Abstract
Purpose
Neutral lower limb alignment does not necessarily produce a horizontal joint line after total knee arthroplasty (TKA). The orientation of the pre- and postoperative tibial mechanical axes (TMAs-G), tibial component, and joint line relative to the ground were evaluated.
Methods
The study group included 46 knees, 23 posterior-stabilized (PS) and 23 bicruciate-stabilized (BCS) TKAs. Using whole-leg standing radiographs, the static orientation of the pre- and postoperative TMAs-G and the tibial component as well as the postoperative alignment were measured. Applying image-matching techniques, the dynamic coronal orientation of the tibial component and joint line over the stance phase of gait were analysed. The correlation between static and dynamic orientation of the tibial component and differences in the joint line between the PS and BCS TKAs were evaluated.
Results
In standing, the postoperative TMA-G (0.8° ± 2.8°) and tibial component (1.5° ± 2.4°) were laterally tilted with a strong correlation. The preoperative lateral tilt of the TMA-G (7.9° ± 5.1°) was a significant predictor of the postoperative TMA-G. The lateral tilt of the tibial component increased to 5.1° ± 2.4° on dynamic analysis, and was moderately correlated to static orientation. The dynamic orientation of the joint line was smaller for the BCS (1.8° ± 2.4°) compared to the PS (5.5° ± 2.7°) TKA.
Conclusion
Even with a mechanically well-aligned TKA, a lateral tilt of the tibial component was identified due to the lateral tilt of the postoperative TMA-G and the stance phase of gait. The BCS can better accommodate the residual lateral tilt of the joint line due to the 3° medial inclination of the joint surfaces of the implant. This study increases the awareness of surgeons regarding the possibility of the coronal joint line orientation to influence preoperative TMA-G and be accommodated by articular surface design, even in mechanically aligned TKA.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has become one of the most successful orthopaedic procedures to provide pain relief and improve knee function in patients with end-stage knee disorders [5, 43]. Moreover, long-term outcomes after TKA have steadily improved as a result of innovations in prosthesis design and surgical techniques [45], with an increasing number of arthroplasty procedures being performed on younger and more physically fit patients [10, 20]. Therefore, concern for revisions due to aseptic mechanical failure in young patients still exist due to their higher activity [30, 37].
One of the key factors for long-term TKA success is to restore the normal alignment of the mechanical axis of the lower extremity and to create a physiological distribution of the loading within the joint [44]. It has been reported that the anatomical joint line forms approximately a 3° varus relative to the mechanical axis of the lower extremity [16]. Moreover, during single leg stance phase in gait, the orientation of the tibial joint line in the coronal plane is parallel to the floor in asymptomatic individuals [14, 44]. With TKAs, it is known that a neutral postoperative lower limb alignment does not necessarily result in a horizontal joint line of the polyethylene articular surfaces [15]. However, the orientation of the postoperative joint line during ambulatory activities has not been evaluated. Therefore, the purpose in this study was to evaluate the static orientation of the pre- and postoperative tibial mechanical axes using radiographic measurement, and the dynamic orientation of the tibial component and the joint line after posterior-stabilized (PS) and bicruciate-stabilized (BCS) TKAs using image-matching techniques. The aim of the study was to answer the following question: are there correlations between the orientations of the tibial component in standing position and during gait, and differences in the orientation of the joint line during gait between different TKA designs? To the best of our knowledge, this is the first study to examine the coronal joint line orientation relative to the ground during gait after TKA using image-matching techniques.
Materials and methods
The study group was comprised of 46 knees in 41 patients. Patients had undergone a clinically successful TKA, with a minimum 12-month follow-up, and were recruited for the study and provided their consent to participate. Patients with a history of fractures around the knee joint, previous arthroplasty, and severe extra-articular deformity were excluded. Relevant pre- and postoperative information of the present study group is presented in Table 1.
