Abstract
Purpose
Torsional osteotomy of the distal femur allows anatomic treatment of patellofemoral instability and patellofemoral pain syndrome in cases of increased femoral antetorsion. The purpose of this study was to investigate the effects of distal femoral torsional osteotomy on pressure distribution of the medial and lateral patellar facet.
Methods
Nine fresh frozen human knee specimens were embedded in custom-made 3D-printed casts and tested with a robotic arm. Torsional osteotomy could be simulated ranging from increased femoral antetorsion of 25° with a corresponding lateralization of the patella to an overcorrected value of 5° of femoral antetorsion. The peak and mean lateral and medial compartment pressure was measured in 0°, 15°, 30°, 45°, 60° and 90° flexion beginning with neutral anatomic muscle rotation.
Results
The medial aspect of the patella showed a significant influence of femoral torsion with an increase of mean and peak pressure in all flexion angles with progressive derotation from 15° external rotation to 5° internal rotation (p = 0.004). The overall pressure difference was highest in near extension and stayed on a constant level with further flexion. On the lateral facet, the derotation resulted in decrease of pressure in near extension; however, it had no significant influence on the mean and peak pressure through the different torsion angles (n.s.). Unlike on the medial facet, a significant consistent increase of peak pressure from 0° to 90° flexion could be shown (p = 0.022) on the lateral patella aspect.
Conclusion
Distal femoral torsional osteotomy to correct pathological femoral antetorsion leads to a redistribution of retropatellar pressure. External derotation leads to an increased peak pressure on the medial patellar facet and can impair simultaneous cartilage repair. However, as the lateral patellofemoral load decreases, it has a potential in preventing patellofemoral osteoarthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patellofemoral instability includes patella tilt, maltracking, subluxation and dislocation [31]. The multifactorial cause of patellofemoral instability comprises medial patellofemoral ligament (MPFL) disruption, trochlear dysplasia, excessive tibial tubercle (TT) lateralization with elevated tibial tubercle–trochlear groove (TTTG) distance, or patella alta [1, 30]. Another important factor, though sometimes underestimated, includes variances of mechanical malalignment such as genu valgum or femoral antetorsion [5, 9, 27]. It affects all corresponding static and dynamic factors of patellofemoral instability as it is essential for bony morphology and the resulting muscular strain [7, 16, 30]. Distal femoral osteotomy (DFO) procedures combined with additional external torsional osteotomies have been proved to be a reliable option for correction of torsional pathologies in patellofemoral instability [4, 16, 32]. High success rates with torsional osteotomies are reported in the literature [6, 17, 32].
Patellar dislocation and chronic patellofemoral instability are linked to the development of abnormal contact stress and joint degeneration [22, 24]. Frequently, concomitant osteochondral injuries, especially cartilage lesions of the patellar surface, are present [12, 23, 29]. As a major contributor to adverse clinical outcomes, these lesions demand a simultaneous treatment. In literature, due to the numerous complex variables influencing treatment of patellofemoral instability, there is still a lack of high-level evidence [21].
Torsional osteotomies are more frequently performed in patellofemoral dysbalance in the last few years, so biomechanical analyzation of the mechanical load gives an important indication for evaluating treatment options in the clinical setting. It is unknown if a torsional DFO leads to increased peak contact pressure to the opposing retropatellar articular cartilage and hence might influence the outcome of a cartilage treatment. The purpose of the current study was to evaluate the effects of torsional DFO on retropatellar contact pressure in human cadaveric knees, as there is an enormous lack of evidence in literature. It was hypothesized that torsion significantly increases the articular contact patterns of the medial patellar facet. On the other hand, a reduction of the lateral facet contact pressure would be preferable in cases of early osteoarthritis. According to the results found in this study, a guideline might be given to the clinician for concomitant patellar cartilage therapy.
Materials and methods
To investigate the hypothesis, nine fresh frozen human knee specimens (Med Cure, Orlando, USA) were used. No ethics approval was required for this cadaver study. The mean age was 66.1 ±11.5 (range 43.2–77.4) years; there were five males and four females. The knees had no history of disease or prior surgery. All knee specimens were thawed overnight at room temperature.
