Abstract
Purpose
The influence of different implantation techniques in TKA on tibiofemoral kinematics was analysed in few investigations so far. However, the influence on patellar kinematics remain unclear. The aim of the present investigation was to compare patellar kinematics of the natural knee with those of knees after both kinematically and mechanically aligned TKAs.
Methods
Patellar kinematics of ten cadaveric knees before and after TKAs implanted using both a kinematic and mechanic alignment technique were investigated and compared using a commercial optical computer navigation system.
Results
There was a statistically significant difference between natural patellar kinematics and both implantation techniques analysing mediolateral shift. Patellar lateral tilt showed significant better results in the kinematically compared to the mechanically aligned TKAs. In terms of patella rotation, the patella of both mechanically and kinematically aligned TKAs showed significant higher values for external rotation compared to the natural knee. Regarding epicondylar distance again a significant better restoration of natural kinematics could be found in the kinematically aligned TKAs.
Conclusion
Kinematically aligned TKAs showed a better overall restoration of patellar kinematics compared to a conventional mechanical alignment technique. In terms of clinical usefulness, the present study highlights the potential benefit for clinical outcome using a kinematically aligned implantation technique in TKA to achieve a better restoration of natural patellofemoral kinematics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative anterior knee pain is one of the remaining major problems after total knee arthroplasty (TKA). Recent cadaveric and biomechanical investigations attributed anterior knee pain and patellar maltracking mainly to femoral and tibial component malalignment [2, 3, 11]. Furthermore, influence of different implant design on tibiofemoral kinematics and the appearance of anterior knee pain was demonstrated in recent investigations [13, 18,19,20]. Different implant radii seem to have a great influence on tibiofemoral kinematics, femoral rollback and mean displacement of tibiofemoral contact [5, 17]. Additionally, a significant correlation of bone tracer uptake of the patella and coronal TKA alignment was found in a SPECT/CT investigation by Slevin et al. [15]. Very little is known about the difference in tibiofemoral kinematics using a mechanical or a kinematical implantation technique [14, 16]. Apart from that, no studies evaluating the difference in choosing one of both techniques with regards to patellofemoral kinematics could be found. The aim of this investigation was to compare patellar kinematics in the natural knee and in TKAs implanted using a kinematic or a conventional mechanic alignment technique. We hypothesised that using a kinematical implantation technique in TKA will result in a better restoration of natural patellar kinematics compared to a mechanical implantation technique.
Materials and methods
According to our local ethical committee at the Medical University of Regensburg/Germany, IRB approval was not necessary.
Lower limbs of ten Thiel-embalmed whole-body specimens were used for this investigation. Evaluated by an initial lower limb CT scan and the specimen’s history, none of the knees had an arthritic deterioration more than grade 1 or 2 according to Outerbridge [12], a varus or valgus deviation more than 3° nor any dysplasia or any history of surgery or injury. Patellar kinematics (mediolateral shift (mm), medial: +/lateral: −; axial tilt (°), medial: −/lateral: +; rotation (°), medial: +/lateral: −; epicondylar distance (mm): distance between patella and anatomical transepicondylar axis) were investigated using a commercial optical computer navigation system (Knee Patella Tracking Software, BrainLAB; Feldkirchen, Germany) before and after standard fixed-bearing, CR-TKA, implanted in kinematical and mechanical alignment technique. According to previous publications [8, 9] a coordinate system for the knee published by Grood and Suntay was used for calculation [6].