Among the 46 knees, in 41 patients, forming the present study group, 23 knees, in 21 patients, had undergone PS fixed-bearing TKA (NexGen Complete Knee Solution Legacy Posterior-Stabilized Knee, Zimmer, Warsaw, IN, USA) and 23 knees, in 20 patients, had undergone BCS fixed-bearing TKA (JOURNEY II, Smith and Nephew, Memphis, TN, USA). The distribution of sex and age was comparable for the BCS and PS TKA groups, with no between-group difference with regard to the fit parameters of the TKA, including postoperative range of motion, pre- and postoperative HKA (hip-knee ankle) angles, and coronal femoral and tibial component angles. The PS TKA has symmetrical femoral condyles and tibial baseplate with symmetrical concave polyethylene articular surfaces, and post-cam mechanism. The BCS TKA has asymmetrical femoral condyles and tibial baseplate with concave medial and convex lateral polyethylene articular surfaces, and anterior and posterior post-cam mechanisms. For the BCS TKA, a 3° medial inclination of the asymmetrical articular surfaces, relative to the tibial baseplate, was implemented by including a 2.5 mm difference in the thickness between the polyethylene insert at the concave medial and convex lateral compartments and between the medial and lateral femoral condyles [6].
Surgical technique
Between 2004 and 2014, all TKAs were performed by the same group of two experienced surgeons, using a similar standardized technique based on the mechanical alignment and the medial para-patellar approach. Using a measured resection technique, the femoral and tibial components were aligned perpendicular to the mechanical axes in the coronal plane by cutting the distal femoral and proximal tibial bone at 90° to their respective mechanical axes with intramedullary and extramedullary instruments, respectively [28]. In the axial plane, the femoral component was aligned along the surgical epicondylar axis [19], with the rotational alignment of the tibial component adjusted to the anteroposterior axis of the tibia [1]. Soft tissue balancing was performed to achieve varus and valgus stability in both extension and flexion.
Radiographic measurements
Pre- and postoperative whole-leg radiographs were taken with the patella facing in a forward position, with the feet straight and at shoulder width (Fig. 1) [24]. The HKA angle was defined as the coronal angle between the mechanical axes of the femur and the tibia [25]. Positive and negative values were expressed as varus and valgus, respectively. For PS TKAs, the coronal femoral angle was defined as the medial angle formed by the mechanical axis of the femur and the horizontal axis of the medial and lateral femoral condyles [26]. For BCS TKAs, the coronal femoral component angle was calibrated by subtracting 3° for built-in lateral inclination of the articular surfaces relative to the distal femoral bone–implant interface. The coronal tibial angle was defined as the medial angle between the mechanical axis of the tibia and the horizontal axis of tibial component [26]. Orientations of the pre- (Fig. 1A) and postoperative tibial mechanical axes (TMAs-G) (Fig. 1B) were defined as the angle between the mechanical axis of the tibia and a line perpendicular to the ground. A positive value was expressed as lateral tilt of the TMA-G. Static orientation of the tibial component was defined as a line drawn along to the tibial tray of the prosthesis and a line parallel to the ground (Fig. 1B) [17]. A positive value was expressed as lateral tilt of the tibial component.
Representative whole-leg standing radiographs for evaluation of the coronal alignment of the knee joint before (A) and after (B) total knee arthroplasty. The static orientation of the tibial mechanical axis (a: TMA-G) relative to a line perpendicular to the ground and the static orientation of the tibial component (b) relative to a line parallel to the ground were evaluated
Kinematic analyses
Gait after TKA was assessed on a level treadmill at a speed of 1.0 km/h, under radiographic surveillance, using a flat-panel detector (FPD: Ultimax-I, Toshiba, Tochigi, Japan: 10 frames per second, image area size 420 (H) × 420 (V) mm, and 0.274 × 0.274 mm/pixel resolution) [13]. The gait cycle was determined using acquired periodic radiographic images, and the data were classified into two main phases (stance and swing phases). The projected three-dimensional (3D) computer-aided design (CAD) model of the tibial component was superimposed onto the serial two-dimensional (2D) radiographic images acquired using the FPD (Fig. 2) [13, 32]. The position of the radiation source relative to the radiograph detector was determined from the projection image of a calibration cage made from an acrylic resin board and metallic balls. Projecting all surface points of the 3D model produced the component silhouette. A model silhouette was matched with the actual object silhouette by translating and rotating the 3D CAD model to minimize the number of unmatched pixels between the silhouettes. Using image-matching techniques with a 3D CAD model of the surfaces of the tibial component and polyethylene insert, the dynamic orientation of the tibial component and the joint line in the coronal plane relative to the ground for both PS (Fig. 3A) and BCS (Fig. 3B) TKAs were evaluated. A positive value in each orientation of the tibial component or joint line was defined as a lateral tilt of the tibial component or joint line relative to the ground, respectively. In terms of measurement accuracy, a previous study estimated the root mean square errors of the position of the tibial component relative to the ground to be 0.28 mm for in-plane translation, 0.21 mm for out-of-plane translation, and 0.17° for rotation [32].
