Abstract
Purpose
The acromioclavicular ligament complex (ACLC) is the primary stabilizer against horizontal translation with the superior ACLC providing the main contribution. The purpose of this study was to evaluate the specific regional contributions in the superior half of ACLC, where the surgeon can easily access and repair or reconstruct, for posterior translational and rotational stability.
Methods
The superior half of ACLC was divided into three regions; Region A (0°–60°): an anterior 1/3 region of the superior half of ACLC, Region B (60°–120°): a superior 1/3 region of the superior half of ACLC, and Region C (120°–180°): a posterior 1/3 region of the superior half of ACLC. Fifteen fresh-frozen cadaveric shoulders were used. Biomechanical testing was performed to evaluate the resistance force against passive posterior translation (10 mm) and the resistance torque against passive posterior rotation (20°) during the following the four conditions. (1) Stability was tested on all specimens in their intact condition (n = 15). (2) The ACLC was dissected and stability was tested (n = 15). (3) Specimens were randomly divided into three groups by regions of suturing. Stability was tested after suturing Region A, Region B, or Region C (n = 5 per group). (4) Stability was tested after suturing additional regions: Region A + B (0°–120°), Region B + C (60°–180°), or Region A + C (0°–60°, 120°–180°, n = 5 per group).
Results
The translational force increased after suturing Region A when compared with dissected ACLC (P = 0.025). The force after suturing Region A + B was significantly higher compared to the dissected ACLC (P < 0.001). The rotational torque increased after suturing Region A or Region B compared with dissected ACLC (P = 0.020, P = 0.045, respectively). The torque after suturing the Region A + C was significantly higher compared to the dissected ACLC (P < 0.001).
Conclusion
The combined Region A + B contributed more to posterior translational stability than Region B + C or Region A + C. In contrast, combined Region A + C contributed more to posterior rotational stability than Region A + B or Region B + C. Based on these findings, surgical techniques restoring the entire superior ACLC are recommended to address both posterior translational and rotational stability of the AC joint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The best surgical procedure for acromioclavicular (AC) joint dislocations is still debated, and numerous variations of surgical procedures have been published [2]. Until 5 years ago, the procedures focused on coracoclavicular (CC) stabilization [17,18,19]. However, persisting posterior instability has been observed after CC stabilization without AC stabilization, and patients with posterior instability had substantially poorer clinical results [1, 18]. Furthermore, cadaveric biomechanical studies have identified the acromioclavicular ligament complex (ACLC) as the primary stabilizer preventing posterior translation and rotation [7,8,9,10]. Therefore, the recent surgical techniques have focused on both CC and AC stabilization [3, 6, 11, 12, 20, 21, 23].
Regarding the biomechanical role of the ACLC, Klimkiewicz et al. demonstrated that the superior part of the ACLC is the main contributor to overall ACLC restraint against posterior translation of the distal clavicle [15]. However, specific regional contributions in the superior part of ACLC are still unclear. Understanding the specific areal contributions for posterior stability of the ACLC’s superior half, where the surgeon can easily access to repair, augment, or reconstruct the ACLC, may help to improve the development of surgical techniques for AC joint dislocation. The purpose of this study is to evaluate the different contributions of the anterior, superior, and posterior segments of the ACLC’s superior half for posterior translational and rotational stability.
Materials and methods
Experimental design
The superior half of ACLC was divided into three regions; Region A (0°–60°): an anterior 1/3 region of the superior half of ACLC, Region B (60°–120°): a superior 1/3 region of the superior half of ACLC, and Region C (120°–180°): a posterior 1/3 region of 1/3 of the superior half of ACLC (Fig. 1).
