Abstract
Purpose
Few studies have used MRI to identify the ALL. As it was shown that it is not possible to precisely characterize this ligament in all examination, it is important to identify concomitant lesions that can help in diagnosing ALL abnormalities. It is important to characterise this injury due to its association with anterolateral knee instability. Thus, the present study was performed to determine the frequency of ALL injuries in patients with acute ACL rupture and to analyse its associated knee lesions.
Methods
Patients with acute ACL injuries were evaluated by MRI. Among this population, the ALL was classified as non-visualised, injured or normal. The possible abnormalities of the meniscus, collateral ligaments, popliteus tendon, posterior cruciate ligament, Iliotibial band (ITB), anterolateral capsule and osseus injuries were evaluated. The association of an ALL injury with these other knee structures as well as sex and age was calculated.
Results
Among the 228 knees evaluated, the ALL could not be entirely identified in 61 (26.7%). Of the remaining 167, 66 (39.5%) presented an ALL abnormality and only four (6.1%) were Segond fractures. ALL abnormalities were associated with lesions of the lateral collateral ligament, medial collateral ligament, popliteus tendon, ITB, anterolateral capsule and osseous contusions of the femoral condyle and tibial plateau. No correlation was found with medial meniscus, lateral meniscus and posterior cruciate ligament injuries. There was no association between ALL injuries and gender, and older patients were more likely to present an ALL injury.
Conclusion
ALL injuries are present in approximately 40% of ACL injuries, and a minority of these are Segond fractures. These injuries are associated with peripheral ligament injuries, anterolateral structures lesions and bone contusions, but there is no association with meniscal injuries. Surgeons must be aware of these associations to consider an ALL lesion even if it is not completely clear in imaging evaluation, especially if a high degree of anterolateral instability is present on physical examination.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Anterolateral knee structures have their importance better recognised recently due to anatomical studies of the “newly discovered” anterolateral ligament (ALL) [1–6]. Damage to the ALL may be responsible for cases of isolated anterior cruciate ligament (ACL) injury that do not progress satisfactorily after isolated intra-articular reconstruction [7–11].
Following these anatomical studies, several researchers have tried to characterise the ALL using magnetic resonance imaging (MRI) in an attempt to establish protocols for diagnosing ALL injuries [1, 12–16]. Despite the presence of various structures in the anterolateral knee region, correlational studies of the anatomy with MRI have shown that it is possible to characterise the ALL [1, 17], but researchers have had difficulties in characterising the ALL along its entire length. Studies attempting to characterise ALL injuries in acute ACL injuries are scarce, characterisation is difficult and non-visualisation indices range between 13 and 24%. Therefore, the epidemiology of these injuries needs to be further clarified [18–21].
Due to the difficulty in characterising the ALL using MRI [18–21], the inability to identify the ALL completely using arthroscopy due to its extra-articular location [2, 3, 22], the variation in dissection methods and cadaver preparation, the inconsistent terminology, the lack of agreement as to the precise anatomic location of the ALL [1–3, 5, 6, 15, 22–29] and the lack of a defined correlation between physical examination tests and ALL damage (although there appears to be an association with the pivot shift test according to Song et al. [30]), other tools need to be developed to aid in correctly diagnosing ALL injury. For ACL injuries, when there is diagnostic uncertainty on MRI, indirect signs of injury may be used [31]. In addition to indirect signs, associated injuries such as the Segond avulsion fractures can be important diagnostic tools [31].
The aim of this study was therefore to evaluate the frequency of ALL abnormalities in acute ACL injuries and to characterise other possible intra- and extra-articular knee injuries that occur in association with ALL injuries. As a secondary objective, we will evaluate whether there is a relationship between ALL abnormalities and complete and partial ACL injuries. It was hypothesised that a significant amount of ALL abnormalities would be found and these would be associated with lateral meniscus and lateral collateral ligament injuries. The diagnostic of sentinel injuries for an ALL injury is new and can make surgeons aware of an ALL lesion even if it is not completely clear in imaging evaluation.
