Abstract
Introduction
Due to a supposed high rate of nonunions in lateral open wedge distal femur osteotomy (LOWDFO), the medial closing wedge technique has been favoured for a long time. The aim of this study was to report the occurrence of delayed- and nonunions following LOWDFO. We hypothesized that the occurrence of nonunions needing revision surgery is comparable to medial closing osteotomies.
Methods
Forty-one patients were treated with LOWDFO with a minimum follow-up of 12 months. Parameters such as age, gender, body mass index, valgus angle, the heights of the opening wedge, as well as the type of osteotomy (biplane vs single plane) were collected. Delayed union and nonunion were evaluated on radiographs along with clinical symptoms.
Results
The study group consisted of 21 females and 20 males, with a median age of 37 years at the time of surgery. Removal of hardware was performed in 63% after 1.3 years (0.6–2.1 years). The median preoperative valgus angle was 6.1° valgus (range 2–15.5°). The heights of the opening wedge ranged from 2 to 12 mm (mean 5.3 mm). Hinge fracture of the medial cortex was seen in 39%. Three patients had a delayed union, and one patient had a nonunion requiring revision surgery.
Conclusion
LOWDFO is a safe alternative to MCWDFO. Although radiolucency of the osteotomy gap can be evident on radiographs even after 12 months, this does not reflect the clinical finding. The nonunion rate is proven to be low and comparable with the nonunion rates of MCWDFOs as well as open wedge HTOs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nowadays, a medial open-wedge high tibial osteotomy (MOWHTO) represents a common and safe technique to address varus alignment [1, 2]. However, considering the past and current literature, establishing the MOWHTO was a long process. Traditionally, the HTO was performed as a lateral closed wedge procedure originally described in 1958 [3]. Until the late eighties, an open wedge HTO was considered as a precarious surgery with a high potential of nonunions [4,5,6]. Over the following two decades, its reputation had improved significantly, especially in the early 2000s due to the introduction of locking plate systems as well as better surgical techniques such as biplane osteotomies [7,8,9]. Eventually the frequency and type of complications, particularly nonunions and delayed unions, are reported to be similar to those for the lateral closing technique [10].
Comparing the development of open wedge HTOs, the same process can be seen for lateral open wedge distal femoral osteotomies (LOWDFO). The difference is that this process is shifted with a delay of two decades. One reason for this delay can be seen in the lower incidence of valgus malalignment and lateral compartment OA. On the other hand, in valgus deformities, the open wedge technique was disreputed as a high risk procedure regarding intra-operative complications as well as nonunions for a long time. The fear of nonunions is mainly based and cited on behalf of results published by Edgerton et al. [11] and Mathews et al. [12]. These authors published non-union rates of over 19–25% in medial closing wedge distal femoral osteotomies (MCWDFO) using previous fixation techniques. In literature, LOWDFOs are regarded to have even higher nonunion rates compared to MCWDFOs [13,14,15,16,17].
In the last decade, an awakened interest in LOWDFOs can be seen in an arising amount of studies investigating this issue. These studies consist mainly of smaller case series, with a mean case number of 20–25 osteotomies. The aim of this study was to report the occurrence of delayed- and nonunions following LOWDFO. We hypothesized that the time to radiologic-evident complete bone union is longer than, e.g. in tibial osteotomies, but the occurrence of nonunions is comparable. We chose not to evaluate the clinical outcome of the procedure because this is already well documented in the literature.
Materials and methods
From 2008 until the end of 2015, after excluding all patients with a follow up less than 12 months and those who were lost to follow up, 41 cases who were treated for valgus malalignment or lateral osteoarthritis of the knee with LOWDFO were studied retrospectively. Baseline data such as age, gender, diagnosis, valgus angle, the heights of the opening wedge, as well as the type of osteotomy (biplane vs single plane) and the time of plate removal were collected from medical reports. Pre-operative radiographic evaluation included anterior–posterior and lateral views of the knee, and full length standing anterior–posterior radiograph of the lower extremity for evaluation of valgus alignment.
