Abstract
Purpose
A ligament of the knee has recently drawn the attention: the rediscovered anterolateral ligament (ALL) of the knee. The tibial insertion of the ALL is torn off in the Segond fracture, pathognomonic of the anterior cruciate ligament tear. The ALL originates from the lateral femoral epicondyle and has fibers inserting on the lateral meniscus. It attaches distally to the tibial plateau, midway between the tip of the fibular head and Gerdy’s tubercle. The purpose of this study was to evaluate the visibility of the ALL using routine MRI (1.5T) protocol.
Materials and methods
In the first part of our study 10 cadaveric knee joints were examined using MR imaging to evaluate the visibility of the ALL. These cadaveric knees have been dissected to assess the presence of the ALL and to evaluate the accordance between MRI and anatomic dissection. In the second part of the study, 61 knee MRI of patients were examined to evaluate the visibility of the ALL using axial and coronal DP-FS weighted sequences.
Results
In all cadaveric knee MRI, the ALL was visualized (full visualization in 75 % and partial visualization in 25 % of the cases), with 100 % accordance between MRI and anatomic dissection. Two cadaveric knees where the ALL was not viewed were excluded of the radio-anatomic analysis. The ALL was visualized in 93.4 % (95 % CI = 84.1–98.2) of the knee MRI studies of the 61 patients included. The whole ligament was visualized in 82 % (95 % CI = 70–90.6) examinations and it was partially visualized in 11.5 % (95 % CI = 4.7–22.2).
Conclusion
Our results show that the ALL of the knee can be identified using routine 1.5T MR imaging, which suggest that better radiological description of this underestimated anatomical structure may be beneficial in the preoperative planning of ACL tears.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A ligament of the knee has recently drawn the attention: the rediscovered anterolateral ligament (ALL). It was originally described in 1879 when Dr Paul Segond demonstrated the existence of a pearly, resistant, fibrous band at the anterolateral aspect of the knee, whose tibial insertion is torn off in the Segond fracture [5, 7, 10, 23, 25, 31].
This resulted in a confusion in its name and anatomical description: anterior band of the lateral collateral ligament [15], lateral capsular ligament [14, 21] or anterior oblique band [1]. In recently published papers, all authors agree on the common name of the anterolateral ligament of the knee.
Recent cadaveric studies have defined anatomical characteristics of the ALL. This ligamentous structure connecting the femur to the tibia originates from the lateral femoral epicondyle, near the fibular collateral ligament (FCL). The ALL has an oblique trajectory, with fibers inserting on the lateral meniscus for most authors and a distal attachment to the lateral aspect of the lateral tibial condyle, midway between the tip of the fibular head and Gerdy’s tubercle [2, 6, 9, 30].
The Segond fracture (ALL distal avulsion) is related to a forced medial rotation trauma and is pathognomonic of the anterior cruciate ligament (ACL) tear [8, 10, 29, 31].
The ALL seems to be an anterolateral stabilizer of the knee [14, 22] injured in around 80 % of ACL ruptures for Claes et al. [4].
It has been suggested that anatomical reconstruction of ACL could result in improved results when combined with ALL reconstruction even if further studies are required to lead to improved clinical outcomes involving ACL reconstruction surgery [27].
Recently published studies have suggested that the ALL could be visible on ultrasound [3] and on magnetic resonance imaging (MRI) in variable proportions and especially on specific non-fat-saturated sequences [2, 4, 12, 20, 23, 28].
To the best of our knowledge, the ALL visibility with routine 1.5 T MRI sequences [T1-weighted, fat suppressed proton density (PD)-weighted] has not been studied to date. No radiological anatomical correlation with cadaveric dissection has been performed to date.
Purpose
The purpose of this study was to evaluate the visibility of the ALL using routine MRI protocol (sagittal T1-weighted, coronal and axial fat suppressed PD-weighted sequences).
Materials and methods
Anatomical study in cadavers
In accordance with our institution’s safety and ethical regulation, 10 cadaveric knee joints were examined using MR imaging (1.5T) to evaluate the visibility of the ALL.
