° internal trochlear groove rotation increased the retropatellar stress by 7%. With femoral component rotation, the tibia inlay stress of 6.7 MPa at 60° of flexion was two times higher both with a 3° internal component rotation and a 6° external rotation.
Conclusion
These results demonstrate in the tested TKA design that a trochlear groove rotation can reduce retropatellar stress. Additionally, during the TKA operation, the surgeon should be aware of the significant influence of axial femoral component rotation on mechanical inlay stress during flexion and of the fact that even small changes in the patellofemoral joint may influence the tibiofemoral joint. These results support that an external rotation of the femoral component should be preferred in TKA to avoid anterior knee pain. Furthermore, new developed TKA designs should integrate an externally rotated trochlea groove.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) leaves 11%–25% of patients unsatisfied [3, 14, 43, 45]. Pain in the patellofemoral joint is a possible consequence of the new loading and kinematic conditions after TKA [45]. In an uninjured knee, the trochlea is the guide rail for the patella, capturing the patella starting at 30° of flexion [1]. TKA changes the relevant kinematics and forces, especially for the retropatellar joint, resulting in complications as observed in various studies [9, 19, 29, 32, 36, 39, 50, 51].
Regarding the intraoperative positioning of TKA components, certain studies have shown that an external rotation of the femoral component obtains a more natural kinematic state with less retropatellar pressure [5, 18, 49]. Moreover, clinical observations have demonstrated that the internal rotation of the femoral component may be responsible for the patellofemoral pain syndrome [11, 13, 42]. These data have motivated most TKA manufacturers and orthopaedic surgeons to recommend a slight external rotation of the femoral component for most TKA systems.
The knee is not a simple hinged joint. Rather, it contains three distinct articulations: the patellofemoral, medial and lateral tibiofemoral joints. Therefore, it is evident that changing the axial rotational alignment of the femoral component influences all parts of the knee including both tibiofemoral compartments and the patellofemoral joint. The patellofemoral kinematics, due to external rotation of the femoral component, display a more lateral shift [5, 6, 39, 46] and a more lateral tilt [6, 39, 40] compared to a neutral alignment. The tibiofemoral kinematics after external rotation of the femoral component produces more external rotation of the tibia with respect to the femur in case of deep flexion because of the changed flexion gap, which causes the knee to move in a more varus orientation [39, 40]. Consequently, a knee with a rotated flexion gap exerts different tensions on its associated ligaments. Particularly, an external component rotation due to a more varus position in flexion generates more tension in the lateral collateral ligament (LCL) and less tension in the medial collateral ligament (MCL) [20]; an internal rotation of the femoral component has likewise been shown to produce more laxity in the lateral compartment [5]. These changed kinematics and loading conditions may influence wear patterns and thus perhaps the long-term outcome of a TKA intervention.
Generally, surgeons and engineers attempt to replicate the body’s native kinematics with correct implant positions or new implant designs. However, changing the femoral component rotation during the operation precludes full kinematic restoration in the knee’s components, including the medial and lateral tibiofemoral joint and the patellofemoral joint. The interconnected relationships among these joint partners are not completely understood [39] although one experimental study demonstrated a new implant design that externally rotated only the trochlea and, therefore, only the patellofemoral joint reduced the retropatellar pressure [49]. However, questions regarding how the trochlear groove rotation in the TKA design may influence the kinematics, loading, and ligament forces compared to intraoperative external component rotation within the same knee have not yet been thoroughly addressed. An improved understanding of the relationship between the patellofemoral and tibiofemoral joint would contribute significant insights for new implant designs and optimized implant positions.
Various TKA designs, interindividual knee kinematics, and complex measuring methods make in vivo investigations difficult. Therefore, researchers have developed in vitro tests that attempt to replicate the in vivo environment. For instance, there are knee rig arrangements for human specimen testing that have been shown to produce reliable experimental results which are at least partially transferable to the patient [52]. However, these experimental test rigs are of limited use because of the decomposition of the cadaver knees and because different TKA positions require different bone cutting approaches during implantation. To address these limitations, in silico models have shown distinct advantages and have also been proven to generate reliable results when experimentally validated [7, 8, 10, 15,16,17, 22, 26, 27, 30, 33, 44, 58].
