Abstract
Purpose
As patellar tracking and loading is influenced by tibial tuberosity and trochlear groove (TT–TG) distance, patellar height, thickness and tilt as well as TKA component position, it was our hypothesis that these parameters significantly correlate with patellar BTU intensity and localization in SPECT/CT. The purpose of the study was to investigate whether TKA component position as well as the height, thickness and tilt of the unresurfaced patella influences the intensity and the distribution pattern of BTU in SPECT/CT.
Methods
A total of 62 consecutive patients who underwent primary TKA without patellar resurfacing were prospectively included. Demographic data such as age, gender, side and type of primary TKA were noted. All patients underwent clinical and radiological examination in a specialized knee clinic, including standardized radiographs (anterior–posterior and lateral weight bearing, patellar skyline view) and Tc-99m-HDP-SPECT/CT before, 12 and 24 months after TKA. SPECT/CT images were analysed on 3D reconstructed images. Rotational, sagittal and coronal position of the tibial and femoral TKA components was assessed using a previously validated analysis software. Measurements of BTU including intensity and anatomical distribution pattern were also performed from 3D data. The patellar height, thickness and tilt were measured, and the distance between TT and TG was measured using axial CT images. Univariate analysis was performed to identify any correlations between BTU and TKA component position and patellar measurements (p < 0.05).
Results
The highest median BTU was measured in the superior posterior parts of the patella. A statistically significant correlation was found between valgus alignment of the femoral TKA and increased BTU at the lateral patellar regions (p < 0.05). External rotation of the tibial TKA correlated with increased BTU at the lateral superior joint adjacent part (p < 0.05). No correlation was found between the tibial TKA position (varus–valgus, anterior and posterior slope), TT–TG distance, patellar height and patellar BTU values.
Conclusions
A significant correlation of increased patellar BTU was found with femoral valgus TKA alignment. These findings highlight the importance of femoral TKA position in coronal plane with regard to post-operative patellar tracking. Moreover, these facts might explain anterior knee pain in unhappy TKA with femoral valgus alignment.
Level of evidence
Diagnostic study, Level II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patellofemoral joint complications are a major and frequent cause for revision surgery after total knee arthroplasty (TKA) [9, 20, 21, 23]. In TKA with or without primary patellar resurfacing, the number of patients with patellofemoral problems appears to be comparably high [4, 22, 25]. The patients typically complain about persistent or new onset of anterior knee pain [19]. In patients with unresurfaced patella, patellar maltracking, patellofemoral overloading and progression of patellofemoral osteoarthritis (OA) are common pain generators [23].
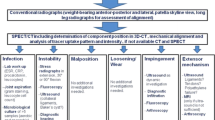
Radionucleotide imaging such as bone scintigraphy (bone scan) has been used to obtain more functional loading information of the patellofemoral joint and assess overloading due to patellar maltracking [11, 20, 32]. The hot patella sign has been controversially discussed [6]. Recent studies demonstrated a clear correlation between increased bone tracer uptake (BTU) and anterior knee pain after TKA. Possible explanations of increased patellar BTU are an increased in vivo loading at the patellofemoral joint and subsequent bone remodelling. Moreover, patients with a hot patella who underwent secondary patellar resurfacing reported a significant symptomatic relief [1]. Some authors even recommended the use of bone scans as a screening tool for diagnosis of patellar-related problems [1]. However, the main drawback of bone scans is their poor ability to localize the increased BTU [28].
Hybrid SPECT/CT, which combines the strengths of 3D bone scan (SPECT) and CT, has been highlighted as an important tool for evaluating patients after TKA [2, 7, 10, 12,13,14,15,16]. In these studies, SPECT/CT was particularly helpful in identifying patellofemoral problems such as maltracking, overloading or progression of osteoarthritis [15]. It is the combined assessment of mechanical, structural and functional information, which offers a richer source for establishment of the correct diagnosis [6, 8, 15]. As patellar tracking and loading of the patella are influenced by TT–TG distance, patellar height, thickness and tilt as well as TKA component position, it was our hypothesis that these parameters significantly correlate with patellar BTU intensity and localization in SPECT/CT.