The study protocol was approved by the Institutional Review Board of Kyushu University (IRB number 24-166). Informed consent was obtained from all patients prior to enrollment.
Statistical analyses
Statistical analysis was performed using JMP Software (Version 11.0; SAS Institute Inc., Cary, NC, USA). All values were expressed as the mean ± standard deviation. Welch’s t test and chi-squared tests were used to evaluate differences in demographic and radiographic data between patients with a PS and a BCS TKAs. A multiple linear regression analysis, using a stepwise variable entry method, was performed to evaluate factors associated with the distribution of postoperative TMA-G in standing position. Demographic data (sex, age, BMI, and type of implant) and radiographic data (preoperative TMA-G, postoperative HKA, and coronal femoral and tibial angles) were included in a multivariate logistic regression model. A Spearman’s correlation analysis was used to evaluate the correlations between static orientation measurements of the postoperative TMA-G and tibial component, between the static orientation of the pre- and postoperative TMAs-G, and between the static and dynamic orientations of the tibial component, with correlation analysis using a 95% confidence ellipse [11]. A repeated measures analysis of variance (ANOVA) and post hoc tests (Student’s t test) were used to compare dynamic orientations of the tibial component and joint line during the stance phase of gait between PS and BCS TKAs. Probability values (P values) < 0.05 were considered as statistically significant. A sample size calculation showed that 17 knees in each group would allow detection of a difference of 2.5° (power = 0.8, α = 0.05), with a standard deviation of 2.5° in dynamic orientations of the tibial component and joint line between the two groups.
Results
Postoperative patient-reported outcomes using the 2011 Knee Society Score were as follows: symptoms, 21.3 ± 3.7; satisfaction, 25.5 ± 7.6; and functional activities, 64.6 ± 19.1 (20.8 ± 7.4 in walking and standing) [27, 39, 40]. The static orientation of the pre- and postoperative TMA-G and of the tibial component in standing position showed a lateral tilt of 7.9° ± 5.1°, 0.8° ± 2.8°, and 1.5° ± 2.4°, respectively. The lateral tilt of the tibial component was comparable for PS (1.7° ± 2.1°) and BCS (1.3° ± 2.7°) TKAs (n.s.). The static orientation of the tibial component was strongly correlated to the static orientation of the postoperative TMA-G (r = 0.82, p < 0.0001; Fig. 4A). A significant moderate correlation between the pre- and postoperative static orientation of the TMA-G was also identified (r = 0.42, p = 0.005; Fig. 4B). In the multiple regression analysis, the static orientation of the preoperative TMA-G was identified as an independent factor that was significantly correlated with the static orientation of the postoperative TMA-G (p = 0.0183; Table 2). Sex, age, BMI, type of implant, postoperative HKA, and coronal angles of the femoral and tibial components did not influence measures of static orientation of the postoperative TMA-G (n.s.; Table 2).
Correlation data showing (A) a strong positive linear correlation (r = 0.82, p < 0.0001) between the static orientations of the postoperative tibial mechanical axis (TMA-G) and tibial component; (B) a moderate linear correlation (r = 0.42, p = 0.005) between static orientations of pre- and postoperative TMAs-G; and; (C) a moderate linear correlation (r = 0.48, p = 0.0009) between the static and dynamic orientations of the tibial component
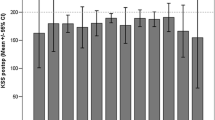
Measurement of the dynamic orientation of the tibial component during the stance phase of gait identified a lateral tilt of 5.1° ± 2.4°, this lateral tilt being 3.6° larger, on average, compared to the static lateral tilt orientation of the tibial component in standing, with a significant moderate correlation between the two measures (r = 0.48, p = 0.0009; Fig. 4C). The dynamic orientation of the tibial component during the stance phase of gait was comparable for the PS and BCS TKAs, with a lateral tilt of 5.5° ± 2.8° and 4.8° ± 2.4°, respectively (n.s.; Fig. 5A). The lateral tilt, measured dynamically during the stance phase of gait, after BCS TKA was 1.8° ± 2.4°, being, on average, 3.6° smaller than the lateral tilt for the PS TKA of 5.5° ± 2.8° (p < 0.0001; Fig. 5B).