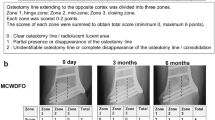
Post-operative radiographs were taken the day after surgery, then subsequently at six weeks, 12 weeks and 12 months and then as required, until the bone healing was evident. After 12 weeks, radiographs were conducted according to the patient’s medical course, especially symptoms like pain and tenderness at the osteotomy site led to regular follow ups every six weeks. Delayed union was defined as the lack of complete osseous consolidation and the presence of radiolucent areas within the opening wedge defect after 12 months, though asymptomatic. Nonunion was evaluated on radiographs along with clinical symptoms according to the following findings: radiological evidence of nonunion either hyper-, olio- or atrophic; pain; no radiologic progress in bony healing after onset of symptoms; a loss of stability or correction; subsequently requiring revision surgery.
Operative technique
First, an arthroscopy was carried out. The arthroscopy included chondral debridement or micro fracturing, osteoarticular cartilage transplantation, autologous chondrocyte implantation, implantation of collagen meniscus implant, partial meniscus resection or suture, and extraction of loose bodies.
For the LOWDFO, a lateral approach to the distal femur was performed. The position of the osteotomy depended on the pre-operative X-ray planning. The osteotomy cut was performed either in single plane or biplane technique. Single plane osteotomies, mainly previous cases, replaced the biplane technique as it has the potential to improve the axial stability and to increase the bone-to-bone contact area [18, 19]. Intra-operatively, a better control for unintentional ante- or recurvatum can be achieved. The axial cut was respectively aligned perpendicular to the femoral cortex. In biplane osteotomy it involved the posterior 3/4 of the femur, completed by a frontal plane osteotomy proceeding in an ascending direction to the anterior femoral cortex. Under X-ray control, the axial cut was performed up to about 1 cm before cutting the contralateral medial cortex. The osteotomy space was opened carefully by chisels and fixed with the Tomofix lateral distal femur plate (Depuy Synthes). In three cases, the osteotomy gap was filled with a bone graft taken from the ipsilateral iliac crest. In all other cases, no bone substitutes or grafts were used. All patients were allowed partial weight-bearing with 20 kg up to the sixth week after surgery.
Statistical analysis
Descriptive statistics to characterize the study group were calculated using means, range and standard deviation or frequency and proportion where appropriate. No power analysis has been performed because this study is a sample of convenience. The analysis was conducted with SPSS version 22.0 (IBM, Armonk, New York).
Results
We performed 41 LOWDFOs. The study group consisted of 21 females (51.2%) and 20 males (48.8%), with a median age of 37 years (range 15–64 years) at the time of surgery. The mean body mass index was 26.4 (range 19.6–38.1, SD 4.6). Ten patients had a nicotine abuse. The median time until plate removal was 1.3 years (0.6–2.1 years). Removal of hardware was performed in 63%, mainly due to discomfort or irritation of the tractus iliotibialis. The median pre-operative mechanical tibio-femoral axis was 6.1° valgus (range 2–15.5°, SD 2.9° valgus) in these patients. The heights of the opening wedge ranged from 2 to 12 mm (mean 5.3 mm, SD 1.9 mm). Hinge fracture, defined as any slightest interruption of the medial cortex on follow-up radiographs, was seen in 16 osteotomies (39%). and 17 osteotomies were performed in single plane technique. Biplane technique was performed in 24 patients, mainly recent osteotomies.
The rate of complications amounted to 12.2% (Table 1). One patient had a deep infection requiring revision surgery. After revision, there was no alteration in bony healing. In one patient, an intra-operative fracture of the frontal cortex of the biplane osteotomy was evident (Fig. 1). It healed within the six weeks of partial weight bearing and did not need further treatment. Another patient suffered from a diaphyseal shaft fracture. This patient had a femoral shaft fracture prior to the osteotomy treated with an intramedullary nail. After hardware removal and LOWDFO, a traumatic shaft fracture reoccurred proximally to the former fracture site. The treatment consisted in changing the TomoFix plate to a LISS (Less Invasive Stabilization System) distal femoral plate bridging the osteotomy as well as the shaft fracture. In one patient, an arthrofibrosis occurred. This patient had a meniscal suture along with the LOWDFO. At the time of plate removal, a manipulation under anaesthesia along with an arthroscopic arthrolysis led to full range of motion.