The purpose of the study was to investigate whether aforementioned patellar criteria, mechanical alignment and TKA component position influence the intensity and the BTU distribution pattern of the unresurfaced patella after TKA. This is the first study assessing in vivo loading of the patella using SPECT/CT.
Materials and methods
A total of 64 knees of 62 consecutive patients (mean age ± standard deviation 66 ± 11, range 23–87 years, male-to-female ratio 31:31) who underwent primary TKA without patellar resurfacing between 2011 and 2013 were prospectively included. All patients underwent clinical and radiological examination in a specialized knee clinic, including standardized radiographs (anterior–posterior and lateral weight bearing, patellar skyline view) and Tc-99m-HDP-SPECT/CT before, 12 and 24 months after TKA. Demographic data such as age, gender, side and type of primary TKA were noted.
Tc-99m-HDP-SPECT/CT was performed using a hybrid system (Symbia T16, Siemens, Erlangen, Germany) which consists of a pair of low-energy, high-resolution collimators and a dual-head gamma camera and an integrated 16 × 0.75 mm slice thickness CT. All patients received a commercial 500–700 MBq Tc-99m-HDP injection (CIS Bio International Sur Yvette, France). Planar scintigraphic images were taken in the perfusion phase (immediately after injection), the soft tissue phase (1–5 min after injection) and the delayed metabolic phase (2 h after injection). SPECT/CT was performed with a matrix size of 128 × 128, an angle step of 32 and a time per frame of 25 s 2 h after injection.
SPECT/CT images were analysed on 3D reconstructed images. Rotational (internal–external rotation), sagittal (flexion–extension, anterior–posterior slope) and coronal (varus–valgus) position of the tibial and femoral TKA components was assessed using a customized analysis software (OrthoExpert©, London, UK) [26].
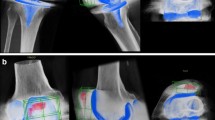
Measurements of BTU including intensity and anatomical distribution pattern were also performed from 3D data [26]. BTU intensity was measured in 3D for each anatomical area, as reflected by a previously validated localization scheme [14]. The localization scheme equally divides the patella into eight different areas to accurately map the BTU activity (Fig. 1). Maximum intensity values were recorded, and ratios between the respective value in the measured area and the background BTU (proximal midshaft of the femur) were calculated.
3D SPECT/CT tracer uptake analysis in the coronal, sagittal and axial planes using a customized software (OrthoExpert©, London, UK). The quantification of the maximum, minimum and mean uptake values was done in eight different anatomical areas of the patella. The patellar grid in those images of a 73-year-old woman 14 months after CR unresurfaced TKA shows significantly higher uptake in the superior–lateral patellar area
The patellar height, according to the modified Insall–Salvati index and the Caton–Deschamps index, and the patella thickness were measured using lateral knee radiographs in 30° flexion [8, 24]. The patellar tilt was measured in a “skyline view” using the Sasaki index [27]. The distance between the tibial tuberosity and the trochlear groove (TT–TG) was measured using axial images from the CT scan [5].
Ethical approval was obtained from the Ethics Committee of Northwestern and Central Switzerland (EKNZ 2016-01890). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Statistical analysis
All data were analysed by an independent professional statistician using IBM SPSS Statistics for Windows, version 24.0 (Armonk, NY: IBM Corp, USA). Continuous variables were described using means with standard deviations and medians with ranges. All statistical analysis was carried out non-parametrically: To compare KSS before and after operation, Wilcoxon signed-rank tests were performed and Spearman rho was calculated to identify any correlations between BTU and TKA component position and patellar measurements (p < 0.05). A post hoc analysis using G*Power, version 3.1.9 (University of Kiel, Germany) showed that with the given N = 64 and a two-tailed alpha <0.05, correlations of r > 0.35 could be found with a power of 80%.