The MR imaging protocol included coronal T1-weighted sequence and 2 mm thick reconstructions from a tridimensional SPAIR sequence.
The knees were then dissected by a team of two orthopedic surgeons (Anatomy laboratory, Faculty of Medicine of Timone, Marseille, France), blinded to MRI results, to assess the presence of the ALL of the knee and to characterize it.
Patient selection and exclusion criteria
In accordance with our institution’s safety and ethical regulation, all patients who underwent knee MRI scans between May and July 2014 were included. Institutional review board was not required for this retrospective study.
Exclusion criteria were suboptimal MRI examination (motion artifacts, incomplete protocol), a history of knee surgery and ACL tear.
For each patient, we collected the following information: age (years), gender (male, female) and indication to perform knee MRI.
MRI protocol
All MRI scans were performed on a 1.5T MR scanner (Philips® Achieva, Best Netherlands) using a dedicated knee coil (8-channel Sense knee array). A 15° knee flexion position was used.
The protocol included sagittal T1-weighted sequence (TR/TE: 500/18; number of excitations: 2; matrix: 512; thickness: 3.5 mm; field of view: 180 × 180 × 92 mm), axial fat suppressed PD-weighted sequence (2209/35; 3; 256; 3.5 mm; 112 × 84 × 160 mm), coronal fat suppressed PD-weighted sequence (1800/30; 3; 256; 3.5 mm; 77 × 143 × 180 mm) and tridimensional SPAIR (800/35; 3; 268; 1.24 mm; 160 × 160 × 99 mm) with 2 mm thick reconstruction (not used for ALL analysis).
Images analysis
Two radiologists (a staff radiologist with 10 years experience (reader 1) and a resident with 1 year of experience in musculoskeletal radiology (reader 2) reviewed MRI scans in consensus.
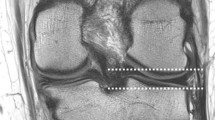
The ALL was assessed for its visibility (non-visualized, partially visualized or completely visualized). The ALL was considered as visible only if it was visible on two planes to overcome partial-volume effect or misinterpretation of structures (direct cross referencing technique).
The ALL was considered completely visible when all three portions of its length were seen, even if the insertion was not clearly individualized. If the ALL was seen on only one MRI sequence, it was not considered visible.
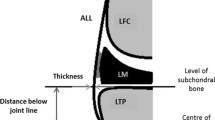
The ALL presents a proximal femoral portion, a middle meniscal portion next to the lateral meniscus with fibers inserting on it and a distal tibial portion inserting on the tibial plateau (Fig. 1).
Statistical analysis
The standard deviation of the average age and the measurement of 95 % confidence intervals for ALL visibility percentages were calculated using the binomial exact method.
Results
Population and MRI indications (Tables 1, 2)
Exclusion criteria were a history of ACL reconstruction, 23 because of a history of knee surgery (18 ACL plasty), 9 because of a ACL tear, 10 because of an incomplete protocol and 5 because of artefacted examination.
A total of 61 patients were included.
Patient age ranged from 15 to 83 years with a mean age of 48 years (standard deviation 19 years). The MRI examinations concerned right knees in 60 % and left knees in 40 %. MRI indications were knee pain (67 %), recent trauma (11 %) and other (21 %).
ALL analysis on cadaveric knees
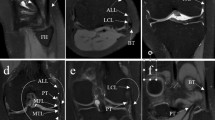
Coronal T1-weighted, coronal and axial SPAIR sequences were used in combination to identify the ALL of the knee (direct cross-referencing of images).
Two orthopedic surgeons performed independently the anatomical dissection. The ALL was identified in 80 % of the knee joints (8/10). Two knee joints where the ALL was not viewed were excluded of the radio-anatomic analysis. Knee MRI were performed and analyzed before anatomic dissection (Fig. 1). In all 8 cases, the ALL was visualized (full visualization in 75 % and partial visualization in 25 % of the cases), with 100 % accordance between MRI and anatomic dissection (Table 3).