In three patients, an asymptomatic delayed union was apparent after 12 months of the osteotomy. Two had a single plane osteotomy, the wedge ranged from 3 to 7 mm. Two patients were smokers, the BMI was in a normal range (21.2–29.1). Though signs of bony healing like callus formation and progressing trabecular bone formation within the osteotomy gap were evident, the radiolucency and remaining defect of bone healing prohibited a plate removal. However, these patients showed no pain under full weight bearing in daily activity as well as in sporting activity. Additional clinical and radiological visits followed until full bony healing was accomplished after 14–16 months without further specific treatment.
One patient had a non-union requiring revision at 7.2 months post-operatively. This patient, a 46-year-old woman, was a smoker and had a BMI of 34.7. The indication for initial surgery was a genu valgum of 5.6° with IV° cartilage damage in the lateral femoro-tibial compartment. There were no difficulties encountered during the biplane osteotomy, with an opening wedge of 6 mm. She was kept partial weight bearing for six weeks, then stepwise full weight bearing was allowed. After 12, 18 and 24 weeks, though full weight bearing, she still complained about load-dependent pain at the osteotomy site. The radiologic assessment with plain X-rays as well as a CT scan showed no further bone healing (Figs. 2 and 3). Due to the clinical symptoms and the radiological evident stop of bone healing progress, a revision surgery was performed with exchanging the angle plate, debridement of the osteotomy and transplantation of autologous bone graft harvested from the iliac crest. In the following course, the pain disappeared with full weight bearing after six weeks, and the radiologic assessment showed progress in bony healing.
Frontal (a) and sagittal (b) CT scan of the nonunion. White arrow: frontal osteotomy; black arrow: axial osteotomy. Note the absence of dense bone bridging the gap and the sclerotic margins extending along the axial osteotomy margins. c, d Same patient after plate exchange and bone graft interposition
Discussion
LOWDFO is a suitable option in the treatment of valgus knee osteoarthritis and in unloading the lateral knee compartment, especially in the pathological higher lateral distal femoral angle. Still, distal femoral osteotomies are rare compared to HTOs [20]. Our aim was to evaluate the rate of nonunions in LOWDFOs with an angle stable fixation device. Reviewing the current literature, we were surprised at the lack of evidence on this topic as well as the wide range of subsequent recommendations given for LOWDFOs.
One obvious issue is the non-uniform definition of nonunion as well as delayed union in osteotomies. The applied definition is inspired by bone healing after fractures and transferred to osteotomies, irrespective of whether an open or a closed wedge technique is performed. A commonly used definition given by the US Food and Drug Administration (FDA) describes nonunion as a fracture that has not healed within nine months and has not shown radiographic progression for three consecutive months [21]. This time-dependent definition is criticized because the exact time frame likely differs per fractured bone or even location within the bone, soft tissue condition, and fracture type.
A further commonly used definition applied for HTOs as well as in DFOs defines delayed union as an incomplete bony healing after three to six months, and nonunion is stated after six months [22, 23]. However, this definition with an arbitrary use of a temporal limit is flawed. The potential of healing progression as well as the clinical appearance is not taken into consideration. Brinker defines nonunion as a fracture that fails to unite and shows no evidence of further union, resulting in a permanent failure of bone healing [24]. This definition is independent of time, but does not include the clinical appearance. The assessment of a healed fracture largely remains a subjective topic, especially in terms of delayed union. Delayed union is defined as a fracture that requires more healing time than usual. A wide time span that a fracture needs to heal is documented, varying widely between fracture sites and types as well as treatment of fractures. Looking at recent studies using angle stable plates, a healing time of three to 19 months is described for the distal femur [25]. Chapman reported a healing time after revised fracture nonunions of the distal femur at an average of eight months [26], whereas Gardner stated an average time to union within four months [27]. This indicates sufficient bone healing potential of the distal femur in ORIF, where the fracture gap between the fragments is minimized and compression might be achieved. But, the data also implicate that the healing time until consolidation is up to 12 months [28].