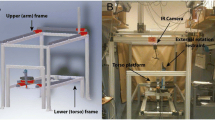
Biomechanical testing was performed to evaluate the resistance force against passive posterior translation and the resistance torque against passive posterior rotation during the following five conditions. (1) Stability was tested on all specimens in their intact condition (n = 15). (2) The ACLC was dissected and stability was tested (n = 15). (3) Specimens were randomly divided into three groups by regions of suturing (Fig. 2). Stability was tested after suturing Region A (0°–60°), Region B (60°–120°), or Region C (120°–180°) (Figs. 2, 3, n = 5 per group). Each region was sutured using four 2-0 FiberWire® (Arthrex Inc., Naples, FL) sutures. (5) Stability was tested after suturing an additional region: Region A + B (0°–120°), Region B + C (60°–180°), or Region A + C (0°–60°, 120°–180°) (Figs. 2, 3, n = 5 per group).
Representative pictures and schemas of suturing ACLC’s superior half. a, d, g Combinations of anterior, superior, and posterior views of suturing Region A (0°–60°). b, e, h Combinations of anterior, superior, and posterior views of suturing Region B (60°–120°). c, f, i. Combinations of anterior, superior, and posterior views of suturing and Region C (120°–180°)
Specimen preparation
Fifteen fresh-frozen cadaveric shoulders were analyzed in this study (mean age of 58.4 ± 12.9). All specimens were obtained from Medcure Inc. (Portland, OR). Specimen preparation was done in accordance with previously published methods [3, 5, 22]. Each shoulder specimen was thawed overnight at room temperature and disarticulated at the glenohumeral joint. The clavicle and scapula were dissected free of all soft tissue except the ACLC, the CC ligaments, and the coracoacromial ligament. The scapula was trimmed and potted with plaster of Paris in a 7.6 cm (diameter) × 7.6 cm (length) section of polyvinyl chloride (PVC) pipe. The glenoid surface was aligned parallel to the floor when the PVC pipe positioned upright. The scapula was secured to a swivel fixture on the X–Y table of a servohydraulic testing system (MTS Systems Corp). The clavicle was then trimmed to 13 cm and potted with bone cement in a 3.2 cm (diameter) × 6.4 cm (length) section of PVC pipe, so that its long axis was centered and ran parallel within the PVC pipe. This enabled clavicular fixation to the actuator of the MTS machine with a custom aluminum clamp. The local institutional review board provided approval for the study. The Health Center’s safety office and OSHA approved the purchase and disposal of cadaver specimens.
Biomechanical test setup
The pipe-cemented specimens were positioned anatomically with the scapula secured to a swivel fixture on an X–Y–Z table of a servohydraulic testing system (MTS Systems Corp). The clavicle side was attached to a custom fixture allowing anterior–posterior translation and rotation motion without moving the specimen. A pneumatic cylinder (Bimba, Monee, IL, USA) connected to 100 lb load cells (Futek, Irvine, CA, USA) was hooked to the custom fixture (parallel to the AC joint) on the clavicle side to generate an anterior–posterior translational force. This setup allowed the investigation of rotational and anterior–posterior loading during the cutting procedure without repositioning the specimen. A displacement controlled setting was used to run the test.
Translational testing
The clavicle was translated anteroposterior with respect to the acromion. A linear displacement of 10 mm in the anterior and posterior directions was applied. This distance has been described in prior studies as native AC joint motion without disturbing the AC joint capsule or the CC ligaments [3, 4, 6]. Fifteen cycles were analyzed after preconditioning with five cycles of reduced distances (5 mm of displacement). The required force to achieve the designated displacement was recorded by load cells. The values of the last cycle were used for analysis.
Rotational testing
The attached translational actuator was released, so the potted clavicle could be fixed with its long axis in line with the shaft of the MTS actuator. The clavicle was rotated about its long axis 20° posterior and 20° anterior at a rate of 5° per second, as was done in a previous study [3]. Anterior rotation was designated as the superior aspect of the clavicle moving anteriorly, and posterior rotation was designated as posterior movement of the superior aspect of the clavicle. Ten cycles were completed after preconditioning with five cycles of reduced distances (10° of displacement). The required force to achieve the designated displacement was recorded by the MTS machine. The values of the last cycle were used for analysis.