Materials and methods
All knee MRI examinations performed at our institution for a period of 12 months, from January 1 to December 31, 2015, with acute ACL injury being prospectively evaluated. The MRI exams were enrolled prospectively as well as the data gathering and then they were evaluated retrospectively.
Patients with signs of acute injury to at least one of the ACL bands on MRI evaluation and whose history of trauma was less than 3 weeks prior to the examination were included. The age range for inclusion was 15–60 years old. Patients with previous knee surgery, known previous knee injuries, previous infection of the knee or with any artefact on the images, mainly related to patient movements during the exam, that could compromise evaluation of the desired structures, were excluded.
The MRI examinations were performed on 1.5 T (Aera, Siemens Medical Solutions, Erlangen, Germany; Espree, Siemens Medical Solutions, Erlangen, Germany; Avanto, Siemens Medical Solutions, Erlangen, Germany; GE Optima 450 W, GE Healthcare, Milwaukee, United States) and 3.0 T (Achieva, Philips Medical Systems, Best, the Netherlands; Skyra, Siemens Medical Solutions, Erlangen, Germany; GE HDX, GE Healthcare, Milwaukee, United States) devices. The MR imaging protocol of our institution is described in Table 1.
The MRI studies were evaluated by two radiologists with training and experience in musculoskeletal disorders and specific training in the evaluation of the ALL, which included participation in anatomical dissections and MRI studies with emphasis on viewing of the anterolateral knee structures. Each evaluator reviewed the exams twice with 30–40 days between the evaluations. The more experienced radiologist was considered the main evaluator and the less experienced served to determine the interobserver correlation for the data obtained. The evaluators did not have any data about physical examination findings at the time of the MRI review.
The following were considered ALL abnormalities: any obvious discontinuity in the ALL fibres and irregular contours associated with periligamentous oedema or proximal or distal detachment, with or without associated bone fragments, so that ALL was classified as normal or abnormal dichotomously. The ALL was defined with origin from the lateral epicondyle to posterior and proximal to it as was described in a specific study about the ALL femoral origin [22] and with insertion between Gerdy’s tubercle and the fibular head [1–3, 5, 6, 25]. Abnormality parameters were based on knowledge of imaging evaluations of other ligaments and on previous studies of this structure [18, 20, 21].
In addition to the ALL, the following were evaluated: the presence of possible injuries to or abnormalities of the medial and lateral menisci, the presence of bone contusions in the lateral and medial tibial plateaus and femoral condyles and the presence of abnormalities in the lateral collateral ligament (LCL), medial collateral ligament (MCL), PCL, popliteus muscle tendon (PT), anterolateral capsule and ITB. Anterolateral capsule injuries were considered if there was a presence of fluid or focal oedema in the anterolateral insertion of the joint capsule, and ITB abnormalities were considered based on the definition by Mansour et al. [32], defined as normal, minor sprain, severe sprain and torn.
To verify the association of an ALL lesion with anterolateral rotatory instability, medical records of the patients were evaluated and the degree of rotatory instability through the pivot shift test was compared to the presence of an ALL abnormality in the MRI exams.
The study was approved by the ethics committee of the institution (CEPesq) and the protocol number for this approval was 442.
Statistical analysis
The Kappa test with a 95% confidence interval was used to evaluate the agreement between the two analyses of each evaluator and between the two evaluators when evaluating the description of the ALL abnormalities.
The chi-squared test, Fisher’s exact test and Student’s t test were used to evaluate the association between ALL injuries and other injuries found in the evaluated cases of acute ACL injury, the association between ALL injuries and the affected patient’s gender and age and the association between ALL injuries and the degree of anterolateral rotational instability. The association between complete and partial ACL tears and ALL abnormalities was also evaluated. For all variables, results with a p value of <0.05 were considered statistically significant.