ALL analysis on patient knees MRI
Axial and coronal fat suppressed PD-weighted sequences were used in combination to identify the ALL of the knee (direct cross-referencing of images) (Figs. 2, 3). The ALL was visualized in 93.4 % (95 % CI = 84.1–98.2) of the knee MRI studies. The whole ligament was visualized in 82 % (95 % CI = 70–90.6) examinations and it was partially visualized in 11.5 % (95 % CI = 4.7–22.2). Only 8 % (CI 95 % = 1.8–15.9) of MR examinations did not demonstrate the ALL (Table 4).
ALL was identified as a thin hypointense band originating from the lateral femoral epicondyle and with a distal insertion on the lateral tibial plateau between the Gerdy’s tubercle and the fibular head (Figs. 1, 4). Its origin was anterior or anterior-distal to the femoral origin of FCL and not always clearly distinguishable from it. The connecting fibers with the lateral meniscus were often well visible. Its distal fibers were close to the posterior fibers of the iliotibial band (ITB). No connecting fibers with popliteal tendon (PT) were observed.
Discussion
The ALL was identified in all cadaveric studies as a distinct ligamentous structure at the anterolateral aspect of the knee, which was clearly distinct from ITB and FCL. Moreover, recent cadaveric studies precisely describe the anatomical structure of the ALL of the knee. Nevertheless some slight discrepancies remain between these studies.
The ALL is described as extra-capsular for some authors [6, 9] whereas it appears as a capsular thickening for others [2, 17, 30]. The origin of the ALL is situated at the prominence of the lateral femoral epicondyle. For some authors connecting fibers are observed between ALL and the joint capsule [9], the FCL [2, 6], and the PT [30]. According to Claes et al. and Vincent et al., the origin of the ALL is anterior to the femoral origin of the FCL [6, 30] whereas it is posterior according to Dodds et al. [9] and posterior-proximal according to Kennedy et al. [17]. According to Scott Caterine et al. the femoral origin of the ALL is somewhat variable in position, inserting either anterior-distal (60 %) or posterior-proximal (40 %) to the femoral origin of the FCL [2]. Given the fact that the femoral origins of ALL and FCL are so closely associated, Claes et al. propose to envelop both structures in the term “lateral collateral complex” [6]: the ALL can be regarded as the lateral counterpart of the deep tibial collateral ligament [18]. According to Vincent et al. the origin of the ALL is just anterior to the popliteus tendon insertion in 90 % of cases [30] whereas it is posterior-proximal for Claes et al. [6]. The ALL has connecting fibers with the periphery of the middle third of the lateral meniscus which is divided into meniscofemoral and meniscotibial portions of the ALL [2, 6, 9, 30]. The lateral inferior geniculate artery and vein is situated in between the lateral meniscal rim and the ALL at the level of the joint line [6]. All authors agree that the distal insertion of the ALL is at the anterolateral side of the proximal tibia in the middle of the line connecting Gerdy’s tubercle and the tip of the fibular head. Flexion of knee to 90° and internal rotation result in tightening of the structure [30].
Cadaveric studies identified the ALL in above 80 % of the examined knees with most studies indicating incidences closer to 100 % [2, 5, 6, 9, 11, 24, 30].
One case report describes the identification of the ALL by ultrasound examination with the knee in 90° flexion and slight internal rotation [3].
Radiographic landmarks of the ALL origin and insertion have been described in order to facilitate the anatomical placement of tunnels during reconstruction of this ligament, even though the authors agree that indications for such a procedure have not been defined yet [24].
Using MRI, the ALL was identified in 100 % of the examined knees in most studies [4, 23] with no further information about partial or total visualization. Helito et al. visualized at least one of the three portions of the ALL in 97.8 % of examined knees [12] while Taneja et al. visualized it in 51 % [28]. All these results were obtained with specific sequences (T2 without FS, PD without FS, three-dimensional T1), which are not performed for routine MRI in the context of traumatic knee evaluation. We know that the ALL is surrounded by adipose tissue and therefore easier to visualize on non-fat-suppressed sequences. Porrino et al. have studied the ALL with routine sequences (coronal PD SPAIR and axial T2-weighted SPAIR) on 3T-MRI with a total visualization of the ALL in 100 % of the cases while stating that the ALL is inseparable from the adjacent FCL at their femoral attachment site and that the distal insertion is inseparable anteriorly from the posterior fibers of the ITT [23]. More recently Macchi et al. have studied the ALL of 47 patients with T1- and T2-weighted sequences on 1.5 T-MRI and visualized it in 93 % and note that ALL was more difficult to recognize in young patients [20].