Various TKA implant designs exist, and surgeons regionally choose implants based on their personal preference. In Germany, the most commonly used implant design in 2016 was the cruciate retaining (CR) design constituting 55.1% followed by the posterior-stabilized (PS) design with 16.8% and cruciate sacrificing (CS) design with 11.7%. Furthermore, in Germany, the fixed bearing type of TKA implants is used in 78.4% of the cases and the mobile bearing type is used in 21.6% [24]. TKA implant design studies show an influence of the trochlea design and, therefore, also in the retropatellar stress especially in unresurfaced condition which constitutes 90% of the TKA cases in Germany [4, 24, 35, 55]. Due to the various influential factors, it is necessary to test design variations within one implant design to hold other possible confounders constant.
In this context, a fixed bearing CR TKA design was used in this study, and it aimed to compare the differences between the kinematics and load transfer in the same knee with axial internal/external rotation of the femoral component (CoRo) versus a separate trochlear groove rotation (TrRo) included in the TKA design. This comparison was conducted using a computer model (finite element method). The hypothesis was as follows:
-
1.
Mechanical stress within the patellofemoral joint is lower using external rotation of the trochlea design.
-
2.
TrRo has less influence on the tibiofemoral kinematics than CoRo.
-
3.
The inlay load increases due to either external or internal CoRo.
Materials and methods
Based on a previous study, the finite element analysis was conducted with the static structural software tool Ansys V14 (Ansys, Inc., Canonsburg, PA, USA) and the default sparse direct solver. This model was validated with an experimental weight-bearing knee rig in a former study and, therefore, is described here only briefly [56]. A further validation step, described in Woiczinski et al., was completed to verify the material properties of the TKA components used in this in silico model [57].
A reconstructed geometric 3D model of the lower extremity of a person (age: 28; weight: 80 kg; height: 173 cm) with no surgical injuries and no pathologic signs was used for the in silico simulation. For all the various simulation models, a fixed-bearing total knee prosthesis (Columbus CR, Aesculap Orthopaedics, Tuttlingen, Germany) was virtually implanted following the manufacturer’s recommendations and under the control of an experienced orthopaedic surgeon.
The ligament structures (LCL; PCLa; PClp; MCLa; MCLo; MCLs) of the in silico knee model were simulated with linear spring elements (Table 1) [56, 47].
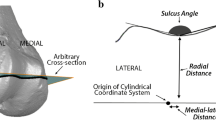
The patellofemoral (\({\mu _1}\)) and tibiofemoral (\({\mu _2}\)) contacts were simulated with friction coefficients of \({\mu _1}=0.02\) and \({\mu _2}= 0.05\) [21, 34, 37]. For the simulation a coordinate system was established in full extension at the distal tibia. The Z-axis was pointed to the femoral head and X-axis was aligned parallel to the mediolateral transepicondylar axis of the femur. The knee was free to move in six DOFs (degrees of freedom) [56].
The femur, tibia, patella, and femoral component of the implant were rigid bodies; the inlay and patella cartilage were deformable bodies.
Muscle forces were simulated with self-programmed spring elements to ensure correct force direction during the whole flexion cycle. Additionally, a simulation of the quadriceps tendon was developed to simulate the effect of quadriceps wrapping [31]. The knee squat simulation modelled flexion of up to 105° within 60 load steps. The force of the vastus intermedius and rectus femoris, simulated with one linear spring, was adapted with respect to the ground reaction force during the whole flexion. For every single load step, the value of the ground reaction force was verified to be between 50 and 55 N. If this was not the case, the force of vastus intermedius and rectus femoris was adapted till the ground reaction force was reached. As the forces of the vastus intermedius and rectus femoris were programmed to maintain this ground reaction force, they exhibited, in the former validation study, values of up to 700 N during deep flexion and, therefore, simulated realistic weight-bearing conditions [56]. The musculus vastus lateralis and musculus vastus medialis were defined with a constant load of 20 N. Additionally, the biceps femoris and semitendinosus were defined with constant loads of 10 N each.
