Abstract
Purpose
Proper rotational alignment in total knee arthroplasty (TKA) is essential for successful outcomes. The surgical epicondylar axis (SEA) has been frequently used to determine the femoral rotational alignment, and the anteroposterior (AP) axis of the tibia described in previous study has been introduced as a line perpendicular to the SEA in healthy knees. However, the rotational relationship between the distal femur and the proximal tibia would vary between normal and osteoarthritic knees, and a question remains whether the rotational relationship between the SEA and the AP axis of the tibia would be the same between normal and osteoarthritic knees. This study aims to determine whether the AP axis of the tibia is actually perpendicular to the SEA and useful for the tibial rotational alignment also in osteoarthritic knees.
Methods
Preoperative computed tomography scans on 25 varus and 25 valgus knees undergoing TKA were studied. The SEA and the AP axis of the tibia were identified using a three-dimensional software, and the angle between the line perpendicular to the projected SEA and the AP axis was measured.
Results
The AP axis of the tibia was 1.7° ± 4.3° and 2.0° ± 4.0° internally rotated relative to the line perpendicular to the SEA in the varus and valgus groups, respectively.
Conclusions
The AP axis of the tibia was, on average, perpendicular to the SEA in both varus and valgus knees. The AP axis would be useful for setting the tibial component with minimal rotational mismatch.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reconstruction of the mechanical leg axis in the coronal and sagittal plane is a major requirement in total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA) [7, 10, 15]. However, proper femoral and tibial component rotational positioning is also essential for successful TKA. Positioning is key as the consequences of malrotation would produce patellofemoral problems [2, 6, 8, 19, 22], flexion instability [6], ultra-high molecular weight polyethylene or post-wear [16, 22, 27], stiffness [23], and abnormal gait patterns [26].
The surgical epicondylar axis (SEA), the line connecting the tip of the lateral epicondyle to the medial epicondylar sulcus, has been shown to be not only a useful anatomic reference axis but also a functional flexion–extension axis [9, 17, 20, 21, 29]. In contrast to the femoral side, several references are used to determine tibial rotational orientation. The anteroposterior (AP) axis connecting the middle of the posterior cruciate ligament (PCL) to the medial border of the patellar tendon at the attachment level described by Akagi et al. has been introduced as a reproducible and reliable line perpendicular to the SEA in healthy knees [3, 4]. However, the rotational relationship between the distal femur and the proximal tibia in knee extended position would vary between normal and osteoarthritic knees [12]. Therefore, a question remains as to whether the AP axis of the tibia is actually perpendicular to the SEA in osteoarthritic knees. Moreover, it is well known that valgus knees have hypoplastic posterolateral condyle [18], and it is much more unclear in valgus knees whether the AP axis of the tibia is perpendicular to the SEA.
The objective of the current study is to identify whether the AP axis of the tibia is perpendicular to the SEA and useful for the tibial rotational alignment also in osteoarthritic knees based on preoperative computed tomography (CT) scan data.
Materials and methods
This study was approved by the institutional review board (Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan, No. 21-8). Informed consent for participation was obtained from all patients. We obtained preoperative knee CT scans on 52 patients with primary varus osteoarthritis (varus angle: median 10.0°, range 0.5°–22.5°) and on 28 patients with primary valgus osteoarthritis (valgus angle: median 6.3°, range 0.3°–25.0°) undergoing TKA. Postoperative knees displaying intra-articular osteosynthesis, high tibial osteotomies and unicompartmental knee arthroplasties were excluded from the study. The patients were all Japanese.
The patients were placed in the supine position on the scanning table and the affected knee was naturally extended without any feeling of internal or external rotation. Transverse CT scans were taken at the levels ranging from the hip joint to the ankle joint at 2-mm intervals. CT images were acquired as DICOM data from the CT system server. A three-dimensional (3D) image of the lower extremity was reconstructed on the computer using the program 3D template (version 02.02.02, Japan Medical Matls. Corp., Osaka, Japan). An axial plane was defined perpendicular to the tibial mechanical axis. The flexion angle of the knee was defined as the angle between the femoral mechanical axis and the tibial mechanical axis.