Prior to testing, every knee underwent a radiological evaluation. The mean Caton–Deschamps index of 0.95 ±0.09 (range 0.79–1.06) indicated a physiological patella height and the patellar morphology was mainly Wiberg type 2. No trochlear dysplasia, osteoarthritis or any patellar deformity was evident.
Each specimen initially consisted of all bone and soft tissue transected 20 cm proximal and distal to the joint line. The soft tissue was excised leaving capsule, fascia, ligaments and tendons intact. The quadriceps muscles were separated into five components: rectus femoris, vastus intermedius, vastus medialis longus, vastus medialis obliquus and vastus lateralis. Additionally, the tractus iliotibialis (ITB) has been prepared for testing. The vastus intermedius was elevated from the anterior femoral shaft and grouped with the rectus femoris. The muscular components and the ITB were each stitched to cloth material and additionally fixed with cable wires to apply muscle load with a total of 205N [11, 25, 34]. The specimens were embedded in 3D-printed castings using quick hardening polyurethane resin (RenCast® FC Isocyanate/FC 52 Polyol). To ensure correct loading, the tibia was potted perpendicular to the joint with the knee in full extension. The femur was aligned parallel to its anatomic axis. Axial rotation of both the tibia and the femur was minimized with respect to the epicondyle axis. To realize these orientation specifications, a cross line laser was utilized during the potting procedure. Specimens were kept moist throughout the preparation and the experiment by spraying physiological saline water occasionally.
A 4041 Tekscan sensor (Tekscan Inc., Boston, USA) was used to measure patellofemoral mean and peak contact pressure. The sensor was 0.1 mm thick with two separate sensors measuring 40.1 × 24.9 mm each, detecting a maximal pressure of 3.45 MPa. Calibration and equilibration were carried out based on manufacturer’s guidelines [3, 8]. The sensor was inserted through the suprapatellar recess maintaining the medial and lateral capsule and ligaments. The two separate sensors covered both the medial and lateral patellar surfaces being pasted up to the cartilage (Superglue, Pattex©, Düsseldorf, Germany) to prevent it from moving during knee flexion.
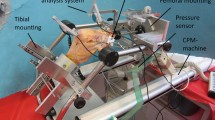
A six-axis robot arm was used for biomechanical testing (Staubli, RX 90 B, Germany, Bayreuth). The tibia was connected to the tip of the robotic system which consisted of a multidimensional force torque sensor (90M40A3, JR3 Inc., Woodland, USA). The femur and the rotatable loading mechanism were attached to the robot’s base frame (Fig. 1). Each of the six different muscle strings were positioned and loaded individually in accordance with directions and physiological cross-sectional areas regarding the anatomic characteristics [10, 34]. Hyperextension of the joint was determined by the system neutralizing the applied loads. The resulting pose was utilized to calculate the measurement flexion angles. To account for the femur mass, half of every specimen’s weight and the connector’s weight were compensated. All other acting forces and moments, except the torque around the fixed epicondyle axis, were minimized during all applied motions. The peak and mean lateral and medial compartment pressure was then measured in 0°, 15°, 30°, 45°, 60° and 90° flexion (with an error of less than 0.1°). Before the investigation, all specimens were preconditioned by three flexion–extension cycles from 0° to 90° of flexion.
Experimental arrangement of the robotic knee simulator. The femur (F) and tibia (T) were potted in custom-made 3D casts. The femur and the rotatable loading frame were attached to the robot’s base frame. The tibia was connected to the robot’s tipcylinders using a bone cement compound. A pressure-sensitive sensor foil was inserted through the suprapatellar recess and fixed with glue. The rotation angle was set by prefabricated fitting (an enlarged detail of the rotation frame)
The study concentrated on the investigation of the peak pressure on the medial and lateral patellofemoral compartment during torsional adjustment osteotomy of the femur. To mimic the torsional osteotomy, a special custom-made loading frame was designed to rotate the femur’s muscle strings manually in 5° steps from 5° external rotation to 15° internal rotation with the femur being fixed. Accordingly, a stepwise clinical relevant situation could be simulated ranging from increased femoral antetorsion of 25° with a corresponding lateralization of the patella to an overcorrected standard value of 5° of femoral antetorsion with a then medialized patella. The peak and mean lateral and medial patellofemoral compartment pressures were then measured in 0°, 15°, 30°, 45°, 60° and 90° flexion beginning with neutral anatomic muscle rotation.