Results
The mean TKA alignment measurements and the patellar thickness, height and the TT–TG distance in the investigated population are shown in Table 1. The mean KSS score significantly improved from 125 ± 27 preoperatively to 184 ± 19 post-operatively (Table 2). The highest mean BTU was measured in the superior and joint adjacent parts of the patella. The second highest BTU was found in the inferior joint adjacent patellar parts. The anterior patellar areas were lower than the joint adjacent areas. The lowest BTU was found in the inferior anterior patellar area (Table 3). A significant correlation was found between valgus alignment of the femoral TKA and increased BTU in the lateral patellar areas (p < 0.05). In addition, a valgus-aligned femoral TKA component correlated with increased medial BTU, although this observation did not reach statistical significance (Table 4). External rotation of the tibial TKA component correlated with increased BTU in the articular lateral superior patellar parts. No correlation was found between the position of the tibial TKA component in the coronal or sagittal plane. There was also no significant correlation between patellar thickness and TT–TG distance to increased BTU at the patella.
Discussion
The most important findings of the present study were as follows: Firstly, valgus alignment of the femoral TKA component was significantly correlated with increased BTU in the patella, in particular the lateral patellar areas. This finding clearly indicates that TKA position in the coronal plane influences in vivo loading of the patella in patients after TKA, a fact which is to date underreported. It appears that knee surgeons focus more on the influence of rotational and sagittal TKA alignment on patellar tracking. It is well established that internal rotation of the femoral TKA leads to increased stress of the lateral patellar facet, which is due to an increased Q-angle and lateral patellofemoral tracking [3, 21]. In the present study, it was found that with more valgus in the femoral component BTU increased in all patellar areas, but particularly in the lateral patellar areas. One explanation could be that femoral TKA valgus alignment results in increased laterally directed forces, which in its maximum extent tend to sublux the patella laterally [21]. Another explanation might be the fact that the contact zone of patella and trochlea changes in valgus-aligned femoral TKA. The trochlear geometry might also play a role here.
It is also a well established fact that flexion of the femoral TKA component increases the patellofemoral pressure and leads to a “pseudo” patella baja. Here an increase in the stress at the superior patellar areas was found [23]. Furthermore, a recent study in native knees has shown that a patella baja correlates with increased BTU in all patellar areas. In addition, a higher patellofemoral tilt angle led to increased BTU in the inferior and superior patellar areas [29]. Another effect of the sagittal component alignment on the patellar kinematics was recently reported in the cadaveric study by Keshmiri et al. [17], as femoral component aligned in 5° of flexion significantly altered patellar mediolateral shift. However, in the present study no correlation between sagittal TKA alignment and BTU in any patellar area was found. There was also no evidence that a patella baja led to more loading of any patellar areas. This is in clear contrast to a biomechanical study by Singerman et al. [30]. Secondly, a specific BTU pattern in patients after TKA with unresurfaced patellae was identified and described in detail. There were significant BTU differences between the patella areas in SPECT/CT. As previously shown, BTU represents the in vivo loading of the tibiofemoral and patellofemoral joint [29]. To date, the normal and pathological BTU pattern after TKA is unknown. In the last 20 years, the discussion with regard to this topic was limited to the question whether a hot patella is a clinically relevant finding in patients after TKA. Some authors stated that the hot patella sign is an important abnormal finding indicating overloading of the patellofemoral joint. Others did not see any clinical value in reporting a hot patella sign as it includes both the normal remodelling of an unresurfaced patella and abnormal loading of the patella.