Dynamic orientation of the tibial component (A) and joint line (B) relative to the ground in the coronal plane during gait for posterior-stabilized (PS) and bicruciate-stabilized (BCS) total knee arthroplasties (TKAs). Grey and black lines represent PS and BCS TKAs, respectively. The error bars represent 1 standard deviation; *significantly different between PS and BCS TKAs (p < 0.05)
Discussion
The most important finding of the present study was that preoperative TMA-G and articular surface design significantly affect the coronal joint line orientation relative to the ground during gait after TKA. This study characterized the orientation of the tibial component and the joint line, relative to the ground, in standing and during gait. All TKAs were well aligned, with a coronal angle of the tibial component and HKA. Yet, a lateral tilt of the tibial component of 1.5° ± 2.4° in standing and 5.1° ± 2.4° during stance phase of gait relative to the ground was still identified. The orientation of the postoperative TMA-G and the tibial component relative to the ground in standing were strongly correlated (r = 0.82, p < 0.0001). On multiple regression analysis, the preoperative lateral tilt of the TMA-G (7.9° ± 5.1°) was a significant predictor of the postoperative lateral tilt of the TMA-G (0.8° ± 2.8°; p < 0.05). The lateral tilt of the tibial component of 5.1° ± 2.4° identified with measurement of the dynamic orientation was moderately correlated to the static orientation of tibial component (r = 0.48, p < 0.001). Although the coronal alignment was comparable for the two different TKA types, PS and BCS, a significant difference in the orientation of the artificial joint line relative to the ground was identified (5.5° ± 2.8° versus 1.8° ± 2.4°, respectively, p < 0.0001).
Regardless of the coronal angles of the femoral and tibial components relative to the mechanical axes, the orientation of the tibial component showed a valgus tilt, with some variability due to the lateral tilt of the postoperative TMA-G, in standing. Although it is well recognized that a neutral lower limb alignment with the mechanically aligned TKA does not necessarily yield a horizontal joint line, patient characteristics and radiographic parameters associated with the variability in postoperative TMA-G alignment have not previously been reported. Using multiple regression analysis, a significant correlation between pre- and postoperative TMA-G alignment measures in standing was identified. Norton et al. suggested that residual malalignment of the TMA-G may be caused by an inability of the subtalar joint to reorient itself after knee realignment due to the fixed hindfoot deformity in patients with advanced knee OA with a varus deformity [12, 35]. Okamoto et al. also reported that the postoperative hindfoot alignment remained in valgus after TKA in patients with a severe varus deformity of the knee preoperatively [36]. Therefore, surgeons should recognize that a pre-existing stiff subtalar joint could induce additional lateral tilting of the TMA-G postoperatively and prevent restoration of the alignment of the joint line parallel to the floor, despite effective correction of the preoperative knee deformity.
Image-matching techniques could provide relevant information regarding the dynamic change in the orientation of the tibial component and the radiolucent artificial joint line relative to the ground. 3D dynamic evaluation during gait, which quantified the load distribution on the knee over multiple cycles performed in daily life, can inform us on how the knee prosthesis is being functionally loaded. Although the kinematics of the femoral component relative to the tibial component has now been well described over functional activities [23], few studies have addressed how the tibial component, which holds up the femoral component, is oriented relative to the ground during dynamic weight-bearing activities. Based on this study sample, an increase in the lateral tilt of the tibial component of 3.6° with dynamic orientation measurement was reported during the stance phase of gait compared to the static orientation in standing (1.5° versus 5.1°). As described in previous studies, adduction of the lower extremity over the stance phase of gait can be attributed to the lateral movement of the centre of gravity over the stance foot [21]. Complex interactions of multiple factors, including tibiofemoral forces, active muscle contraction, ligaments, and constrains of the surrounding soft tissues produce dynamic knee stability [3]. Previous kinematic analyses have confirmed the absence of a significant lift-off with a well-balanced and -aligned TKA [22] when performed using measured resection [14] or a gap-balancing technique [9, 31].