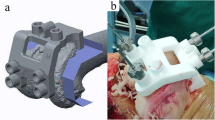
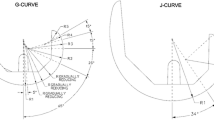
The following modifications of the axial femoral component rotation (CoRo) and the designed trochlear rotation (TrRo) were implemented with the CAD software (Catia V5R19, Dassault System) and were tested in the same FEA (Finite Element Model) knee model. Neutral alignment of the original TKA implant was according to the manufacturer’s manual in line with the anatomical transepicondylar axis. To implement the different axial rotation angles, the centre of the implant was defined as the rotation centre, and different axial internal/external rotation angles of 3° internal, 3° external, and 6° external rotation were simulated (Fig. 1) and compared to the neutral (0°) alignment. In total, seven different finite element models were calculated and analysed (Table 2).
The ethics committee of the University of Munich verified the study design as being in accordance with the international ethical principles for medical research and approved this study (Number 58–16).
To compare the load distribution of the retropatellar and tibiofemoral joints, the von Mises stresses of the patella cartilage within the inlay were analysed. For the tibiofemoral kinematic comparison, the AP movement, tibial rotation, and varus/valgus movements were analysed. Patella kinematics was analysed with regard to tilt and shift. Moreove, all tensions in the ligaments were considered for all rotation variations. All results were analysed in flexion increments of 10° beginning from 20°. GraphPad Prism 5 (GraphPad Software, Inc., La Jolla, USA) was used, and points were fitted with a nonlinear fourth-order polynomial.
Results
For the neutral model, retropatellar stress showed a maximum of 0.5 MPa at 20° of flexion, and the TrRo did not influence the stress until 60° of flexion. After 60° of flexion, differences in the retropatellar stress could be recognized. The absolute value at 105° of flexion for a 3° internal TrRo marked an increased retropatellar stress of 3.2 MPa, and the external TrRo reduced this to 2.8 MPa (Fig. 2). An external TrRo resulted in lower stress on the patella ridge and higher stress on the lateral side of the patella. The TrRo did not alter the stress on the inlay during flexion. The neutral femoral orientation model showed stresses ranging from 4.5 (20°) to 8.9 MPa (105°).
“Appendix 1” presents all tensions in all ligament structures that accompany the TrRo implementation. All TrRo models resulted in similar trends.
The tibiofemoral kinematics of TrRo showed differences only in the rotation of the tibia (Fig. 3). The greatest differences in tibial rotation due to TrRo was found between the 3° internal TrRo at 60° of flexion, which showed − 2° internal tibial rotation, compared to the 6° external TrRo, which showed 2.5° external tibial rotation.
Differences in the patella rotation were observed only from 70° of flexion (Fig. 4). The lateral patella tilt increased with external TrRo: between 3° internal and 6° external trochlear rotation, the patella tilt varied by approximately 9.5° at 20° of flexion. For higher flexion angles, differences in the patellar tilt became smaller. The patellar shift behaved similar to the tilt. The maximum value between 3° internal and 6° external TrRo, at 20° of flexion, was 6.5 mm to the lateral side. At 105° of flexion, the difference introduced by TrRo was negligible.
The CoRo with 3° internal rotation increased the retropatellar stress to an absolute maximum of 3.2 MPa at 105° of flexion, in comparison to the neutral rotation model (3.0 MPa). Figure 5 details the stress distribution, which showed a variance of the peak stress only at the patella ridge. For the inlay, CoRo showed changes in load and in localization of the peak stresses. At 60° of flexion, the stress in the neutral orientation was 6.7 MPa, located on the medial side (Fig. 6). An internal CoRo of 3° increased the medial peak value to 11.1 MPa. At 60° of flexion, an external CoRo induced a maximum stress of 7.3 MPa (3°) and 11.9 MPa (6°) and also changed the compartmental position to the lateral side.
CoRo affected all ligament tensions during flexion. An internal CoRo increased the tension in in all portions of the MCL (MCLa, MCLs, and MCLo) and PCL (PCLa and PCLp). At 50° of flexion, the external CoRo induced a higher tension in the LCL, up to 241N for the 6° external rotation model compared to 16 N for the neutral CoRo (“Appendix 2”).