The UConn Health Institutional Review Board (IRB) confirmed that the use of de-identified cadaveric specimens does not constitute human subject research.
Statistical analysis
Assuming a standard deviation of 30 N in translation force and 0.4 N-m of torque across the testing conditions with a correlation of 0.5 among the repeated measures We assumed by as. A sample size of ten specimens would provide 80% power at an alpha level of 0.05 to detect a 20 N difference in translation and a 2 N-m difference in torque. Descriptive statistics were calculated using mean and standard deviation or frequency and proportion where appropriate. Differences in posterior translational force and rotational torque with different suturing conditions were analyzed with a one-way repeated-measure ANOVA. Following a significant ANOVA, differences between the intact and suturing conditions were evaluated with Dunnett’s method for multiple comparisons. An alpha level of 0.05 was set for all comparisons.
Results
Posterior translational force
The resistance force against posterior translation in the intact condition significantly decreased after dissection of the ACLC (P < 0.001, Fig. 4). Suturing Region A (0°–60°), Region B (60°–120°), or Region C (120°–180°) yielded a significantly lower resistance force for posterior translation compared to the intact condition (P < 0.001, Fig. 4). The resistance forces increased after suturing Region A when compared with complete dissection of the ACLC (P = 0.025, Fig. 4).
Posterior translational force (N) during the 10 mm displacement of distal clavicle with intact condition of ACLC, after dissection of overall ACLC (ACLC-), suturing Region A (0°–60°), Region B (60°–120°), and Region C (120°–180°) with remaining intact coracoclavicular ligaments. The error bars indicate the standard deviation. ***P < 0.001 compared with the intact condition. †P < 0.05 compared with the dissected ACLC. #P between 0.05 and 0.1 compared with the dissected ACLC
Suturing Region A + B (0°–120°) significantly increased the resistance force compared to complete dissection of the ACLC (P = 0.004, Fig. 5). There was no significant difference in resistance force between the complete dissection of the ACLC and suturing Region B + C (60°–180°) or Region A + C (0°–60°, 120°–180°) (n.s, respectively, Fig. 5).
Posterior translational force (N) during the 10 mm displacement of distal clavicle with intact condition of acromioclavicular ligament complex (ACLC), after dissection of ACLC (ACLC-), suturing Region A + B (0°–120°), Region B + C (60°–180°), and Region A + C (0°–60°, 120°–180°) with remaining intact coracoid clavicular ligaments. The error bars indicate the standard deviation. *P < 0.05 and ***P < 0.001 compared with the intact condition. ††P < 0.01 compared with the dissection of all capsule condition
Posterior rotational torque
The resistance torque against posterior rotation significantly decreased after complete dissection of the ACLC (P < 0.001, Fig. 6). Suturing Region A, Region B, or Region C yielded a significantly lower resistance torque for posterior rotation compared to the intact condition (P = 0.006, P = 0.004, P < 0.001, respectively, Fig. 6). The resistance torque after suturing Region A or Region B increased when compared with complete dissection of the ACLC (P = 0.020, P = 0.045, respectively, Fig. 6).
Posterior rotational torque (N-m) during the 20 degree rotation of distal clavicle with intact condition of acromioclavicular ligament complex (ACLC), after dissection of ACLC (ACLC-), suturing Region A (0°–60°), Region B (60°–120°), and Region C (120°–180°) with remaining intact coracoclavicular ligaments. The error bars indicate the standard deviation. **P < 0.01 and ***P < 0.001 compared with the intact condition. †P < 0.05 compared with the dissected condition
The resistance torque after suturing Region A + C significantly increased when compared to the completely dissected ACLC (P < 0.001, Fig. 7). There were no significant differences in resistance torque between the dissected ACLC and suturing Region A + B or Region B + C (n.s, respectively, Fig. 7).