Surgical procedure
After performing a standard medial parapatellar approach the joint capsule of each knee was marked at four defined locations with a waterproof pen (3 cm proximal to the superior patellar tip, at the medial proximal patellar edge, centrally at the medial patellar edge and at the medial distal patellar edge) to ensure subsequent anatomic closure. The reference arrays for the navigation system were attached to the proximal tibia and to the distal femur. The femoral array was attached through an additional 1 cm incision to avoid soft tissue tension while performing the motion cycle. Subsequently the different landmarks according to the navigation protocol were recorded to define the femoral and tibial coordinate system. Afterwards, femorotibial kinematics were measured by means of the navigation system. The line connecting the middle of the posterior cruciate ligament to the medial edge of the patellar tendon onset (tibial tubercle) was defined as the tibial a.p. axis according to Akagi [1]. The patella array (BrainLAB; Feldkirchen, Germany) was fixed to the anterior side of the patella with a small screw as recommended by the manufacturer. The most medial, superior and inferior edge and the most prominent point at the posterior articular ridge of the patella were registered to additionally define the patellar coordinate system. After anatomical closure of the joint capsule at the prior defined locations, the natural patellar kinematics and the relative orientation between femur, tibia and patella were recorded; the lower extremity was placed free onto a continuous passive motion machine in a straight position without muscle load to simulate intraoperative conditions. Three motion cycles were performed while patellar kinematics were measured every 10° between 10° and 90° of flexion. Subsequently, the measurement of patellar kinematics was repeated after implanting the cruciate-ligament retaining trial prosthesis (PFC Sigma, cruciate retaining, fixed bearing inlay; DePuy, Warsaw, IN, USA) using a kinematical and consecutive a mechanical alignment technique fixing the components with pins and screws. For kinematically aligned TKAs, 9 mm from the medial and lateral distal femur was resected according to the thickness of the femoral component by means of the navigation system. The four-in-one cutting block was attached parallel to the posterior condylar line resulting in an equal medial and lateral posterior resection of 9 mm. At the proximal tibia 8 mm medial and lateral was resected in accordance to the tibial component thickness. The rotational alignment of the tibial tray was set to the above mentioned Akagi-line. No ligament release or any patella intervention was performed. The accuracy of the desired position of the femoral and tibial component was verified using the navigation system and adapted, if required. After anatomical capsule closure, patellar kinematics were registered.
The same procedure was performed using a mechanical alignment technique cutting both the tibia and the distal femur perpendicular to the mechanical axis, resecting the minimum amount of bone possible preserving the initial tibial slope. The rotation of the four-in-one cutting block was set to 3° of external rotation in relation to the posterior condylar line by means of the navigation system. Again, patellar kinematics were recorded after anatomical closure at the initially defined marks.
Statistical analysis
Mean and standard deviation of patellar kinematic parameters (shift, tilt, rotation, epicondylar distance) were calculated at nine positions between 10° and 90° of flexion in 10° steps. To compare patellar kinematics before and after TKA (kinematically and mechanically aligned, respectively), a paired t-test was used. Power analysis was done post hoc for paired samples using the standard deviation (SD) of the difference between compared groups. All values are reported for a power of 0.90. A two-sided p value of ≤ 0.05 was considered statistically significant. Statistical analyses were performed with IBM SPSS Statistics v22.0.
Results
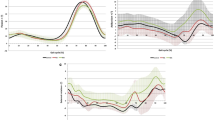
Mediolateral shift
The natural knees as well as both types of implantation techniques showed a constant increase of medial patellar shift from 20° to 90° of flexion. There was a statistically significant difference between natural patellar kinematics and both implantation techniques over the whole range of motion (Fig. 1; Table 1).
Tilt
Statistically significant differences were found compared to the natural knees from 40° to 90° of flexion in the kinematically aligned and from 10° to 90° of flexion in the mechanically aligned TKAs (Fig. 2; Table 1).
Rotation
The kinematically aligned TKAs showed a statistically significant difference from 40° to 90° of flexion compared to the natural knees while the mechanically aligned TKAs showed significant different values from 30° to 90° of flexion compared to the natural knees (Fig. 3; Table 1).
Epicondylar distance
A statistically significant difference between the natural knees and knees after kinematically aligned TKAs at 10° of flexion could be found, while statistically significant differences between the natural knees and mechanically aligned TKAs occurred from 10° to 70° of flexion (Fig. 4; Table 1).
Discussion
The most important finding of the present investigation was that a significant difference in patellofemoral kinematics between both alignment techniques in TKA the controversial discussed kinematical and the conventional mechanical alignment was found. Furthermore, a better overall restoration of natural patellar kinematics could be found in the kinematically aligned compared to the mechanically aligned TKAs.