Estimating the analysis of association frequencies, having as a parameter of refusal of the null Hypothesis the increase of the ALL injury frequency in the presence of associated lesions, we estimated a total sample size of at least 152 individuals would be necessary for this study. The present sample calculation has parameters Risk α ≤ 5% for Type I Error and Risk β ≤ 20% for Type II Error.
Results
A total of 252 patients with acute ACL injuries were initially included in the study. Of these 252 patients, 24 presented exclusion criteria, leaving 228 for the final evaluation (Fig. 1). The mean age of the patients was 34.1 ± 2.5 years; 165 were male and 63 female.
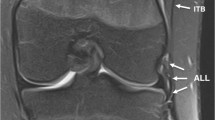
After evaluating the MRI exams, it was not possible to characterise the ALL adequately in 61 patients (26.7%). Among the remaining 167 patients, 101 ALL were normal (Fig. 2) and 66 (39.5%) had abnormalities according to the established criteria, divided into 30 (45.4%) cases of proximal injuries, 30 (45.4%) cases of distal injuries and 6 (9.1%) cases of concomitant anomalies in the proximal and distal portion of the ALL. Only four (6.1%) cases of ALL injury had distal avulsion (Segond fracture) (Fig. 3). Injuries to the other evaluated structures are described in Table 2.
Sagittal T2 FS-weighted MRI image (a) showing complete rupture of the anterior cruciate ligament (white arrow), with discontinuity and diffuse oedema, and Coronal T2 FS-weighted images showing injury of the medial collateral ligament (arrowheads) (b) and a normal anterolateral ligament (arrowheads) (c)
Sagittal T2 FS-weighted MRI image showing a complete rupture of the proximal ACL (white arrow) (a) and Coronal T2 FS- (b) and COR DP-weighted (c) MRI images showing a bone avulsion from the external margin of the lateral tibial plateau (Segond fracture) (arrow) and the anterolateral ligament attached to it (arrowheads). The same patient antero-posterior knee radiograph shows the bone fragment from the external margin of the lateral tibial plateau (d)
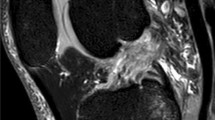
ALL injuries were associated with injuries to the LCL (p = 0.004), popliteus tendon (p = 0.005), MCL (p = 0.011) (Fig. 4), anterolateral capsule (p = 0.000034) and ITB, with an increased correlation with the degree of the ITB abnormality (no injury < low-grade injury < high-grade injury) (p = 0.000021). No cases of complete ITB injury were observed (Figs. 5, 6) (Table 3). There was also an increased correlation with bone contusions in the tibial plateau and femoral condyle related to ALL injury (without injury <, femoral condyle only <, tibial plateau only < both) (p = 0.008) (Fig. 7). There was no correlation between ALL injuries and injuries to the medial meniscus (p = n.s.), lateral meniscus (p = n.s.) or PCL (p = n.s.). Injury to the ALL was not associated with gender (p = n.s.), but was associated with patient age, with older patients having a greater tendency to present with ALL injury associated with ACL injury (p = 0.038). Partial ACL injuries were not associated with ALL injury, but complete injuries were associated (p = 0.023).
Sagittal T2 FS-weighted MRI image showing a complete rupture of the ACL (white arrow) (a). Coronal T2 FS-weighted MRI image showing a complete rupture of the anterolateral ligament (arrowheads) (b), mild strain of the lateral collateral ligament (arrow) (c) and rupture of the medial collateral ligament (arrows) (d)
Sagittal T2 FS-weighted MRI images showing discontinuity and diffuse oedema of the proximal ACL (white arrow), suggesting a complete rupture (a) and bone marrow oedema (*) representing contusions in the lateral femoral condyle and lateral tibial plateau (b). Coronal T2 FS-weighted MRI images showing complete rupture of the proximal ACL (arrow) and injury of the medial collateral ligament (arrowheads) (c) and rupture of the anterolateral ligament (arrow) (d)
The interobserver correlation according to the kappa test was 0.724. The intraobserver correlations were 0.819 and 0.855 for the two evaluators. Both results were considered satisfactory.