Additionally, the influence of two TKA designs, the PS and BCS, on the in vivo orientation of the articular joint line was compared. The BCS TKA incorporates an asymmetrical geometry of polyethylene articular surfaces, with a 3° medial incline [23]. Therefore, the BCS TKA may bring the artificial joint line into a more optimal orientation parallel to the ground during the stance phase of gait compared to the PS TKA. As far as we know, this is the first study showing the above-mentioned differences between PS and BCS TKAs. Thienpont et al. recently reported that obtaining a neutral mechanical axis with a joint line parallel to the floor and a central alignment of the load-bearing axis remains the primary goals for surgeons [41]. However, although early mechanical failure has not been reported, surgeons remain concerned that a kinematic alignment of the TKA that recreates a patient’s pre-arthritis articular surface anatomy, also known as constitutional varus, might increase the risk for patellofemoral complications, including an increase stress on the medial tibia for cases with a severe knee varus deformity [33]. It was demonstrated that the BCS lends itself to a better orientation of the joint line, horizontal to the floor, when compared to the PS TKA, using the same standard TKA technique. In healthy knees, the tibial joint line is parallel to the floor in the coronal plane during ambulatory activities [14, 45]. Therefore, the option of using tibial or femoral or even double osteotomies to achieve an optimal medial–lateral slope of the joint line has been discussed [2, 4]. Certainly, the wear of the ultrahigh molecular weight polyethylene (UHMWPE) insert in TKAs has been significantly improved through advances in implant design [34, 42], the mechanical properties of the fabricated material and by reducing the potential for long-term oxidation after implantation [7, 29]. However, achieving a horizontal joint line orientation with a neutral mechanical axis can still, theoretically, be expected to decrease shear force at the tibiofemoral articulation and the tension on the collateral ligament after cruciate-sacrificing TKA, resulting in restoration of natural knee joint kinematics [44] and subsequent improvement in patient-reported functional outcomes [18, 38].
The limitations of the present study should be considered in the interpretation of these results. First, this is a retrospective study of a non-randomized cohort, and selection bias is present in the surgical allocation of patients into each group. However, patients’ demographics and coronal implant alignment were relatively similar between the two TKA groups. It is readily evident that there are differences in the joint line orientation between the two designs with different tibiofemoral articular surface geometries. Second, dynamic data averaged throughout bipedal and monopedal stance phases were compared to the static data in the bipedal standing position. Previous studies have demonstrated that knee alignment was dynamic and changed with different postures and across varying degrees of weight bearing [8]. Third, as mentioned in the initial part of discussion, foot and ankle angles would affect the orientation of the leg, tibia, and joint line in relation to the ground. Fourth, this study did not evaluate whether a parallel orientation of the artificial joint line relative to the ground provides better joint loading and shear stress in each TKA. Additional studies are required to analyse the force distribution under dynamic conditions with ligamentous constraint using loading simulators or finite element model. While the horizontal artificial joint line of the BCS TKAs may be good in short-term follow-up, the convex lateral articular surface may have the potential of higher degree of polyethylene wear. Therefore, further investigation will be necessary to determine the long-term clinical outcomes.
Conclusion
A lateral tilt of the tibial component of 1.5° relative to the ground was identified in standing position and related to the lateral tilt of the postoperative TMA-G, which, itself, was significantly correlated to the preoperative TMA-G. Gait induced a significant 3.6° increase in the lateral tilt of the tibial component (5.1°) relative to the ground, compared to standing. The BCS TKA design significantly decreased the lateral tilt of the artificial joint line compared to the PS design due to the 3° of medial inclination of the articular surfaces of the implant. This study increases awareness among surgeons that mechanically well-aligned TKA tends to show a lateral tilt of the tibial component relative to the ground during gait, and that both preoperative TMA-G and articular surface design could influence the coronal joint line orientation relative to the ground.