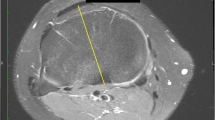
The tip of the lateral epicondyle and the medial epicondylar sulcus were identified, and the SEA was drawn. In eight varus knees and four valgus knees, the medial epicondylar sulcus could not be recognized on CT scans. In these subjects, the clinical epicondylar axis (CEA) connecting the most prominent point of the medial epicondyle and the lateral epicondyle was identified, and the SEA assumed as a line rotating the CEA internally by 3° [5, 28]. For the AP axis of the tibia, the middle of the PCL at the tibial attachment (Fig. 1a) and the medial border of the patellar tendon at the attachment level (Fig. 1b) were identified.
a The middle of the PCL at the tibial attachment (white circle) was identified. b. The AP axis of the tibia, the SEA and the line perpendicular to the SEA were drawn (two solid line and one dotted line, respectively), and the angle between the line perpendicular to the SEA and the AP axis was measured
The SEA and the AP axis were projected onto a plane of the patellar tendon attachment at the tibia perpendicular to the tibial mechanical axis, and the angle between the line perpendicular to the projected SEA and the AP axis was measured (Fig. 1b). All the angles were measured in the computer program 3D template and the program allowed one decimal.
Statistical analysis
Seven patients in the varus group and three patients in the valgus group with a flexion contracture greater than 15° were excluded as this would have resulted in an altered reciprocal rotational position between the femur and tibia. Patients in the varus group were matched with the valgus group as often as possible based on knee extension angle, gender and the hip-knee-ankle angle (HKA, the angle between the femoral and tibial mechanical axis). Setting an order of priority described above, the matched 25 varus knees were extracted (Table 1).
All the measurement procedures were repeated three times at least a week apart by one examiner (SK) for all patients, and the average of three measurements was adopted as data. To evaluate the intra-observer and interobserver reproducibility, the measurement was performed three times by one examiner (SK) and once by two examiners (HM, HN) on the 10 knees randomly selected from the study group. The intraclass correlation coefficient and the interclass correlation coefficient were 0.90 and 0.89 for measurement of the angle between the line perpendicular to the projected SEA and the AP axis of the tibia.
Results
The parameters of the varus and valgus groups were shown in Table 1 and all of them were not significantly different.
The AP axis of the tibia was 0.6° (median) internally rotated in the varus group and 2.6° (median) internally rotated in the valgus group relative to the line perpendicular to the SEA (Fig. 2).
Discussion
The most important finding of the present study was that the AP axis of the tibia was almost perpendicular to the SEA in both varus and valgus knees. Aglietti et al. [1] measured the angle between the line perpendicular to the SEA and the AP axis of the tibia (tibial rotation angle) in a manner similar to the current study in 100 osteoarthritic knees including varus and valgus knees. The tibial rotation angle was 0.1° ± 3.3° in men and 0.0° ± 3.9° in women, respectively. In that study, however, it was unclear whether the AP axis was actually perpendicular to the SEA in varus and valgus knees because their subjects were not divided into each group. Anatomical data of the knee should be evaluated separately in varus and valgus knees [24]. Because valgus knees have hypoplastic posterolateral condyle, it is much more unclear whether rotational relationship is the same in normal and valgus knees. The results of the current study suggested that the AP axis would be applicable as a tibial rotational reference in varus and valgus knees when performing TKA.
To avoid rotational mismatch, surgeons can make appropriate corrections of the tibial rotational alignment with trial components. However, the proximal tibia should be cut in the same direction of the tibial component position when the tibia is prepared with some degree of posterior slope. If the rotational direction of the tibial cutting procedure is different from the rotational position of the tibial component, the component would be malaligned in varus or valgus due to its tibial posterior slope [14]. Therefore, the tibial rotational alignment should be determined before cutting the proximal tibia. In this respect, the AP axis is believed to be useful when deformities exist.
Whether the same rotational relationship exists before and after surgery is another important clinical question. Relative rotational position between the distal femur and the proximal tibia is determined by many factors such as the articular configuration [11], the ligamentous tension and the muscle traction. Tight soft tissue structures have been released during TKA, and the current prosthetic design does not have a constrained articulation. Therefore, tendon attachment location such as the tibial tuberosity is a major factor for determining the rotational relationship between the distal femur and the proximal tibia after TKA. Since the location of the tendon attachment does not change by surgery, we believe the rotational position would not significantly change perioperatively.