Statistical analysis
The statistical analysis is based upon a two-factor analysis of variance (ANOVA) with repeated measures. Hereby, differences between various conditions of angle and rotation were tested. The data set is balanced and includes nine specimens for which observations are given under each condition. To control for possible violations against the sphericity assumption, a Huynh–Feldt and Greenhouse–Geisser correction was conducted. For all statistical decisions, a significance level of 0.05 was used. Violations against the sphericity assumption seemed to be of minor extent in the overall analysis and only have to be taken into account when analyzing differences under the medial pressure setup. The analysis is conducted with SPSS version 24.0 (IBM, Armonk, New York), while the results were additionally recalculated with R version 3.4.2 (Austria, Vienna). Given the exploratory nature of this study, a priori sample size analysis was not performed.
Results
The medial aspect of the patella (Fig. 2) showed a significant influence of external femoral derotation with an increase of peak pressure with progressive derotation from 15° internal torsion to 5° external torsion (p = 0.004) as well as a tendency to higher peak pressures in all flexion angles (n.s.). Similarly, the mean medial contact pressure increased (p = 0.008). Accordingly, a decrease of mean and peak pressure was detected for the lateral facet and femoral external derotation from 15° internal torsion to 5° external torsion (Fig. 3). The strongest effect was measured between 0° and 30° of knee flexion. However, the derotation had no significant influence through the different flexion angles (n.s.). Still, a consistent increase of peak pressure from 0° to 90° flexion could be detected (p = 0.022). Retropatellar mean pressure was lowest in near extension and increased gradually with flexion. The mean pressure remained < 0.41 MPa for flexion up to 90°.
Discussion
The most important finding of this study was that the patellofemoral pressure at the medial facet increases significantly in distal femoral torsional osteotomies. Mean and peak pressure of the medial facet increases highest in 15°–30° flexion angles and remains on a constant level with further flexion. In simulated increased femoral antetorsion and corresponding lateralization of the patella, the mean and peak pressure is higher on the lateral facet compared to the medial facet and increases with continuous knee flexion.
Osteotomies around the knee have been utilized independently as well as in combination with cartilage repair techniques to improve symptoms of cartilage pathology and patellofemoral symptoms. In the tibiofemoral joint, both opening- and closing-wedge femoral or tibial osteotomies have been established as a technique to off-load damaged cartilage areas in an attempt to provide symptom relief [14, 20, 36]. In the setting of cartilage repair, a concomitant osteotomy can be used to off-load the repair site and to support the healing process [2].
In pathologic femoral antetorsion, a distal femoral torsional osteotomy provides significant pain relief as well as patellofemoral stability. In a cadaver study of mature femora, Lee et al. quantified the impact of femoral antetorsion on quadriceps tension and patellofemoral contact pressure [19]. Increased femoral antetorsion caused greater lateral contact pressure of the patella. The highest pressure values were noted between 30° and 60° of knee flexion. Dickschas et al. reported significant pain relief and correction of patellar tracking with femoral torsional osteotomies in patients with additional torsional deformity of the femur causing anterior knee pain and patellar instability [6, 35].
Osteochondral fractures are frequent concomitant lesions after patellar dislocation [33]. Nomura et al. reported even a 95% incidence of cartilage damage with 72% of osteochondral lesions located on the medial patellar facet [28]. In chronic patellofemoral instability with lateralized patella, OA develops in the lateral patellofemoral joint, mainly due to consistent lateral hyperpression [15]. The results of this study confirm the influence of lateralized patella and corresponding hyperpression. This suggest a favorable situation of torsional osteotomies to reduce lateral facet pressure and therefore prevent early OA. In a previous in vitro assessment, equivalent findings of excessive lateral hypercompression in pathologic femoral antetorsion could be demonstrated [19]. Despite the advantages of torsional osteotomies for the lateral facet, this assessment revealed an increase of retropatellar pressure of the medial facet in external derotation osteotomy. Elevated intraarticular pressure impairs the outcome of cartilage repair techniques. Kuroda et al. demonstrated the potentially ill effects of overmedialization of the tuberosity [18]. In elevated TTTG, cartilage lesions on the medial facet of the patella pose a contraindication for medial tubercle transposition, as it increases the intraarticular pressure as well. For cartilage lesions of the lateral facet, antero-medialization of the tibial tubercle is meant to be successful in cartilage repair [13].