Comparing our results with those that exist in literature, we found that defining an osteotomy as healed by using only radiological and time-dependent criteria, especially in an open wedge technique, is not advisable. Taking a closer look at the results and the discussions given in literature, one frequently finds that osteotomies healed without further treatment after nine to 12 months in DFOs.
In an early study of Edgerton et al. in MCWDFO, seven of 20 patients (35%) had a “slow” healing, delayed union was stated in four patients requiring prolonged casting, and three patients developed a nonunion. Although the time period was not clarified, of the patients developing a nonunion, one was treated with casting and electric stimulator, and two patients were treated with bone graft and external fixation. In the end, all osteotomies healed [11]. Saragaglia presented a study of 29 (14 MCDFO, 10 LOWDFO, 5 double osteotomies) osteotomies, using an AO T-shaped plate or an OTIS-F®locking plate [29]. None of their cases had a nonunion. No nonunions or delayed unions in 26 V-shaped osteotomies using the DCS plate was stated by de Carvalho et al. [30].
Looking at LOWDFOs, only few papers exist, mainly retrospective studies with an average case number of 20 osteotomies. A commonly cited study is the one of Jacobi et al. [31]. They abandoned the procedure of LOWDFO due to a high prevalence of delayed unions as well as nonunions. Their retrospective study assessed 14 osteotomies using the Tomofix plate, in which only seven (50%) had a sufficient consolidation at three months, and two (14%) showed persistent insufficient healing at six months. Still, although the clinical symptoms had not been declared, only one of them had to be revised (plate exchange, bone augmentation), the others healed at nine months. This demonstrates the problem in using a time-dependent classification for delayed- and nonunions, resulting subsequently in a high incidence, but without consequences on the clinical outcome. The majority of studies investigating LOWDFOs have low nonunion rates. The group of Ekeland et al. stated in their series of 24 LOWDFOs using the Puddu plate, that 75% of the osteotomies had healed at the three-month follow-up and all at the six-month follow-up [32]. Cameron et al. reported one nonunion (3.2%) requiring revision surgery, and all other 30 osteotomies healed after six months [33]. Saithna had one nonunion in 21 LOWDFOs [34]. Another group comparing intramedullary nailing versus LISS plates in LOWDFO did not report on any nonunions [35].
In our group of LOWDFOs, one female patient (2.4%) had a nonunion requiring revision surgery which was performed 7.2 months after the initial osteotomy. This low nonunion rate is comparable to the data given in literature. A systemic review comparing the lateral opening versus the medial closing wedge technique shows almost identical figures. In lateral open wedge osteotomies, the rate of nonunion was 2.2% (3/138) [36]. For the medial closing wedge technique, they found a rate of 3.8% (6/157) for nonunions, which is even slightly higher than in LOWDFO. Delayed union was seen in 5.8% (8/138) of LOWDFOs, although this criterion, defined as the presence of radiolucent areas within the opening wedge defect, remains strongly subjective in its evaluation and a time-dependent definition has no direct impact on the patients’ clinical course. Although the bone healing potential of the distal femur is high, it appears that the healing process is slow and can take even longer than 12 months. This means that radiolucency can still be seen at the osteotomy gap in a radiological work up, but this does not alter the patients’ clinical course. Though this prolonged healing is evident in distal femur, most of the osteotomies heal within one year. The nonunion rate is proven to be low and comparable with the nonunion rates of MCWDFOs as well as open wedge HTOs. However, for patients who are smokers or in obese patients, the indication should be handled with care since a negative tendency for developing a nonunion was determined.