In a recent retrospective study, Ahmad et al. [1] found a significant correlation between the “hot patella” sign and post-operative patellofemoral problems in 55 symptomatic patients after TKA. In this study, patients underwent bone scans. The authors concluded that patients with a “hot patella” sign are more likely to benefit from a secondary patellar resurfacing. However, this study was done on 2D and the present study used 3D data. Our group has shown in many previous publications that 3D data should be used to open a more realistic and detailed window into the bone homoeostasis [11, 12, 16, 26, 31]. The “hot patella” sign, which is defined as greater BTU in the patella than in the ipsilateral distal femur or the proximal tibia [18], is a rather rough and broad assessment of patella BTU. Based on our data, the “hot patella” sign is not useful for assessment of patellar loading. However, when the patellar bone is divided into several different areas, BTU evaluation in 3D might be helpful for guidance of treatment. In a similar way to the “hot patella” concept, Awengen et al. [2] found significantly higher BTU intensity in symptomatic TKA in all the different anatomical regions in the patella using SPECT/CT. The SPECT/CT algorithm presented here localizes and quantifies patellar BTU in eight different areas of interest. In future, analysis of patellar BTU after TKA might be beneficial in establishing more differential diagnoses and possible reasons for anterior knee pain following TKA. This algorithm might then also guide further treatment in unhappy patients after TKA [16].
The present study bears a considerable number of limitations. This was a prospective series of TKA in a teaching hospital setting. Hence, a team of different surgeons operated on a consecutive series of patients. In addition, the patients investigated were not specifically evaluated for anterior knee pain, which would allow to differentiate between normal and abnormal BTU pattern in symptomatic and asymptomatic patients after TKA. In this study, this was only done based on KSS, which is not a patellofemoral-specific outcome instrument. Furthermore, increased patellar BTU might not only be due to the factors investigated, but also due to other reasons such as residual patellar osteoarthritis.
Conclusion
The strongest correlation of increased patellar BTU was found with a femoral TKA in valgus orientation. These findings highlight the clinical importance of femoral TKA position in the coronal plane with regard to post-operative patellar tracking. In unhappy TKA with anterior knee pain, these facts should be carefully considered.
References
Ahmad R, Senthil Kumar G, Katam K, Dunlop D, Pozo JL (2009) Significance of a “hot patella” in total knee replacement without primary patellar resurfacing. Knee 16:337–340
Awengen R, Rasch H, Amsler F, Hirschmann MT (2016) Symptomatic versus asymptomatic knees after bilateral total knee arthroplasty: what is the difference in SPECT/CT? Eur J Nucl Med Mol Imaging 43:762–772
Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A (2014) Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 21:272–277
Burnett RS, Haydon Christopher M, Rorabeck CH, Bourne RB (2004) The John Insall award: patella resurfacing versus nonresurfacing in total knee arthroplasty: results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res 18:12–25
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Fogelman I, Mckillop JH (1983) The “Hot Patella” sign: is it of any clinical significance? Concise communication. J Nucl Med 24:312–316
Forrer F, Hirschmann MT, Rasch HF (2014) July) SPECT/CT for the assessment of painful knee prosthesis. Nucl Med Commun 35(7):782
Grelsamer RP, Meadows S (1992) The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Relat Res 282:170–176
Heyse TJ, Figiel J, Hähnlein U, Timmesfeld N, Schofer MD, Fuchs-Winkelmann S, Efe T (2013) MRI after patellofemoral replacement: the Component-bone interface and rotational alignment. HSS J 9:108–112
Hirschmann MT, Amsler F, Rasch H (2015) Clinical value of SPECT/CT in the painful total knee arthroplasty (TKA): a prospective study in a consecutive series of 100 TKA. Eur J Nucl Med Mol Imaging 42:1869–1882
Hirschmann MT, Davda K, Iranpour F, Rasch H, Friederich NF (2011) Combined single photon emission computerised tomography and conventional computerised tomography (SPECT/CT) in patellofemoral disorders: a clinical review. Int Orthop 35:675–680