The tibiofemoral kinematics presented differences in all CoRo models (Fig. 7). The tibia exhibited a higher internal rotation until 60° of flexion, caused by the 3° internal CoRo. With rising flexion angles, all tibial rotations showed nearly the same level. Tibial movement in the varus-valgus direction for 6° external CoRo at 105° flexion showed a 12.6° higher varus position in contrast to 3° internal CoRo. Femoral AP movement for all modifications showed similar curve progressions.
Discussion
The most important finding of the present study was a lower retropatellar stress after external axial rotation of the trochlear groove and higher stress due to internal axial rotation. Compared to the total axial femoral component rotation, the TKA designs that included the trochlear groove rotation generated similar smaller retropatellar stresses and had fewer side effects on the tibiofemoral kinematics and stress distribution.
Anterior knee pain remains a major problem in TKA, and the retropatellar pressure that seems to be responsible [19, 29, 36, 50, 51] for a part of the pain is influenced by the internal and external rotation of the femoral component [2, 5, 11,12,13, 38, 42, 46]. Surgeons often attempt to modify the kinematic environment by aligning the femoral component; unfortunately, it is not possible to restore patellofemoral and tibiofemoral conditions simply by rotating the femoral component, even if a link between these joints seems obvious [39]. In this study, the ligament forces, tibial rotation, varus–valgus position, inlay and retropatellar stress were heavily influenced with femoral component rotation. The reduction in retropatellar stress by external rotation has also been observed experimentally [18] and in clinical outcomes where an internal rotation should be avoided [11, 42]. A study by Steinbrück et al. investigated only the trochlear rotation using an experimental knee rig setup and showed similar effects on the retropatellar pressure [49]. A clinical study which shows implant trochlear height of different femoral component designs is related to secondary patellar resurfacing also validates our result of the significant influence of small trochlea design changes to the retropatellar loading [55].
Femoral component rotations showed significant influence on the inlay stress. Not only was the maximum stress on the inlay changed because of the complete rotation of the femoral component, but the medial predominant maximum that is normally seen in TKA [25] was shifted to the lateral side. For both femoral rotational modifications, 3° internal and 6° external, the stress on the inlay was two times higher compared to the neutral alignment, and, therefore, may impact bone interface stability or wear patterns. One explanation for this difference in the inlay stress may be the different ligament situation caused by a rotated flexion gap. Axial external rotation of the femoral component forces the knee into a more varus position with further flexion, which was also seen in the tibiofemoral kinematic patterns. This different relative position between the femur and the tibia influences the ligament strain pattern and is responsible for more force on the ligaments, i.e. more LCL force due to external rotation. This changed ligament pattern is then transferred to the inlay stress because of increased compression in the lateral compartment. Miller et al. and Merican et al. [39, 40] also revealed in their experimental studies that a rotated flexion gap is linked to more forces on the ligaments, further supporting the component rotation origin of the increased stress on the inlay. However, this situation will probably not be encountered often in the TKA because the surgeon would probably notice the stiffer ligaments and release these in some cases. Nevertheless, the rotation of the femoral component warrants increased attention during implantation.
The tibiofemoral kinematics changed because of the trochlear groove rotation, especially between 50° and 80° of flexion. Not surprisingly, an externally rotated trochlea design changed the tibia’s axial rotation (internal/external) at the beginning of the knee flexion because the patella was shifted laterally and, therefore, the tuberositas tibiae moved the tibia to an external rotation. However, the most significant difference in tibial rotation caused by the trochlear groove rotation design appeared at 70° of flexion, with 4.6° more external tibial rotation compared to internal trochlear rotation, which is not self-evident in this amount and at this range of flexion. The detailed perspective on the ligament situation also showed that this range of motion (50° to 80° of flexion) was accompanied by the highest differences in forces for the MCLa, thereby proving ligament influence on the tibiofemoral kinematics and vice versa [54]. The shift and tilt of the patellar kinematics were also greatest in this range of motion in the lateral direction, suggesting that the patellar movement is one possible influencing factor for the tibiofemoral differences.