This study has some shortcomings. Due to the retrospective design, the complication data were collected from the medical records in our clinic as well as from patient comments during follow-up. Furthermore, the sample size of 41 is small. The radiographic assessment of bone union was performed by a single examiner and involved subjective evaluations made by the senior author only. No radiological assessment was performed between 3 and 12 postoperative months in asymptomatic patients. Therefore no statement can be given about the exact time for radiological healing during that time.
Conclusion
With the development of locking plates and the possibility of gaining a good primary stability, a LOWDFO is a safe alternative to MCWDFO. Although the bone healing potential of the distal femur is high, the radiological consolidation of the osteotomy gap appears to be prolonged. However, most of the osteotomies heal unrelieved within one year. The nonunion rate is proven to be low and comparable with the nonunion rates of MCWDFOs as well as open wedge HTOs.
References
Bonasia DE, Dettoni F, Sito G, Blonna D, Marmotti A, Bruzzone M et al (2014) Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med 42(3):690–698
Miller BS, Downie B, McDonough B, Wojtys EM (2009) Complications after medial opening wedge high Tibial osteotomy. Arthroscopy 25(6):639–646
Jackson J (1958) Osteotomy for osteoarthritis of the knee. Proceedings of the Sheffield regional Orthopaedic Club. J Bone Joint Surg Br 40:826
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study J Bone Joint Surg Am 69:332–354
Schatzker J, Burgess R, Glynn M (1985) The management of nonunions following high tibial osteotomy. Clin Orthop Relat Res 193:230–233
Cameron H, Welsh R, Jung Y, Noftall F (1993) Repair of nonunion of tibial osteotomy. Clin Orthop Relat Res 287:167–169
Flamme C, Kohn D, Kirsch L, Hurschler C (1999) Primary stability of different implants used in conjunction with high tibial osteotomy. Arch Orthop Trauma Surg 119:450–455
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11:132–138
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia—early results in 92 cases. Injury 34(Suppl 2):B55–B62
Hoell S, Suttmoeller J, Stoll V, Fuchs S, Gosheger G (2005) The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch Orthop Trauma Surg 125:638–643
Edgerton BC, Mariani EM, Morrey BF (1993) Distal femoral varus osteotomy for painful genu valgum. A five-to-11-year follow-up study. Clin Orthop Relat Res (288):263–9
Mathews J, Cobb AG, Richardson S, Bentley G (1998) Distal femoral osteotomy for lateral compartment osteoarthritis of the knee. Orthopedics 21(4):437–440
Puddu G, Cipolla M, Cerullo G, Franco V, Giannì E (2010) Which osteotomy for a valgus knee? Int Orthop 34(2):239–247
Lobenhoffer P, De Simoni C, Staubli AE (2002) Open wedge high-tibial osteotomy with rigid plate fixation. Tech Knee Surg 1:93–105
Koyonos L, Slenker N, Cohen S (2012) Complications in brief: osteotomy for lower extremity malalignment. Clin Orthop Relat Res 470(12):3630–3636
McDermott AG, Finklestein JA, Farine I, Boynton EL, MacIntosh DL, Gross A (1988) Distal femoral varus osteotomy for valgus deformity of the knee. J Bone Joint Surg Am 70(1):110–116
Healy WL, Anglen JO, Wasilewski SA, Krackow KA (1988) Distal femoral varus osteotomy. J Bone Joint Surg Am 70(1):102–109
Brinkman JM, Hurschler C, Staubli AE, van Heerwaarden RJ (2011) Axial and torsional stability of an improved single-plane and a new bi-plane osteotomy technique for supracondylar femur osteotomies. Knee Surg Sports Traumatol Arthrosc 19(7):1090–1098
van Heerwaarden R, Najfeld M, Brinkman M, Seil R, Madry H, Pape D (2013) Wedge volume and osteotomy surface depend on surgical technique for distal femoral osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):206–212