There are several limitations to this study. First, we evaluated a limited number (25 knees) of valgus knees. Secondly, some knees evaluated in the study were not able to reach full extension in the CT scanner due to flexion contractures greater than 15° (seven varus knees and three valgus knees); therefore, they were excluded in the study. These slight flexion angles would have possibly affected the reciprocal rotational position between the femur and tibia. Thirdly, this study has been performed under the static knee condition. However, the rotational relationship between the femoral and tibial components is generally confirmed in knee extended position during surgery, and it is dependent principally on the articular configuration, the ligamentous tension and the muscle traction under the dynamic knee condition. Therefore, it is basically important that the rotational positions of each component are determined in knee extended position. Additionally, the study population was limited to Japanese subjects. The study described by Akagi et al. also included Japanese subjects, and our study is in agreement with their study in this respect. However, it is possible that the data included in the current study would be typical only for knees of Japanese subjects and therefore there would be anatomic differences from the Caucasian population [13, 25]. Therefore, one should interpret the results of this study cautiously.
Conclusion
We investigated that the AP axis of the tibia was, on average, almost perpendicular to the SEA in varus and valgus knees. The clinical relevance of the present study is that the AP axis can be used as a tibial rotational reference in varus as well as valgus knees to minimize the risk for rotational mismatch between the femoral and tibial components.
References
Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755
Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T (1999) Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 366:155–163
Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C (2005) Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 436:172–176
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Akagi M, Yamashita E, Nakagawa T, Asano T, Nakamura T (2001) Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res 388:147–156
Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT (1993) The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 287:170–177
Bauwens K, Matthes G, Wich M, Gebhard F, Hanson B, Ekkernkamp A, Stengel D (2007) Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am 89:261–269
Berger RA, Crossett LS, Jacobs JJ, Rubash HE (1998) Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 356:144–153
Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS (1993) Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 286:40–47
Bruni D, Iacono F, Russo A, Zaffagnini S, Marcheggiani Muccioli GM, Bignozzi S, Bragonzoni L, Marcacci M (2010) Minimally invasive unicompartmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients. Knee Surg Sports Traumatol Arthrosc 18:710–717
Casino D, Martelli S, Zaffagnini S, Lopomo N, Iacono F, Bignozzi S, Visani A, Marcacci M (2009) Knee stability before and after total and unicondylar knee replacement: in vivo kinematic evaluation utilizing navigation. J Orthop Res 27:202–207
Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD (1994) Version of the osteoarthritic knee. J Arthroplasty 9:73–79
Hovinga KR, Lerner AL (2009) Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J Orthop Res 27:1191–1196
Insall JN, Easley ME (2001) Surgical techniques and instrumentation in total knee arthroplasty. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill Livingstone, New York, pp 1553–1620
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg Br 73:709–714
Lewis P, Rorabeck CH, Bourne RB, Devane P (1994) Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop Relat Res 299:11–17
Mantas JP, Bloebaum RD, Skedros JG, Hofmann AA (1992) Implications of reference axes used for rotational alignment of the femoral component in primary and revision knee arthroplasty. J Arthroplasty 7:531–535
Matsuda S, Miura H, Nagamine R, Mawatari T, Tokunaga M, Nabeyama R, Iwamoto Y (2004) Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res 22:104–109
Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg 14:152–156
Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE (2001) Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res 392:38–45
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am 69:745–749
Nagamine R, Whiteside LA, White SE, McCarthy DS (1994) Patellar tracking after total knee arthroplasty. The effect of tibial tray malrotation and articular surface configuration. Clin Orthop Relat Res 304:262–271
Su EP, Su SL, Della Valle AG (2010) Stiffness after TKR: how to avoid repeat surgery. Orthopedics 33:658
Sun T, Lu H, Hong N, Wu J, Feng C (2009) Bony landmarks and rotational alignment in total knee arthroplasty for Chinese osteoarthritic knees with varus or valgus deformities. J Arthroplasty 24:427–431
Urabe K, Mahoney OM, Mabuchi K, Itoman M (2008) Morphologic differences of the distal femur between Caucasian and Japanese women. J Orthop Surg 16:312–315
Verlinden C, Uvin P, Labey L, Luyckx JP, Bellemans J, Vandenneucker H (2010) The influence of malrotation of the femoral component in total knee replacement on the mechanics of patellofemoral contact during gait: an in vitro biomechanical study. J Bone Joint Surg Br 92:737–742
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 299:31–43
Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y (2001) Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty 16:493–497
Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Joint Surg Am 69:873–880
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawahara, S., Matsuda, S., Okazaki, K. et al. Relationship between the tibial anteroposterior axis and the surgical epicondylar axis in varus and valgus knees. Knee Surg Sports Traumatol Arthrosc 20, 2077–2081 (2012). https://doi.org/10.1007/s00167-011-1826-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1826-0