The limitations of this study should also be considered when transferring the results of the numerical simulation to the patient. First, this was an experimental study, and not all in vivo situations can be recreated when a biomechanical setup is developed. Simulating weight-bearing is essential and, therefore, we decided to use a 50-N ground reaction force, even if this is not a realistic patient weight. Müller et al. showed that the highest influence is provided by weight-bearing versus passive motion, and therefore, we believe that transferable results were generated in this study [41]. Furthermore, in this study, the hamstring and vastus medialis and lateralis were simulated with constant load which might also influence the study results [53] but are necessary to stabilize the knee. Additionally, the FEA knee simulation was validated previously with 15 specimens for mechanical parameters (retropatellar pressure, retropatellar area and quadriceps force) and with 7 specimens for kinematic parameters (tibia rotation, AP movement, patellar shift, patella tilt, patellar rotation and patella flexion) with the identical boundary conditions and the same TKA implant, and it showed good agreement with the experiments [56]. However, the FEA only represents one patient anatomy which should be considered when transferring these results. Choosing only one implant design is also a limiting factor but as mentioned, it is necessary because the influence of all TKA implant design aspects is significant. In this study, a fixed CR design implant was used which was implanted more than 215,000 times worldwide and has a trochlea design which is comparable with other commercially available CR trochlea designs. Furthermore, we did not resurface the patella. The topic of resurfacing the patella is still under debate [23, 28] and current literature shows that resurfacing the patella increases the patellofemoral loading after TKA [48].
Conclusion
In conclusion, this study showed that an external trochlear groove rotation implemented in the tested TKA design can reduce the patellofemoral stress. Second, during operation procedures, the surgeon should be aware that an axial femoral component rotation heavily influences the mechanical stress in the inlay and the forces on the ligaments during knee flexion. Future studies should focus on tibiofemoral rotation to obtain further information regarding the interactions among these knee joint partners, and other TKA designs should be involved to transfer the results to more implant designs. These results support that an external rotation of the femoral component should be preferred in TKA to avoid anterior knee pain. An external trochlea rotation should be included in future TKA designs.
References
Ahmed AM, Duncan NA (2000) Correlation of patellar tracking pattern with trochlear and retropatellar surface topographies. J Biomech Eng 122:652–660
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H et al (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW (1996) Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 11:831–840
Andriacchi TP, Yoder D, Conley A, Rosenberg A, Sum J, Galante JO (1997) Patellofemoral design influences function following total knee arthroplasty. J Arthroplasty 12:243–249
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Armstrong AD, Brien HJ, Dunning CE, King GJ, Johnson JA, Chess DG (2003) Patellar position after total knee arthroplasty: influence of femoral component malposition. J Arthroplasty 18:458–465
Baldwin MA, Clary C, Maletsky LP, Rullkoetter PJ (2009) Verification of predicted specimen-specific natural and implanted patellofemoral kinematics during simulated deep knee bend. J Biomech 42:2341–2348
Baldwin MA, Clary CW, Fitzpatrick CK, Deacy JS, Maletsky LP, Rullkoetter PJ (2012) Dynamic finite element knee simulation for evaluation of knee replacement mechanics. J Biomech 45:474–483
Barink M, Van de Groes S, Verdonschot N, De Waal Malefijt M (2006) The difference in trochlear orientation between the natural knee and current prosthetic knee designs; towards a truly physiological prosthetic groove orientation. J Biomech 39:1708–1715
Barink M, Van der Mark PC, Fennis WM, Kuijs RH, Kreulen CM, Verdonschot N (2003) A three-dimensional finite element model of the polymerization process in dental restorations. Biomaterials 24:1427–1435