References
Akagi M, Mori S, Nishimura S, Nishimura A (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Amis AA (2013) Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21:197–205
Andriacchi TP, Stanwyck TS, Galante JO (1986) Knee biomechanics and total knee replacement. J Arthroplasty 1:211–219
Babis GC, An KN, Chao E, Rand JA, Sim FH (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity: clinical results. J Bone Joint Surg Am 84A:1380–1388
Callaghan JJ, O’Rourke MR, Iossi MF, Liu SS, Goetz DD, Vittetoe DA, Sullivan PM, Johnston RC (2005) Cemented rotating-platform total knee replacement: a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg Am 87:1995–1998
Catani F, Ensini A, Belvedere C, Feliciangeli A, Benedetti MG, Leardini A, Giannini S (2009) In vivo kinematics and kinetics of a bi-cruciate substituting total knee arthroplasty: a combined fluoroscopic and gait analysis study. J Orthop Res 27:1569–1575
Chakrabarty G, Vashishtha M, Leeder D (2015) Polyethylene in knee arthroplasty: a review. J Clin Orthop Trauma 6:108–112
Deep K, Eachempati KK, Apsingi S (2015) The dynamic nature of alignment and variations in normal knees. Bone Joint J 97-B:498–502
Dennis DA, Komistek RD, Kim RH, Sharma A (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468:102–107
Duffy GP, Crowder AR, Trousdale RR, Berry DJ (2007) Cemented total knee arthroplasty using a modern prosthesis in young patients with osteoarthritis. J Arthroplasty 22:67–70
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185:1332–1338
Gursu S, Sofu H, Verdonk P, Sahin V (2016) Effects of total knee arthroplasty on ankle alignment in patients with varus gonarthrosis: do we sacrifice ankle to the knee? Knee Surg Sports Traumatol Arthrosc 24:2470–2475
Hamai S, Miura H, Okazaki K, Shimoto T, Higaki H, Iwamoto Y (2014) No influence of coronal laxity and alignment on lift-off after well-balanced and aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:1799–1804
Hamai S, Okazaki K, Ikebe S, Murakami K, Higaki H, Nakahara H. Shimoto T, Mizu-uchi H, Akasaki Y, Iwamoto Y (2016) In vivo kinematics of healthy and osteoarthritis knees during stepping using density-based image-matching techniques. J Appl Biomech 32:586–592
Hungerford DS, Kenna RV (1983) Preliminary experience with a total knee prosthesis with porous coating used without cement. Clin Orthop Relat Res 176:95–107
Hungerford DS, Krackow KA (1985) Total joint arthroplasty of the knee. Clin Orthop Relat Res 192:23–23
Hutt J, Massé V, Lavigne M, Vendittoli PA (2016) Functional joint line obliquity after kinematic total knee arthroplasty. Int Orthop 40:29–34
Ji HM, Han J, Jin DS, Seo H, Won YY (2016) Kinematically aligned TKA can align knee joint line to horizontal. Knee Surg Sports Traumatol Arthrosc 24:2436–2441
Kawahara S, Matsuda S, Okazaki K, Tashiro Y, Mitsuyasu H, Nakahara H, Iwamoto Y (2012) Relationship between the tibial anteroposterior axis and the surgical epicondylar axis in varus and valgus knees. Knee Surg Sports Traumatol Arthrosc 20:2077–2081
Keeney JA, Eunice S, Pashos G, Wright RW, Clohisy JC (2010) What is the evidence for total knee arthroplasty in young patients? A systematic review of the literature. Clin Orthop Relat Res 469:574–583
Kozanek M, Hosseini A, Liu F, Van de Velde SK, Gill TJ, Rubash HE, Li G (2009) Tibiofemoral kinematics and condylar motion during the stance phase of gait. J Biomech 42:1877–1884
Kuriyama S, Ishikawa M, Nakamura S, Furu M, Ito H, Matsuda S (2016) No condylar lift-off occurs because of excessive lateral soft tissue laxity in neutrally aligned total knee arthroplasty: a computer simulation study. Knee Surg Sports Traumatol Arthrosc 24:2517–2524
Kuroyanagi Y, Mu S, Hamai S, Robb WJ, Banks SA (2012) In vivo knee kinematics during stair and deep flexion activities in patients with bicruciate substituting total knee arthroplasty. J Arthroplasty 27:122–128
Lee YS, Lee BK, Lee SH, Park HG, Jun D-S, Moon DH (2013) Effect of foot rotation on the mechanical axis and correlation between knee and whole leg radiographs. Knee Surg Sports Traumatol Arthrosc 21:2542–2547
Lindstrand A, Boegard T, Egund N, Thorngren KG (1982) Use of a guide instrument for compartmental knee arthroplasty. Acta Orthop Scand 53:633–639
Mahaluxmivala J, Bankes MJ, Nicolai P, Aldam CH, Allen PW (2001) The effect of surgeon experience on component positioning in 673 Press Fit Condylar posterior cruciate-sacrificing total knee arthroplasties. J Arthroplasty 16:635–640