Dahl A, Lidgren L, Sundberg M, Robertsson O (2015) Introducing prospective national registration of knee osteotomies. A report from the first year in Sweden. Int Orthop 39(7):1283–1288
USFDA (1988) Guidance document for the preparation of investigational device exemptions and pre-market approval applications for bone growth stimulator devices. United States Food and Drug Administration, Rockville
Han JH, Kim HJ, Song JG, Yang JH, Bhandare NN, Fernandez AR, Park HJ, Nha KW (2015) Is bone grafting necessary in opening wedge high Tibial osteotomy? A meta-analysis of radiological outcomes. Knee Surg Relat Res 27(4):207–220
Kolb W, Guhlmann H, Windisch C, Kolb K, Koller H, Grutzner P (2009) Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am 91:2581–2588
Brinker MR (2003) Nonunions: evaluation and treatment. In: Trafton PG (ed) Skeletal Trauma: basic science, management, and reconstruction, 3rd edn. W.B. Saunders, Philadelphia, pp 507–604
Batista B, Salim R, Paccola C, Kfuri M (2014) Internal fixators: a safe option for managing distal femur fractures? Acta Ortop Bras 22(3):159–162
Chapman MW, Finkemeiere CG (1999) Treatment of supracondylar nonunions of the femur with plate fixation and bone graft. J Bone Jt Surg Am 81(A):1217–1228
Gardner MJ, Toro-Arbelaez JB, Harrison M, Hierholzer C, Lorich DG, Helfet DL (2008) Open reduction and internal fixation of distal femoral nonunions: long-term functional outcomes following a treatment protocol. J Trauma 64(2):434–438
Holzman MA, Hanus BD, Munz JW, O’Connor DP, Brinker MR (2016) Addition of a medial locking plate to an in situ lateral locking plate results in healing of distal femoral nonunions. Clin Orthop Relat Res 474(6):1498–1505
Saragaglia D, Chedal-Bornu B (2014) Computer-assisted osteotomy for valgus knees: medium-term results of 29 cases. Orthop Traumatol Surg Res 100(5):527–530
de Carvalho LH Jr, Temponi EF, Soares LF, Gonçalves MB, Costa LP (2014) Physical activity after distal femur osteotomy for the treatment of lateral compartment knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 22(7):1607–1611
Jacobi M, Wahl P, Bouaicha S, Jakob RP, Gautier E (2011) Distal femoral varus osteotomy: problems associated with the lateral open-wedge technique. Arch Orthop Trauma Surg 131:725–728
Ekeland A, Nerhus TK, Dimmen S, Heir S (2016) Good functional results of distal femoral opening-wedge osteotomy of knees with lateral osteoarthritis. Knee Surg Sports Traumatol Arthrosc 24(5):1702–1709
Cameron JI, McCauley JC, Kermanshahi AY, Bugbee WD (2015) Lateral opening-wedge distal femoral osteotomy: pain relief, functional improvement, and survivorship at 5 years. Clin Orthop Relat Res 473:2009–2015
Saithna A, Kundra R, Getgood A, Spalding T (2014) Opening wedge distal femoral varus osteotomy for lateral compartment osteoarthritis in the valgus knee. Knee 21:172–175
Özcan Ç, Sökücü S, Beng K, Çetinkaya E, Demir B, Kabukçuoğlu YS (2016) Prospective comparative study of two methods for fixation after distal femur corrective osteotomy for valgus deformity; retrograde intramedullary nailing versus less invasive stabilization system plating. Int Orthop 40(10):2121–2126
Wylie JD, Jones DL, Hartley MK, Kapron AL, Krych AJ, Aoki SK, Maak TG (2016) Distal femoral osteotomy for the valgus knee: medial closing wedge versus lateral opening wedge: a systematic review arthroscopy. J Arthrosc Relat Surg 32(10):2141–2147
Acknowledgements
All authors confirm that this article was written without direct nor indirect financial support of any corporate bodies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Liska, F., Voss, A., Imhoff, F.B. et al. Nonunion and delayed union in lateral open wedge distal femoral osteotomies—a legitimate concern?. International Orthopaedics (SICOT) 42, 9–15 (2018). https://doi.org/10.1007/s00264-017-3504-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3504-4