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B et al (2014) Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 21:272–277
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Donahue TL, Hull ML, Rashid MM, Jacobs CR (2002) A finite element model of the human knee joint for the study of tibio-femoral contact. J Biomech Eng 124:273–280
Fitzpatrick CK, Baldwin MA, Ali AA, Laz PJ, Rullkoetter PJ (2011) Comparison of patellar bone strain in the natural and implanted knee during simulated deep flexion. J Orthop Res 29:232–239
Fitzpatrick CK, Rullkoetter PJ (2012) Influence of patellofemoral articular geometry and material on mechanics of the unresurfaced patella. J Biomech 45:1909–1915
Fuchs S, Schutte G, Witte H (1999) Effect of knee joint flexion and femur rotation on retropatellar contact of the human knee joint. Biomed Tech (Berl) 44:334–338
Fuchs S, Skwara A, Tibesku CO, Rosenbaum D (2005) Retropatellar contact characteristics before and after total knee arthroplasty. Knee 12:9–12
Ghosh KM, Merican AM, Iranpour F, Deehan DJ, Amis AA (2012) Length-change patterns of the collateral ligaments after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1349–1356
Gispert MP, Serro AP, Colaco R, Saramago B (2006) Friction and wear mechanisms in hip prosthesis: comparison of joint materials behaviour in several lubricants. Wear 260:149–158
Godest AC, Beaugonin M, Haug E, Taylor M, Gregson PJ (2002) Simulation of a knee joint replacement during a gait cycle using explicit finite element analysis. J Biomech 35:267–275
Grassi A, Compagnoni R, Ferrua P, Zaffagnini S, Berruto M, Samuelsson K et al (2018) Patellar resurfacing versus patellar retention in primary total knee arthroplasty: a systematic review of overlapping meta-analyses. Knee Surg Sports Traumatol Arthrosc;10.1007/s00167-018-4831-8
Grimberg A, Jansson V, Liebs T, Melsheimer O, Steinbrück A. EPRD Jahresbericht 2016. 2017
Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, Bergmann G (2012) Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am 94:1023–1029
Halloran JP, Ackermann M, Erdemir A, van den Bogert AJ (2010) Concurrent musculoskeletal dynamics and finite element analysis predicts altered gait patterns to reduce foot tissue loading. J Biomech 43:2810–2815
Halloran JP, Petrella AJ, Rullkoetter PJ (2005) Explicit finite element modeling of total knee replacement mechanics. J Biomech 38:323–331
Hasung K, Jong-Keun S, Jong-Hwan S, Gun-Woo K, Seung-Hyun Y (2016) Total knee arthroplasty with or without patellar resurfacing with grade IV osteoarthritis in patellofemoral joint. Orthopaedic Proc 98-B:154–154
Hauf W, Mittlmeier T, Hagena FW, Plitz W (1992) [Method for in vivo measurement of intraosseous pressure of the patella]. Biomed Tech (Berl) 37:263–272
Heegaard JH, Leyvraz PF, Hovey CB (2001) A computer model to simulate patellar biomechanics following total knee replacement: the effects of femoral component alignment. Clin Biomech (Bristol Avon) 16:415–423
Hehne HJ (1990) Biomechanics of the patellofemoral joint and its clinical relevance. Clin Orthop Relat Res 258: 73–85
Keshmiri A, Maderbacher G, Baier C, Sendtner E, Schaumburger J, Zeman F et al (2015) The influence of component alignment on patellar kinematics in total knee arthroplasty. Acta Orthop 86:444–450
Kiapour A, Kiapour AM, Kaul V, Quatman CE, Wordeman SC, Hewett TE et al (2014) Finite element model of the knee for investigation of injury mechanisms: development and validation. J Biomech Eng 136:011002
Kyomoto M, Iwasaki Y, Moro T, Konno T, Miyaji F, Kawaguchi H et al (2007) High lubricious surface of cobalt-chromium-molybdenum alloy prepared by grafting poly(2-methacryloyloxyethyl phosphorylcholine). Biomaterials 28:3121–3130
Leichtle UG, Lange B, Herzog Y, Schnauffer P, Leichtle CI, Wulker N et al (2017) Influence of different patellofemoral design variations based on genesis II total knee endoprosthesis on patellofemoral pressure and kinematics. Appl Bionics Biomech 2017:5492383
Leichtle UG, Wunschel M, Leichtle CI, Muller O, Kohler P, Wulker N et al (2014) Increased patellofemoral pressure after TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 22:500–508
Lizhang J, Fisher J, Jin Z, Burton A, Williams S (2011) The effect of contact stress on cartilage friction, deformation and wear. Proc Inst Mech Eng H 225:461–475