The medical records of 68 patients with a described ALL injury on MRI were available for evaluation. Among these patients, 34 presented a grade 1 pivot, 24 a grade 2 pivot and 10 a grade 3 pivot. ALL abnormalities were present in 3 (8.8%) patients with grade 1 pivot, 12 (50%) patients with grade 2 pivot and 8 (80%) patients with grade 3 pivot. A correlation between high-grade pivot shift and an ALL MRI abnormality was found (p = 0.000018).
Discussion
The main findings of this study were the approximately 40% prevalence of associated ALL injuries in acute ACL injury cases, the association of these injuries with the LCL, MCL, popliteus tendon, anterolateral capsule and ITB injuries and the lack of association with meniscal injuries, including those of the lateral meniscus, which has a solid connection with the ALL at its periphery [33]. In addition, there was no association between ALL injuries and partial ACL injuries, that is, where some of the ACL bands remain intact [34], and the association with complete injuries may suggest that the ALL is only injured in traumas of greater magnitude or that its integrity is a protective factor against complete ACL injuries.
Unlike the normal appearance of the ALL on MRI, few studies have investigated the association of ALL injury in cases of ACL injury, and the results have been controversial [18–21]. Claes et al. [18] found ALL abnormalities in almost 80% of cases, whereas in other studies, this figure did not exceed 50% [20, 21]. This discrepancy probably occurred because Claes et al. [18] did not distinguish among acute, subacute and chronic ACL injuries. The inclusion of all ACL injuries together may have increased the percentage of ALL abnormalities, if we consider that the lateral structures have an increased function in the absence of the ACL and the ALL MRI signal could be altered in these patients due to this overload [9, 35]. No study focused on the potential healing of the ALL, but the scar tissue of a healed ligament would not present a totally normal MRI sign. The eventual healing potential of this structure could also cause a false-positive evaluation of this structure in a chronic ACL lesion scenario. In our study, which only included cases of acute injury, we found similar results to those of Helito et al. [20] and Van Dyck et al. [21], so we believe that the percentage of associated abnormalities should be approximately 40–50%.
Focusing on others anterolateral structures, in a study evaluating abnormalities of the anterolateral capsule in acute ACL injuries, Musahl et al. [36] found changes in 51% of the patients, a higher percentage than we found in this study for this structure (29.9%). Those authors did not focus specifically on the ALL evaluation. Mansour et al. [32] evaluated the ITB abnormalities in acute knee trauma and found this structure was the most injured one, even though most of the lesions were considered to be minor sprain, probably without clinical significance. They also found an association with ACL injury. These authors did not focus on the ALL as well. Terry et al. [37] also found the ITB was frequently injured in association with an ACL injury. Some authors postulated that the capsulous-osseus layer of the ITB described by Terry et al. [37] and the ALL are generally the same structure dissected in different ways [38]. As we found association between ALL, anterolateral capsule and ITB injures in this study, it is probably true that they work in a synergistic way to provide anterolateral knee stability. Biomechanical studies are still controversial to show what is the most important structure to resist against anterolateral forces [39, 40]. Even with this high number of detected lesions, evaluations of residual pivot shift after ACL reconstruction using different techniques show that a large proportion of these ALL and anterolateral structures injuries might heal without affecting knee stability [8, 11, 41–44].
Regarding the location of ALL injuries, most studies found injuries in the distal portion of the ALL, but a minority of these injuries were Segond fractures [18, 20, 21]. We believe that the location of the abnormality is secondary, may be associated with the trauma mechanism and likely has no influence on the sufficiency of this structure. A study of unconventional trauma mechanisms evaluating knee lateral complex injuries found only proximal ALL injuries, concomitant to injuries in the LCL origin [45].