Analogous to surgical medialization of the tuberositas tibiae, the data presented in this study show that torsional osteotomies have a significant influence on patellar pressure. This suggests that the surgical combination of torsional osteotomy and cartilage repair has to take the localization of the cartilage defect into account. Located on the medial patellar facet, the simultaneous intervention might have negative effects on the outcome of cartilage repair. On the other hand, treating cartilage lesions of the lateral facet, the outcome might be favorable. Furthermore, the results indicate that external torsional osteotomy might delay the development of early OA, especially of the lateral facet by reducing the intraarticular pressure forces. In future cartilage studies involving the patellofemoral joint, lesions should be separated by location and evaluated separately, to better target available and advancing treatment options in this region.
The clinical relevance of the present data is highlighted by the fact that torsional osteotomy influences the retropatellar pressure dissimilarly regarding the lateral and medial facet. As a result, the outcome of simultaneous cartilage repair can be impaired at the medial facet, but be favorable on the lateral facet. This poses important information for the orthopedic surgeon using simultaneous interventions. Furthermore, a torsional osteotomy can reduce a prearthrotic deformity of the patellofemoral joint.
Limitations of this study include those inherent to in vitro testing. The specimens’ flexion angles were reached by the robot neutralizing all measured loads except the torque around the epicondyle axis. Care was taken to avoid misalignment of that axis, since it would have induced different motions and thereby in deviations regarding the pressure measurements and the flexion poses. Nonetheless, the flexion poses might differ from the ones, which would have been reached by real in vivo conditions. Like in other in vitro studies, the specimens were elderly and it is unknown if the mean age influences the studies’ outcome.
Since, among others, Mueller et al. [26] demonstrated that the amount of muscle loads does not necessarily affect biomechanical experiments, the muscle loads were chosen to be static and lower than in vivo, to consider the test setup boundaries.
Conclusion
Distal femoral torsional osteotomy increases medial patellofemoral contact pressure and can impair simultaneous cartilage repair. However, as the lateral patellofemoral load decreases, it has a potential in preventing patellofemoral osteoarthritis.
References
Aglietti P, Buzzi R, Insall J (2001) Disorders of the patellofemoral joint. In: Insall JN, Scott WN (eds) Surgery of the knee, 3. edn. Churchill Livingstone, Philadelphia, pp 913–1043
Bauer S, Khan RJ, Ebert JR et al (2012) Knee joint preservation with combined neutralising high tibial osteotomy (HTO) and matrix-induced autologous chondrocyte implantation (MACI) in younger patients with medial knee osteoarthritis: a case series with prospective clinical and MRI follow-up over 5 years. Knee 19:431–443
Brimacombe JM, Wilson DR, Hodgson AJ, Ho KC, Anglin C (2009) Effect of calibration method on Tekscan sensor accuracy. J Biomech Eng 131:034503 1–4
Brinkman JM, Freiling D, Lobenhoffer P, Staubli AE, van Heerwaarden RJ (2014) Supracondylar femur osteotomies around the knee: patient selection, planning, operative techniques, stability of fixation, and bone healing. Orthopade 43(Suppl;1):1–10
Bruce WD, Stevens PM (2004) Surgical correction of miserable malalignment syndrome. J Pediatr Orthop 24:392–396
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132:289–298
Dye SF (2005) The pathophysiology of patellofemoral pain: a tissue homeostasis perspektive. Clin Orthop Relat Res 436:100–110
Drewniak EI, Crisco JJ, Spenciner DB, Fleming BC (2007) Accuracy of circular contact area measurements with thin-film pressure sensors. J Biomech 40:2569–2572
Eckhoff DG, Montgomery WK, Kilcoyne RF, Stamm ER (1994) Femoral morphometry and anterior knee pain. Clin Orthop Relat Res 302:64–68
Farahmand F, Senavongse W, Amis AA (1998) Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint. J Orthop Res 16:136–143