Matsuda S, Ishinishi T, White SE, Whiteside LA (1997) Patellofemoral joint after total knee arthroplasty. Effect on contact area and contact stress. J Arthroplasty 12:790–797
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1479–1487
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Muller O, Lo J, Wunschel M, Obloh C, Wulker N (2009) Simulation of force loaded knee movement in a newly developed in vitro knee simulator. Biomed Tech (Berl) 54:142–149
Murakami AM, Hash TW, Hepinstall MS, Lyman S, Nestor BJ, Potter HG (2012) MRI evaluation of rotational alignment and synovitis in patients with pain after total knee replacement. J Bone Jt Surg Br 94:1209–1215
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Pena E, Calvo B, Martinez MA, Doblare M (2006) A three-dimensional finite element analysis of the combined behavior of ligaments and menisci in the healthy human knee joint. J Biomech 39:1686–1701
Petersen W, Rembitzki IV, Bruggemann GP, Ellermann A, Best R, Koppenburg AG et al (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Rhoads DD, Noble PC, Reuben JD, Tullos HS (1993) The effect of femoral component position on the kinematics of total knee arthroplasty. Clin Orthop Relat Res 286:122–129
Shin CS, Chaudhari AM, Andriacchi TP (2007) The influence of deceleration forces on ACL strain during single-leg landing: a simulation study. J Biomech 40:1145–1152
Slevin O, Schmid FA, Schiapparelli F, Rasch H, Hirschmann MT (2018) Increased in vivo patellofemoral loading after total knee arthroplasty in resurfaced patellae. Knee Surg Sports Traumatol Arthrosc 26:1805–1810
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2014) The effect of trochlea tilting on patellofemoral contact patterns after total knee arthroplasty: an in vitro study. Arch Orthop Trauma Surg 134:867–872
Steinbruck A, Schroder C, Woiczinski M, Fottner A, Muller PE, Jansson V (2013) Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 12:58
Stukenborg-Colsman C, Ostermeier S, Burmester O, Wirth CJ (2003) Dynamische In-vitro-Messung des retropatellaren Drucks nach alloplastischem Kniegelenkersatz. Der Orthopäde 32:319–322
Varadarajan KM, Harry RE, Johnson T, Li G Can in vitro systems capture the characteristic differences between the flexion extension kinematics of the healthy and TKA knee? Med Eng Phys 31:899–906
Victor J, Labey L, Wong P, Innocenti B, Bellemans J (2010) The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res 28:419–428
Wada K, Hamada D, Tamaki S, Higashino K, Fukui Y, Sairyo K (2017) Influence of medial collateral ligament release for internal rotation of tibia in posterior-stabilized total knee arthroplasty: a cadaveric study. J Arthroplasty 32:270–273
Werth L, Saffarini M, Amsler F, Abdelkafy A, Hirschmann MT (2017) The need for secondary resurfacing is affected by trochlear height in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3818–3823
Woiczinski M, Steinbruck A, Weber P, Muller PE, Jansson V, Schroder C (2016) Development and validation of a weight-bearing finite element model for total knee replacement. Comput Methods Biomech Biomed Engin 19:1033–1045
Woiczinski M, Tollrian C, Schroder C, Steinbruck A, Muller PE, Jansson V (2013) Calculation of the elastic properties of prosthetic knee components with an iterative finite element-based modal analysis: quantitative comparison of different measuring techniques. Biomed Tech (Berl) 58:369–376
Zelle J, Heesterbeek PJ, De Waal Malefijt M, Verdonschot N (2010) Numerical analysis of variations in posterior cruciate ligament properties and balancing techniques on total knee arthroplasty loading. Med Eng Phys 32:700–707
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The ethics committee of the University of Munich verified the study design as being in accordance with the international ethical principles for medical research and approved this study (Number 58–16). The study have been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Woiczinski, M., Kistler, M., Schröder, C. et al. TKA design-integrated trochlea groove rotation reduces patellofemoral pressure. Knee Surg Sports Traumatol Arthrosc 27, 1680–1692 (2019). https://doi.org/10.1007/s00167-018-5324-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5324-5