In a radiological investigation Zhang et al. demonstrated a relation between tibiofemoral rollback and patellofemoral kinematics [21]. As the tibiofemoral joint rotated, the patellofemoral joint became more stable and aligned. We can confirm these findings thus the kinematical aligned TKA presented a better overall restoration of preoperative patellar kinematics compared to the conventional mechanic alignment technique. In both kinematical and mechanical aligned TKAs, no significant difference in any measured flexion angle regarding mediolateral patellar shift compared to the natural preoperative knee could be found. Interestingly, the patella shifted more medially in the kinematically aligned TKAs. This result does not support the findings of Brar et al. of a more laterally driven patella and later engagement in the femoral component groove in kinematically aligned TKAs [4]. However, our findings could indicate a medialization of the patella due to a more medialized trochlea groove using a standard implant for kinematically aligned implantation. Thus, restoration of natural patellofemoral kinematics could benefit from a more oblique lateralized trochlea groove implant design to allow a natural patella engagement using a kinematical alignment technique. Analysing patellar tilt, the kinematically aligned TKAs showed no significant difference compared to the natural knees from 10° to 30° of flexion while the mechanically aligned TKAs showed a significant difference from 10° to 90° of flexion. The better restoration from 10° to 30° of flexion suggest again less tension on the lateral aspect of the patellofemoral joint as well as missing ventro-distal overstuffing in kinematically aligned TKAs. Regarding patellar rotation, a better restoration of natural kinematics could be demonstrated by kinematically aligned TKAs. However, both alignment techniques showed a statistically significant difference compared to the natural knees.
A greater femoral rollback and more external rotation of the femoral component was observed in kinematically aligned TKA compared to a conventional mechanically aligned TKA by Ishikawa et al. using a musculoskeletal computer model [7]. However, they also found increased patellofemoral and tibiofemoral contact stress forces in kinematically aligned compared to mechanically aligned TKA. In the present investigation the kinematically aligned TKAs showed a nearly preoperative situation regarding the epicondylar distance. As we value the epicondylar distance as an indirect parameter for pressure of the patellofemoral joint, we cannot confirm these findings. Additionally, we found a significant difference in epicondylar distance between the natural knees and knees after mechanically aligned TKAs. This effect could be ascribed to a ventro-distal overstuffing of the lateral femoral condyle in mechanically aligned TKAs.
There is no literature so far analysing patellar kinematic parameters using different alignment techniques to compare. However, in the present investigation especially epicondylar distance and lateral tilt behavior reflect our concern of lateral over tension and overstuffing by a too prominent lateral femoral condyle while performing a TKA using a conventional implant design and a mechanical alignment technique.
This study bears a considerable number of limitations. First of all, patellar kinematics were measured without muscle force and through passive range of motion on a passive motion machine, reflecting intraoperative conditions. However, the data was collected using cadaveric knees still attached to the torso. Moreover, Masri and McCormack reported in a radiological investigation, that quadriceps contraction does not alter the congruence angles obtained in 30° and 45° axial views [10]. The goal of the present investigation was to simulate intraoperative conditions to correlate data with clinical outcome parameters in future investigations.
Furthermore, in the natural knee, reference points on the patella need to be registered after arthrotomy. Hence, patellar tracking of the natural knee was measured after anatomical closure of the capsule. Defined marks were set to achieve same tensionless anatomical closure for patellar tracking before and after TKA implantations and measurements were performed under same conditions. The closure and reopening of the arthrotomy as well as the motion cycle on the passive motion machine was conducted with great care, due to possible deterioration of the capsule. However, differences in patellar kinematic values in between measurement cycles also might have occurred due to this procedure. Furthermore, the usage of TKA components from one manufacturer might have produced unique patellar kinematics, not generally transferable to knees resurfaced with other implants.
In terms of clinical relevance, the present study highlights the benefit of using a kinematical alignment technique in TKA regarding the restoration of natural patellofemoral kinematics. Thus, more surgeons should consider to use this technique in daily routine.
Conclusion
Kinematical alignment in TKA showed a better restoration with regards to natural patellar kinematics compared to conventional mechanical alignment and is therefore the superior implantation technique with regards to patellar tracking. Still, significant difference was shown in both implantation techniques in comparison to the natural knee, respectively, possibly demonstrating that alteration of patellar tracking in TKA might be a cause for postoperative anterior knee pain. Further clinical investigations are necessary to confirm and correlate these findings with clinical outcome parameters.