Farahmand F, Tahmasbi MN, Amis AA (1998) Lateral force–displacement behaviour of the human patella and its variation with knee flexion: a biomechanical study in vitro. J Biomech 31:1147–1152
Farr J, Covell DJ, Lattermann C (2012) Cartilage lesions in patellofemoral dislocations: incidents/locations/when to treat. Sports Med Arthrosc Rev 20:181–186
Frosch S, Balcarek P, Walde TA et al (2011) The treatment of patellar dislocation: a systematic review. Z Orthop Unfall 149:630–645
Fu FH, Zurakowski D, Browne JE et al (2005) Autologous chondrocyte implantation versus debridement for treatment of full-thickness chondral defects of the knee: An observational cohort study with 3-year follow-up. Am J Sport Med 33:1658–1666
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA (2004) Osteochondral defects in the human knee: influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med 32:1451–1458
Heegaard J, Leyvraz PF, Curnier A, Rakotomanan L, Huiskes R (1995) The biomechanics of the human patella during passive knee flexion. J Biomech 28:1265–1279
Hinterwimmer S, Minzlaff P, Saier T, Niemeyer P, Imhoff AB, Feucht MJ (2014) Biplanar supracondylar femoral derotation osteotomy for patellofemoral malalignment: the anterior closed-wedge technique. Knee Surg Sports Traumatol Arthrosc 22:2518–2521
Kuroda R, Kambic H, Valdevit A et al (2001) Articular cartilage contact pressure after tibial tuberosity transfer. A cadaveric study. Am J Sports Med 29:403–409
Lee TQ, Anzel SH, Bennett KA et al (1994) The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res 302:69–74
Liska F, Voss A, Imhoff FB, Willinger L, Imhoff AB (2018) Nonunion and delayed union in lateral open wedge distal femoral osteotomies-a legitimate concern? Int Orthop 42(1):9–15
Liu JN, Steinhaus ME, Kalbian IL, Post WR, Green DW, Strickland SM, Shubin Stein BE (2017) Patellar instability management: a survey of the international patellofemoral study group. Am J Sports Med. https://doi.org/10.1177/0363546517732045
Mäenpää H, Lehto MUK (1997) Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res 339:156–162
Mashoof AA, Scholl MD, Lahav A, Greis PE, Burks RT (2005) Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patella dislocation. Arthroscopy 21:228–232
Mehta VM, Inoue M, Nomura E, Fithian DC (2007) An algorithm guiding the evaluation and treatment of acute primary patellar dislocations. Sports Med Arthrosc Rev 15:78–81
Merican AM, Amis AA (2009) Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J Biomech 42:1539–1546
Mueller O, Lo JH, Wuenschel M, Obloh C, Wuelker N (2009) Simulation of force loaded knee movement in a newly developed in vitro knee simulator. Biomed Eng 54(3):142–149
Nelitz M, Dreyhaupt J, Williams SR, Dornacher D (2015) Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop 39:2355–2362
Nomura E, Inoue M, Kurimura M (2003) Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 19:717–721
Nomura E, Inoue M (2005) Second-look arthroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthr Cartil 13:1029–1036
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14(1):7–12
Sheehan FT, Derasari A, Fine KM, Brindle TJ, Alter K (2010) Q-angle and J-sign: Indicative of Maltracking Subgroups in Patellofemoral Pain. Clin Orthop Relat Res 468(1):266–275
Staheli LT (1989) Torsion–treatment indications. Clin Orthop Relat Res 247:61–66
Stanitski CL, Paletta GA Jr (1998) Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med 26:52–55
Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA (2015) The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med 43(1):186–194
Strecker W, Dickschas J (2015) Torsional osteotomy: Operative treatment of patellofemoral maltracking. Oper Orthop Traumatol 27:505–524
Tang WC, Henderson IJ (2005) High tibial osteotomy: long term survival analysis and patients’ perspective. Knee 12:410–413
Funding
The Technical University of Munich has received direct funding from the German Arthritis Foundation and the German speaking Society for Arthroscopy and Joint Surgery (AGA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Liska, F., von Deimling, C., Otto, A. et al. Distal femoral torsional osteotomy increases the contact pressure of the medial patellofemoral joint in biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 27, 2328–2333 (2019). https://doi.org/10.1007/s00167-018-5165-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5165-2