Hirschmann MT, Henckel J, Rasch H (2013) SPECT/CT in patients with painful knee arthroplasty-what is the evidence? Skeletal Radiol 42:1201–1207
Hirschmann MT, Iranpour F, Davda K, Rasch H, Hügli R, Friederich NF (2010) Combined single-photon emission computerized tomography and conventional computerized tomography (SPECT/CT): clinical value for the knee surgeons? Knee Surg Sports Traumatol Arthrosc 18:341–345
Hirschmann MT, Iranpour F, Konala P, Kerner A, Rasch H, Cobb JP, Friederich NF (2010) A novel standardized algorithm for evaluating patients with painful total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography. Knee Surg Sports Traumatol Arthrosc 18:939–944
Hirschmann MT, Konala P, Iranpour F, Kerner A, Rasch H, Friederich NF (2011) Clinical value of SPECT/CT for evaluation of patients with painful knees after total knee arthroplasty—a new dimension of diagnostics? BMC Musculoskelet Disord 12:36
Hirschmann MT, Wagner CR, Rasch H, Henckel J (2012) Standardized volumetric 3D-analysis of SPECT/CT imaging in orthopaedics: overcoming the limitations of qualitative 2D analysis. BMC Med Imaging 12(1):5
Keshmiri A, Springorum HR, Baier C, Zeman F, Grifka J, Maderbacher G (2016) Changes in sagittal component alignment alters patellar kinematics in TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 24:823–829
Kipper MS, Alazraki NP, Feiglin DH (1982) The “hot” patella. Clin Nucl Med 7:28–32
Li S, Chen Y, Su W, Zhao J, He S, Luo X (2011) Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop 35:305–316
Lorberboym M, Ben Ami D, Zin D, Nikolov G, Adar E (2003) Incremental diagnostic value of 99mTc methylene diphosphonate bone SPECT in patients with patellofemoral pain disorders. Nucl Med Commun 24:403–410
Malo M, Vince KG (2003) The unstable patella after total knee arthroplasty: etiology, prevention, and management. J Am Acad Orthop Surg 11:364–371
Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E (2011) Patellar resurfacing in total knee arthroplasty: does design matter?: a meta-analysis of 7075 cases. J Bone Joint Surg Am 93:1301–1309
Petersen W, Rembitzki IV, Brüggemann G-P, Ellermann A, Best R, Koppenburg AG-, Liebau C (2014) Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 38:319–328
Phillips CL, Silver DA, Schranz PJ, Mandalia V (2010) The measurement of patellar height: a review of the methods of imaging. J Bone Joint Surg Br 92:1045–1053
Pilling RWD, Moulder E, Allgar V, Messner J, Mohsen A (2012) Patellar resurfacing in primary total knee replacement. J Bone Joint Surg Am 94:2270–2278
Rasch H, Falkowski AL, Forrer F, Henckel J, Hirschmann MT (2013) 4D-SPECT/CT in orthopaedics: a new method of combined quantitative volumetric 3D analysis of SPECT/CT tracer uptake and component position measurements in patients after total knee arthroplasty. Skelet Radiol 42:1215–1223
Sasaki T, Yagi T (1986) Subluxation of the patella. Investigation by computerized tomography. Int Orthop 10:115–120
Schillaci O, Danieli R, Manni C, Simonetti G (2004) Is SPECT/CT with a hybrid camera useful to improve scintigraphic imaging interpretation? Nucl Med Commun 25:705–710
Schön SN, Afifi FK, Rasch H, Amsler F, Friederich NF, Arnold MP, Hirschmann MT (2014) Assessment of in vivo loading history of the patellofemoral joint: a study combining patellar position, tilt, alignment and bone SPECT/CT. Knee Surg Sports Traumatol Arthrosc 22:3039–3046
Singerman R, Davy DT, Goldberg VM (1994) Effects of patella alta and patella infera on patellofemoral contact forces. J Biomech 27:1059–1065
Slevin O, Amsler F, Hirschmann MT (2017) No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4400-y
Smith SL, Wastie ML, Forster I (2001) Radionuclide Bone Scintigraphy in the Detection of Significant Complications after Total Knee Joint Replacement. Clin Radiol 56:221–224
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
There was no financial conflict of interest with regards to this study.
Ethical approval
Ethical approval was obtained from the Ethikkommission Nordwest- und Zentralschweiz (EKNZ, Basel). All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Slevin, O., Schmid, F.A., Schiapparelli, FF. et al. Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 3605–3610 (2017). https://doi.org/10.1007/s00167-017-4627-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4627-2