In relation to associated injuries that could help identify the ALL in cases of diagnostic doubt regarding ALL injury due to non-visualisation or lack of experience on the part of the orthopaedic surgeon or radiologist in the evaluation of this structure, we found an association with peripheral ligament injuries, anterolateral structures and bone contusions, but we did not find any association with meniscal injuries. Van Dyck et al. [21] conducted a similar study, but with a smaller number of patients, and found an association between ALL injuries with LCL and lateral meniscus injuries and bone contusions. Those authors also found a trend toward association with MCL injuries, which was confirmed in this study. In addition to confirming the association with peripheral injuries, we also found an association with popliteus tendon abnormalities, which were not evaluated by Van Dyck et al. [21]. Regarding the bone contusions typical of ACL injury, we found a growing association between this finding and ALL injury ; only 5.9% of patients with ALL injuries showed no bone injuries, and 46.5% had bone contusions on both the femur and tibia, denoting greater ACL injury trauma energy (Table 4). Song et al. [46] also found an association between bone contusion and ALL injury in patients with acute ACL injuries.
On the other hand, no association between ALL abnormalities and meniscal injuries was found. Because of the close proximity of the ALL to the lateral meniscus, some anatomical studies have suggested that there might be an association between injuries to these structures [1–3, 33]. The only two studies that have attempted to demonstrate this association present conflicting results. Van Dyck et al. [21] found an association between these injuries but Helito et al. [20] did not. While one study only used MRI [20], the other also used arthroscopy and identified some lateral meniscal injuries that were not initially observed on the MRI [21]. However, a minority of these injuries that had not been identified initially had ALL abnormalities. Given the statistical value found for this association in this study, we do not believe that the identification of some occasional MRI false negatives on arthroscopy would significantly alter the values found. The non-association with lateral meniscus injuries may suggest that when there is damage to the ALL, this structure does not subject the lateral meniscus to excessive traction, possibly avoiding its injury. More clinical and biomechanical studies should be conducted to confirm this hypothesis.
According to the associated injury findings, it is possible to infer that ALL injuries occur in association with acute ACL injuries in cases of higher energy injury. The non-association between ALL injuries and partial ACL injuries reinforces this hypothesis. The hypothesis that can be inferred from this finding in relation to partial injuries is that the ALL is only damaged when the ACL is completely torn, which subjects the knee to greater rotational forces, or that its integrity has a protective factor for ACL injury and that the ACL is only fully damaged if its secondary restrictors are affected. Engebretsen et al. [7] found that lateral tenodesis reduces stress on a reconstructed ACL graft by 43%. The integrity of the native anterolateral structures could also act to reduce stress on the ACL.
Segond fractures were found only in a minority of ALL injuries. The four cases found in this study correspond to only 6.1% of the evaluated ALL injuries and only 2.6% of all 228 ACL injury cases initially evaluated. Van Dyck et al. [21] found a considerable number, 17%, of these injuries in their sample; however, Sonnery-Cottet et al. [11] found only 1.1% in a sample of 92 cases, and Flores et al. found only 1.25% in a large sample [47]. A similar study found only 3 Segond fractures among 101 cases studied [13]. We therefore do not believe it is possible to only consider the Segond fracture as an abnormality of the anterolateral knee complex. In a study of patients undergoing exploratory surgery of the lateral compartment after acute ACL injury, Ferretti et al. [48] found this type of injury in 10% of cases, whereas another 80% of patients had other anterolateral abnormalities. Previous studies have proposed the term “Segond-like” to characterise anterolateral injuries where there is no clear Segond fracture involved [20]. Despite some controversy over which is the main anatomical structure responsible for this fracture, recent studies have found a correlation with the ALL, although there is not yet a defined consensus in this regard [23, 25, 28, 49, 50]. In biomechanical studies seeking to evaluate the strength and resistance of the ALL, Kennedy et al. [5] and Helito et al. [51] were able to reproduce Segond fracture cases, and Kennedy et al. found these fractures to be a major mechanism in ALL failure. The findings of these studies corroborate the hypothesis that ALL is the structure responsible for Segond fractures.