Posterior rotational torque (N-m) during the 20 degree rotation of distal clavicle with intact condition (Intact) of acromioclavicular ligament complex (ACLC), after dissection of ACLC (ACLC-), suturing Region A + B (0°–120°), Region B + C (60°–180°), and Region A + C (0°–60°, 120°–180°) with remaining intact coracoclavicular ligaments.. The error bars indicate the standard deviation. *P < 0.05, **P < 0.01, and ***P < 0.001 compared with the intact condition. †††P < 0.01 compared with the dissection of the ACLC
Discussion
The most important finding of the present study was each segment of the ACLC’s superior has different contributions for posterior translational and rotational stability of AC joint. The resistance forces against posterior translation increased after suturing Region A and when compared with complete dissection of the ACLC (Fig. 4). Moreover, the resistance force after suturing Region A + B significantly increased compared to complete dissection of the ACLC. Furthermore, there was no significant difference in resistance force between the complete dissection of the ACLC and suturing Region B + C and Region A + C (Fig. 5). Klimkiewicz et al. reported the superior part of the ACLC was the main contributor to the overall ACLC’s posterior translational stability [15]. However, there are some differences in the method of segmentation between the current study and Klimkiewicz’s study. The present study focused on the superior half of ACLC and divided it into three regions (Region A, B, and C), due to the clinical relevance for repair or augmentation. Klimkiewicz et al. sectioned the overall ACLC into four segments (anterior, superior, posterior, and inferior) with reference to clavicular anatomy. The authors reported that the contribution of the superior segment of the ACLC to posterior translational stability was statistically significant relative to all other sectioning conditions. Sectioning the posterior ACLC was only significant relative to the native condition, but not when compared with all the other ligaments. In an anatomical study of the AC ligament, Nakazawa et al. reported the ACLC is divided into two parts (superoposterior and anteroinferior bundles) and has several anatomical variations (categorized into three types) [16]. These anatomic variations may have further contributed to the different results between the studies. Based on the present findings, Region A and Region B may contribute more than the Region C to the resistance force against posterior translation.
For posterior rotational stability, we demonstrated that the resistant torque after suturing Region A + C significantly increased compared to the dissected ACLC. In contrast, there was no significant difference in resistance torque between the dissection of the ACLC and suturing Region A + B or Region B + C. To our knowledge, this is the first study to analyze the regional contribution of the superior half of the ACLC to rotational stability. Kippe et al. compared the posterior rotational torque after a Weaver–Dunn reconstruction to native shoulders [14]. Following the technique, which does not reconstruct the ACLC, the resistance torque against posterior rotation was decreased about 85% or more when compared with native shoulders. The present study also demonstrated that the resistance torque against posterior rotation decreased about 94% after dissection of the ACLC. Furthermore, the resistance force against posterior translation decreased about 79% after dissection of the ACLC when compared to the intact condition. These findings suggest that the ACLC is more important for posterior rotational stability than posterior translational stability.
Based on the present findings, repair or reconstruction of the entire superior ACLC is required to restore both posterior translational and rotational stability of the AC joint. In chronic case, reconstruction of the entire superior ACLC may be needed, due to the limited healing potential of the acromioclavicular ligaments. Beitzel at al. biomechanically compared four techniques for AC reconstruction in addition to CC stabilization (modified anatomic CC ligament reconstruction, intramedullary, transacromial, and 8-turn) [3]. The modified anatomic CC ligament reconstruction, which wraps the entire AC joint using a semitendinosus tendon, was the most stable method with regard to clavicle translation and rotation. However, this technique has several limitations to require a long tendon, tendon-to-bone attachment, and surgical invasion due to access to the inferior part of the AC joint. Therefore, our study focused on the superior half of the AC joint and analyzed the individual contributions of different regions for posterior translational and rotational stability. Recently, another modified anatomic CC ligament reconstruction method was reported [13]. This technique reconstructed the superior ACLC with a semitendinosus tendon after CC ligament reconstruction and repaired the ruptured anterior and posterior ACLC with suture anchors. At midterm follow-up, 93% of patients had two-dimensional radiographic stability and three-dimensional dynamic clinical stability; therefore, restoring the superior ACLC may also optimize the clinical outcome after AC repair or reconstruction.