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Barrack RL, Schrader T, Bertot AJ et al (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Belvedere C, Catani F, Ensini A et al (2007) Patellar tracking during total knee arthroplasty: an in vitro feasibility study. Knee Surg Sports Traumatol Arthrosc 15:985–993
Brar AS, Howell SM, Hull ML, Mahfouz MR (2016) Does kinematic alignment and flexion of a femoral component designed for mechanical alignment reduce the proximal and lateral reach of the trochlea? J Arthroplast 31(8):1808–1813
Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ (2013) The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46(7):1351–1357
Grood SE, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application for the knee. J Biomech Eng 105:136–144
Ishikawa M, Kuriyama S, Ito H, Furu M, Nakamura S, Matsuda S (2015) Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee 22(3):206–212
Keshmiri A, Maderbacher G, Baier C, Zeman F, Grifka J, Springorum HR (2016) Significant influence of rotational limb alignment parameters on patellar kinematics: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(8):2407–2414
Keshmiri A, Springorum HR, Baier C, Zeman F, Grifka J, Maderbacher G (2016) Changes in sagittal component alignment alters patellar kinematics in TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24(3):823–829
Masri BA, McCormack RG (1995) The effect of knee flexion and quadriceps contraction on the axial view of the patella. Clin J Sport Med 5(1):9–17
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92-B:1238–1244
Outerbridge Re (1961) The etiology of chondromalacia patellae. J Bone Joint Surg Br 43-B:752–757
Pejhan S, Bohm E, Brandt JM, Wyss U (2017) The influence of geometric design variables on the kinematic performance of a surface-guided total knee replacement. J Orthop Surg (Hong Kong) 25(3):2309499017727922
Rivière C, Iranpour F, Harris S, Auvinet E, Aframian A, Parratte S, Cobb J (2018) Differences in trochlear parameters between native and prosthetic kinematically or mechanically aligned knees. Orthop Traumatol Surg Res 104(2):165–170
Slevin O, Schmid FA, Schiapparelli FF, Rasch H, Amsler F, Hirschmann MT (2017) Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(11):3605–3610
Takahashi T, Ansari J, Pandit HG (2018) Kinematically aligned total knee arthroplasty or mechanically aligned total knee arthroplasty. J Knee Surg 31:999–1006
Wang H, Simpson KJ, Chamnongkich S, Kinsey T, Mahoney OM (2008) Biomechanical influence of TKA designs with varying radii on bilateral TKA patients during sit-to-stand. Dyn Med 13(7):12
Werth L, Saffarini M, Amsler F, Abdelkafy A, Hirschmann MT (2017) The need for secondary resurfacing is affected by trochlear height in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25(12):3818–3823
Xie X, Rusly R, DesJardins JD, Voss F, Chillag K, LaBerge M (2017) Effect of rotational prosthetic alignment variation on tibiofemoral contact pressure distribution and joint kinematics in total knee replacement. Proc Inst Mech Eng Part H 231(11):1034–1047
Zeller IM, Sharma A, Kurtz WB, Anderle MR, Komistek RD (2017) Customized versus patient-sized cruciate-retaining total knee arthroplasty: an in vivo kinematics study using mobile fluoroscopy. J Arthroplast 32(4):1344–1350
Zhang LK, Wang XM, Niu YZ, Liu HX, Wang F (2016) Relationship between patellar tracking and the “screw-home” mechanism of tibiofemoral joint. Orthop Surg 8(4):490–495
Acknowledgements
We would like to thank Depuy, Germany and Brainlab, Germany for their technical and logistical support for this study. Furthermore, we would like to thank the Institute of Anatomy at the Medical University of Graz/Austria to provide the specimen for this investigation.
Funding
For this study no external funding was used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest regarding the submitted article.
Ethical approval
According to the local ethical committee at the Medical University of Regensburg/Germany, IRB approval was not necessary.
Rights and permissions
About this article
Cite this article
Keshmiri, A., Maderbacher, G., Baier, C. et al. Kinematic alignment in total knee arthroplasty leads to a better restoration of patellar kinematics compared to mechanic alignment. Knee Surg Sports Traumatol Arthrosc 27, 1529–1534 (2019). https://doi.org/10.1007/s00167-018-5284-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5284-9