The limitations of this study include the absence of a specific protocol for ALL evaluation on MRI. Although some studies have suggested that the use of proton density sequences and the visualisation of lower lateral genicular vessels [13] could assist in visualisation, evaluations to date have been based on the radiologist’s and orthopaedist’s experience and made empirically. This limitation is a constant limitation in all studies evaluating the ALL with MRI [1, 12–15, 18, 21, 24, 36, 45, 50, 52]. Another limitation was the non-use of arthroscopic or open surgery to confirm the MRI findings, what might have cause some false-positive and false-negative numbers, specially the correlation of associated meniscal injuries, which could have affected some of the numbers of injuries found, although MRI is very accurate when identifying these injuries [53–55]. It is also known that the detected MRI injuries not always correspond to a clinical instability and some normal structures in MRI can be insufficient to provide knee stability. We can also cite that the correlation between these injuries and physical examination for anterolateral instability was not provided for all patients and the degree of instability found was only reported on the medical records, although previous studies have correlated lateral insufficiency with increased instability on the pivot shift test [9, 10, 30, 40, 56]. The use of 1.5 T instead of 3.0 T for all patients can also be considered a limitation. The use of 3.0 T only could lead to a different result, although Helito et al. [20] did not find any difference in the capability to visualise the ALL with 1.5 and 3.0 T in their study.
The most important clinical relevance of this study is the characterisation of knee sentinel lesions that will make surgeons aware of a possible ALL lesion in MRI, even if it is not completely clear in imaging evaluation, especially if a high degree of anterolateral instability is present on physical examination.
Conclusion
ALL injuries are present in approximately 40% of ACL injuries, and a minority of these are Segond fractures. These injuries are associated with peripheral ligament injuries, anterolateral structures lesions and bone contusions, but there is no association with meniscal injuries. Surgeons must be aware of these associations to consider an ALL lesion even if it is not completely clear in imaging evaluation, especially if a high degree of anterolateral instability is present on physical examination.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ALL:
-
Anterolateral ligament
- MCL:
-
Medial collateral ligament
- LCL:
-
Lateral collateral ligament
- PCL:
-
Posterior cruciate ligament
- PT:
-
Popliteus tendo
- MRI:
-
Magnetic resonance imaging
- ITB:
-
Iliotibial band
References
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A (2015) A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc 23:3186–3195
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328
Helito CP, Demange MK, Bonadio MB, Tirico LE, Gobbi RG, Pecora JR, Camanho GL (2013) Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med 1:2325967113513546
Helito CP, Torres JA, Bonadio MB, Aragao JA, de Oliveira LN, Natalino RJ, Pecora JR, Camanho GL, Demange MK (2016) Anterolateral ligament of the fetal knee: an anatomic and histological study. Am J Sports Med. doi:10.1177/0363546516664888
Kennedy MI, Claes S, Fuso FA, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43:1606–1615
Vincent JP, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20:147–152
Engebretsen L, Lew WD, Lewis JL, Hunter RE (1990) The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med 18:169–176
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520
Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ, D’Arrigo C (2012) Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc 20:870–877
Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ, Goldsmith MT, LaPrade RF (2016) An in vitro robotic assessment of the anterolateral ligament, part 1: secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. Am J Sports Med 44:585–592
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med 43:1598–1605
Helito CP, Demange MK, Helito PV, Costa HP, Bonadio MB, Pecora JR, Rodrigues MB, Camanho GL (2015) Evaluation of the anterolateral ligament of the knee by means of magnetic resonance examination. Rev Bras Ortop 50:214–219