The present study has several limitations. (1) The in vitro nature of biomechanical evaluation can be a limiting factor in the application of the findings to the in vivo conditions of the shoulder complex. This is particularly true in the AC joint, with its specific 3D forces and complex contributions to multiple shoulder motions. Accurate replication of these forces in a cadaveric study may be difficult. To evaluate changes in biomechanical behavior under translational and rotational stress, we used a methodology based on the previous descriptions [3, 9]. The major strength of this biomechanical setup was that all tested motions could be performed without changing the position of the specimens. Each specimen was placed and centered in the materials testing machine, so that all changes measured through the test could be compared to the native state. We thought that this would be necessary to detect the changes that would arise with each consecutive modification to the specimens. (2) Specimens tested were from donors with a mean age of 58 ± 13 years, whereas patients with AC dislocation are usually younger. (3) Biomechanical testing with cadaveric specimens does not give information on healing biology, and the tested biomechanical setup cannot reproduce the clinical situation. The clinical relevance of this study is to add the knowledge that each segment of the ACLC’s superior has different contributions for posterior translational and rotational stability of AC joint and surgical techniques restoring the entire superior ACLC are recommended to address both posterior translational and rotational stability.
Conclusions
Region A + B (0°–120°) contributed more to posterior translational stability than Region B + C (60°–180°) or Region A + C (0°–60°/120°–180°). In contrast, Region A + C contributed more to posterior rotational stability than Region A + B or Region B + C. Based on these findings, surgical techniques restoring the entire superior ACLC are recommended to address both posterior translational and rotational stability of the AC joint.
References
Barth J, Duparc F, Baverel L, Bahurel J, Toussaint B, Bertiaux S et al (2015) Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res 101:S305–S311
Beitzel K, Cote MP, Apostolakos J, Solovyova O, Judson CH, Ziegler CG et al (2013) Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy 29:387–397
Beitzel K, Obopilwe E, Apostolakos J, Cote MP, Russell RP, Charette R et al (2014) Rotational and translational stability of different methods for direct acromioclavicular ligament repair in anatomic acromioclavicular joint reconstruction. Am J Sports Med 42:2141–2148
Beitzel K, Obopilwe E, Chowaniec DM, Niver GE, Nowak MD, Hanypsiak BT et al (2011) Biomechanical comparison of arthroscopic repairs for acromioclavicular joint instability: suture button systems without biological augmentation. Am J Sports Med 39:2218–2225
Beitzel K, Sablan N, Chowaniec DM, Obopilwe E, Cote MP, Arciero RA et al (2012) Sequential resection of the distal clavicle and its effects on horizontal acromioclavicular joint translation. Am J Sports Med 40:681–685
Braun S, Beitzel K, Buchmann S, Imhoff AB (2015) Arthroscopically assisted treatment of acute dislocations of the acromioclavicular joint. Arthrosc Tech 4:e681–e685
Dawson PA, Adamson GJ, Pink MM, Kornswiet M, Lin S, Shankwiler JA et al (2009) Relative contribution of acromioclavicular joint capsule and coracoclavicular ligaments to acromioclavicular stability. J Shoulder Elbow Surg 18:237–244
Debski RE, Parsons IMT, Woo SL, Fu FH (2001) Effect of capsular injury on acromioclavicular joint mechanics. J Bone Joint Surg Am 83-A:1344–1351
Dyrna FGE, Imhoff FB, Voss A, Braun S, Obopilwe E, Apostolakos JM et al (2018) The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med 46:1432–1440
Fukuda K, Craig EV, An KN, Cofield RH, Chao EY (1986) Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am 68:434–440
Hann C, Kraus N, Minkus M, Maziak N, Scheibel M (2018) Combined arthroscopically assisted coraco- and acromioclavicular stabilization of acute high-grade acromioclavicular joint separations. Knee Surg Sports Traumatol Arthrosc 26:212–220