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y (2013) Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res 471:127–133
Matsuda S, Mizu-uchi H, Miura H, Nagamine R, Urabe K, Iwamoto Y (2003) Tibial shaft axis does not always serve as a correct coronal landmark in total knee arthroplasty for varus knees. J Arthroplasty 18:56–62
Medel FJ, Martínez-Morlanes MJ, Alonso PJ, Rubín J, Pascual FJ, Puértolas JA (2013) Microstructure, thermooxidation and mechanical behavior of a novel highly linear, vitamin E stabilized, UHMWPE. Mater Sci Eng C Mater Biol Appl 33:182–188
Meehan JP, Danielsen B, Kim SH, Jamali AA, White RH (2014) Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty. J Bone Joint Surg Am 96:529–535
Moro-oka T-A, Shiraishi H, Iwamoto Y, Banks SA (2009) Modified gap-balancing technique in total knee arthroplasty: evaluation of the post-operative coronal laxity. Knee Surg Sports Traumatol Arthrosc 18:375–380
Nakahara H, Okazaki K, Hamai S, Kawahara S, Higaki H, Mizu-uchi H, Iwamoto Y (2015) Rotational alignment of the tibial component affects the kinematic rotation of a weight-bearing knee after total knee arthroplasty. Knee 22:201–205
Nakamura S, Tian Y, Tanaka Y (2017) The effects of kinematically aligned total knee arthroplasty on stress at the medial tibia. Bone Joint Res 6:43–51
Nishikawa K, Okazaki K, Matsuda S, Tashiro Y, Kawahara S, Nakahara H, Okamoto S, Shimoto T, Higaki H, Iwamoto Y (2014) Improved design decreases wear in total knee arthroplasty with varus malalignment. Knee Surg Sports Traumatol Arthrosc 22:2635–2640
Norton AA, Callaghan JJ, Amendola A, Phisitkul P, Wongsak S, Liu SS, Fruehling-Wall C (2014) Correlation of knee and hindfoot deformities in advanced knee OA: compensatory hindfoot alignment and where it occurs. Clin Orthop Relat Res 473:166–174
Okamoto Y, Otsuki S, Jotoku T, Nakajima M, Neo M (2016) Clinical usefulness of hindfoot assessment for total knee arthroplasty: persistent post-operative hindfoot pain and alignment in pre-existing severe knee deformity. Knee Surg Sports Traumatol Arthrosc 19:211–218
Parvizi J, Nunley RM, Berend KR, Lombardi AV, Ruh EL, Clohisy JC, Hamilton WG, Valle Della CJ, Barrack RL (2013) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472:133–137
Rames RD, Mathison M, Meyer Z, Barrack RL, Nam D (2017) No impact of under-correction and joint line obliquity on clinical outcomes of total knee arthroplasty for the varus knee. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-017-4507-9
Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WN (2011) The new knee society knee scoring system. Clin Orthop Relat Res 470:3–19
Taniguchi N, Matsuda S, Kawaguchi T, Tabara Y, Ikezoe T, Tsuboyama T, Ichihashi N, Nakayama T, Matsuda F, Ito H (2015) The KSS 2011 reflects symptoms, physical activities, and radiographic grades in a Japanese population. Clin Orthop Relat Res 473:70–75
Thienpont E, Cornu O, Bellemans J, Victor J (2015) Current opinions about coronal plane alignment in total knee arthroplasty: A survey article. Acta Orthop Belg 81:471–477
Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ (2006) The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res 452:28–34
Victor J, Bellemans J (2006) Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res 452:53–58
Victor JMK, Bassens D, Bellemans J, Gürsu S, Dhollander AAM, Verdonk PCM (2013) Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 472:98–104
Victor J, Ghijselings S, Tajdar F, Van Damme G, Deprez P, Arnout N, Van Der Straeten C (2014) Total knee arthroplasty at 15–17 years: does implant design affect outcome? Int Orthop 38:235–241
Acknowledgements
This work was supported by a Grant of Kaibara Morikazu Medical Science Promotion Foundation. We thank Junji Kishimoto, a statistician from the Digital Medicine Initiative at Kyushu University, for his valuable comments and suggestions in regard to statistical analyses.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
The study protocol was approved by the Institutional Review Board of Kyushu University (IRB number 24-166). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Murakami, K., Hamai, S., Okazaki, K. et al. Preoperative tibial mechanical axis orientation and articular surface design influence on the coronal joint line orientation relative to the ground during gait after total knee arthroplasties. Knee Surg Sports Traumatol Arthrosc 26, 3368–3376 (2018). https://doi.org/10.1007/s00167-018-4899-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-4899-1