Helito CP, Helito PV, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL, Demange MK (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skelet Radiol 43:1421–1427
Kosy JD, Mandalia VI, Anaspure R (2015) Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skelet Radiol 44:1647–1653
Macchi V, Porzionato A, Morra A, Stecco C, Tortorella C, Menegolo M, Grignon B, De Caro R (2015) The anterolateral ligament of the knee: a radiologic and histotopographic study. Surg Radiol Anat 38:341–348
Porrino J Jr, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS (2015) The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. AJR Am J Roentgenol 204:367–373
Helito CP, Helito PV, Bonadio MB, Pecora JR, Bordalo-Rodrigues M, Camanho GL, Demange MK (2015) Correlation of magnetic resonance imaging with knee anterolateral ligament anatomy: a cadaveric study. Orthop J Sports Med 3:2325967115621024
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80:45–49
Hartigan DE, Carroll KW, Kosarek FJ, Piasecki DP, Fleischli JF, D’Alessandro DF (2016) Visibility of anterolateral ligament tears in anterior cruciate ligament-deficient knees with standard 1.5-tesla magnetic resonance imaging. Arthroscopy 32:2061–2065
Helito CP, Helito PV, Costa HP, Demange MK, Bordalo-Rodrigues M (2016) Assessment of the anterolateral ligament of the knee by magnetic resonance imaging in acute injuries of the anterior cruciate ligament. Arthroscopy. doi:10.1016/j.arthro.2016.05.009
Van Dyck P, Clockaerts S, Vanhoenacker FM, Lambrecht V, Wouters K, De Smet E, Gielen JL, Parizel PM (2016) Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 26:3383–3391
Daggett M, Ockuly AC, Cullen M, Busch K, Lutz C, Imbert P, Sonnery-Cottet B (2015) Femoral origin of the anterolateral ligament: an anatomic analysis. Arthroscopy 32:835–841
Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J, Resnick D (2001) Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 219:381–386
Coquart B, Le Corroller T, Laurent PE, Ollivier M, Pradel V, Champsaur P, Guenoun D (2016) Anterolateral ligament of the knee: myth or reality? Surg Radiol Anat 38:955–962
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA (2014) The anterolateral ligament: anatomy, length changes and association with the Segond fracture. Bone Joint J 96-B:325–331
Helito CP, Amaral C, Nakamichi YC, Gobbi RG, Bonadio MB, Natalino RJM, Pecora JR, Cardoso TP, Camanho GL, Demange MK (2016) Why do authors differ with regard to the femoral and meniscal anatomical parameters of the knee anterolateral ligament?. Orthop J Sports Med 4:2325967116675604
Hughston JC, Andrews JR, Cross MJ, Moschi A (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 58:173–179
Irvine GB, Dias JJ, Finlay DB (1987) Segond fractures of the lateral tibial condyle: brief report. J Bone Joint Surg Br 69:613–614
Terry GC, Hughston JC, Norwood LA (1986) The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med 14:39–45
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. Am J Sports Med 44:362–369
Guenoun D, Le Corroller T, Amous Z, Pauly V, Sbihi A, Champsaur P (2012) The contribution of MRI to the diagnosis of traumatic tears of the anterior cruciate ligament. Diagn Interv Imaging 93:331–341.
Mansour R, Yoong P, McKean D, The JL (2014) The iliotibial band in acute knee trauma: patterns of injury on MR imaging. Skelet Radiol 43:1369–1375
Helito CP, Bonadio MB, Soares TQ, da Mota EARF, Natalino RJ, Pecora JR, Camanho GL, Demange MK (2016) The meniscal insertion of the knee anterolateral ligament. Surg Radiol Anat 38:223–228
Ferretti M, Levicoff EA, Macpherson TA, Moreland MS, Cohen M, Fu FH (2007) The fetal anterior cruciate ligament: an anatomic and histologic study. Arthroscopy 23:278–283
George MS, Dunn WR, Spindler KP (2006) Current concepts review: revision anterior cruciate ligament reconstruction. Am J Sports Med 34:2026–2037
Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, Lopomo N, Samuelsson K, Irrgang JJ (2016) The influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. doi:10.1177/0363546516659649
Terry GC, Norwood LA, Hughston JC, Caldwell KM (1993) How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med 21:55–60
Daggett M, Claes S, Helito CP, Imbert P, Monaco E, Lutz C, Sonnery-Cottet B (2016) The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee: letter to the editor. Am J Sports Med. doi:10.1177/0363546516638069
Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, Amis AA (2016) The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med 44(345):54
Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L, Imbert P (2016) The involvement of the anterolateral ligament in rotational control of the knee. Am J Sports Med 44:1209–1214
Dai C, Wang F, Wang X, Wang R, Wang S, Tang S (2016) Arthroscopic single-bundle anterior cruciate ligament reconstruction with six-strand hamstring tendon allograft versus bone-patellar tendon-bone allograft. Knee Surg Sports Traumatol Arthrosc 24:2915–2922
Karikis I, Ahlden M, Casut A, Sernert N, Kartus J (2016) Comparison of outcome after anatomic double-bundle and antero-medial portal non-anatomic single-bundle reconstruction in ACL-injured patients. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4132-z
Liu A, Sun M, Ma C, Chen Y, Xue X, Guo P, Shi Z, Yan S (2015) Clinical outcomes of transtibial versus anteromedial drilling techniques to prepare the femoral tunnel during anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3672-y
Vadala AP, Iorio R, De Carli A, Bonifazi A, Iorio C, Gatti A, Rossi C, Ferretti A (2013) An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop 37:187–192
Davis BA, Hiller LP, Imbesi SG, Chang EY (2015) Isolated lateral collateral ligament complex injury in rock climbing and Brazilian Jiu-jitsu. Skelet Radiol 44:1175–1179
Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H (2016) Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy. doi:10.1016/j.arthro.2016.03.015
Flores DV, Smitaman E, Huang BK, Resnick DL (2016) Segond fracture: an MR evaluation of 146 patients with emphasis on the avulsed bone fragment and what attaches to it. Skelet Radiol 45:1635–1647
Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A (2016) Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy. doi:10.1016/j.arthro.2016.05.010
Claes S, Luyckx T, Vereecke E, Bellemans J (2014) The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 30:1475–1482
De Maeseneer M, Boulet C, Willekens I, Lenchik L, De Mey J, Cattrysse E, Shahabpour M (2015) Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skelet Radiol 44:413–421
Helito CP, Bonadio MB, Rozas JS, Wey JM, Pereira CA, Cardoso TP, Pecora JR, Camanho GL, Demange MK (2016) Biomechanical study of strength and stiffness of the knee anterolateral ligament. BMC Musculoskelet Disord 17:193. doi:10.1186/s12891-016-1052-5
Taneja AK, Miranda FC, Braga CA, Gill CM, Hartmann LG, Santos DC, Rosemberg LA (2015) MRI features of the anterolateral ligament of the knee. Skeletal Radiol 44:403–410
Gupta MK, Rauniyar MK, Karn NK, Sah PL, Dhungel K, Ahmad K (2014) MRI evaluation of knee injury with arthroscopic correlation. J Nepal Health Res Counc 12:63–67
Phelan N, Rowland P, Galvin R, O’Byrne JM (2016) A systematic review and meta-analysis of the diagnostic accuracy of MRI for suspected ACL and meniscal tears of the knee. Knee Surg Sports Traumatol Arthrosc 24:1525–1539
Wong KP, Han AX, Wong JL, Lee DY (2016) Reliability of magnetic resonance imaging in evaluating meniscal and cartilage injuries in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-016-4211-1
Monaco E, Maestri B, Conteduca F, Mazza D, Iorio C, Ferretti A (2014) Extra-articular ACL reconstruction and pivot shift: in vivo dynamic evaluation with navigation. Am J Sports Med 42:1669–1674
Author contributions
CPH designed the study, analysed the data and wrote the manuscript. PVPH designed the study, analysed the data and wrote the manuscript. RVL analysed the data and wrote the manuscript. MKD supervised the study. MBR analysed the data and supervised the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest in relation to this study.
Funding
The study had no funding.
Ethical approval
The study was approved by the ethics committee of the institution (CEPesq) and the protocol number for this approval was 442.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Helito, C.P., Helito, P.V.P., Leão, R.V. et al. Anterolateral ligament abnormalities are associated with peripheral ligament and osseous injuries in acute ruptures of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 25, 1140–1148 (2017). https://doi.org/10.1007/s00167-017-4498-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4498-6