Izadpanah K, Jaeger M, Ogon P, Sudkamp NP, Maier D (2015) Arthroscopically assisted reconstruction of acute acromioclavicular joint dislocations: anatomic AC ligament reconstruction with protective internal bracing-the “AC-RecoBridge” technique. Arthrosc Tech 4:e153–e161
Kibler WB, Sciascia AD, Morris BJ, Dome DC (2017) Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy 33:696–708
Kippe MA, Demetropoulos CK, Baker KC, Jurist KA, Guettler JH (2009) Failure of coracoclavicular artificial graft reconstructions from repetitive rotation. Arthroscopy 25:975–982
Klimkiewicz JJ, Williams GR, Sher JS, Karduna A, Des Jardins J, Iannotti JP (1999) The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg 8:119–124
Nakazawa M, Nimura A, Mochizuki T, Koizumi M, Sato T, Akita K (2016) The orientation and variation of the acromioclavicular ligament: an anatomic study. Am J Sports Med 44:2690–2695
Salzmann GM, Walz L, Buchmann S, Glabgly P, Venjakob A, Imhoff AB (2010) Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med 38:1179–1187
Scheibel M, Droschel S, Gerhardt C, Kraus N (2011) Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med 39:1507–1516
Tauber M, Gordon K, Koller H, Fox M, Resch H (2009) Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med 37:181–190
Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P (2016) Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med 44:482–489
Triantafyllopoulos IK, Lampropoulou-Adamidou K, Schizas NP, Karadimas EV (2017) Surgical treatment of acute type V acromioclavicular joint dislocations in professional athletes: an anatomic ligament reconstruction with synthetic implant augmentation. J Shoulder Elbow Surg 26:e369–e375
Voss A, Singh H, Dyrna F, Buchmann S, Cote MP, Imhoff AB et al (2017) Biomechanical analysis of intra-articular pressure after coracoclavicular reconstruction. Am J Sports Med 45:150–156
Weiser L, Nuchtern JV, Sellenschloh K, Puschel K, Morlock MM, Rueger JM et al (2017) Acromioclavicular joint dislocations: coracoclavicular reconstruction with and without additional direct acromioclavicular repair. Knee Surg Sports Traumatol Arthrosc 25:2025–2031
Funding
The University of Connecticut Health Center/UConn Musculoskeletal Institute has received direct funding and material support from Arthrex Inc., Naples, FL, USA. The company had no influence on study design, data collection, or interpretation of the results or the final manuscript.
Author information
Authors and Affiliations
Contributions
Authors DM, JDJ, EO, and BS participated in obtaining the data. Authors ADM and MPC were responsible for the analysis of data. Authors FD, FBI, and KB made substantial contribution in designing the methodology and providing oversight to the conduct of the study. All authors (DM, JDJ, EO, BS, ADM, MPC, FD, FBI, and KB) made significant contributions to the development and revision of the manuscript. In addition, all authors have given final approval for the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors DM, FD, JDJ, EO, FBI, BS declare no conflict of interest. MPC received personal fee from the Arthroscopy Association of North America. KB is a consultant for Arthrex GmbH, Germany. ADM received grants to his institution from Arthrex Inc. Naples, Fl, USA. He is a consultant for Arthrex Inc. Naples Fl, USA and Ortho x, Inc., Lewisville, TX, USA.
Ethical approval
The above study was conducted using only de-identified cadaveric specimens and is therefore not considered human subjects research. Our institutional review board (IRB) provides a Human Research Determination Form to help investigators determine whether IRB review is needed. While we have confirmed with our IRB that projects conducted in our biomechanics laboratory that utilize de-identified specimens does not constitute human subjects research and therefore no review required.
Rights and permissions
About this article
Cite this article
Morikawa, D., Dyrna, F., Cote, M.P. et al. Repair of the entire superior acromioclavicular ligament complex best restores posterior translation and rotational stability. Knee Surg Sports Traumatol Arthrosc 27, 3764–3770 (2019). https://doi.org/10.1007/s00167-018-5205-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5205-y