In our study, we were able to visualize the ALL in 93.4 % of the knees with a routine protocol (axial and coronal fat suppressed PD-weighted sequences) and a stringent criterion of visibility in both axial and coronal planes to confirm its visualization. The whole ligament was visualized in 82 % of the case. The ALL was identified with MRI as a thin hypointense band originating from the lateral femoral epicondyle and with a distal insertion on the lateral tibial plateau between the Gerdy’s tubercle and the fibula’s head. Its femoral origin was rarely clearly distinguishable from the insertion of the FCL. In addition, at the tibial distal insertion, there was not always reliable plane between the ALL and the posterior fibers of the ITT. These results are also consistent with other MRI studies and the differences with results of gross anatomical dissections are easily explained by the limitation of spatial resolution of MRI.
The clinical implications of confirming the visibility of ALL on MRI with routine protocol are as follows:
First we know now that ALL distal avulsion is pathognomonic of the ACL tear [8, 10, 29, 31]: visualization on an ALL avulsion in case of uncertain ACL rupture would allow to claim the rupture.
Then, Claes et al. demonstrated a high prevalence (79 %) of ALL abnormalities on the MRI of ACL-injured knees [4].
The ALL is for some authors an important lateral knee stabilizer, controlling internal tibial rotation and preventing tibial translation [14, 16, 22], especially at high angles of flexion [22].
The ALL is not repaired in usual ACL reconstruction and its rupture is probably responsible for some chronic anterolateral instability after isolated intra-articular reconstruction of the ACL in patients without any predisposing factors (improper tunnel positioning or problems with rehabilitation). The role of extra-articular lateral reconstruction/tenodesis combined with ACL reconstruction improving postoperative knee stability has been discussed but recent studies [19, 32] and a meta-analysis [13] showed a variable (marginally to statistically significant) reduction in pivot shift in favor of the combined procedure. Sonnery-Cottet et al. describe a safe and reproducible arthroscopic technique to allow identification and examination of the ALL [26] and demonstrate that a combined ACL and ALL reconstruction can be an effective procedure without specific complications [27].
Our results show that the ALL of the knee can be identified using routine 1.5 T MR imaging, which suggest that better radiological description of this underestimated anatomical structure may be beneficial in the preoperative planning of ACL tears.
References
Campos JC, Chung CB, Lektrakul N, Pedowitz R, Trudell D, Yu J, Resnick D (2001) Pathogenesis of the Segond fracture: anatomic and MR imaging evidence of an iliotibial tract or anterior oblique band avulsion. Radiology 219:381–386. doi:10.1148/radiology.219.2.r01ma23381
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A (2014) A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3117-z
Cianca J, John J, Pandit S, Chiou-Tan FY (2014) Musculoskeletal ultrasound imaging of the recently described anterolateral ligament of the knee. Am J Phys Med Rehabil 93:186. doi:10.1097/PHM.0000000000000070
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80:45–49
Claes S, Luyckx T, Vereecke E, Bellemans J (2014) The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 30:1475–1482. doi:10.1016/j.arthro.2014.05.039
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328. doi:10.1111/joa.12087
Delzell PB, Schils JP, Recht MP (1996) Subtle fractures about the knee: innocuous-appearing yet indicative of significant internal derangement. AJR Am J Roentgenol 167:699–703. doi:10.2214/ajr.167.3.8751684
Dietz GW, Wilcox DM, Montgomery JB (1986) Segond tibial condyle fracture: lateral capsular ligament avulsion. Radiology 159:467–469. doi:10.1148/radiology.159.2.3961179
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA (2014) The anterolateral ligament Anatomy, length changes and association with the Segond fracture. Bone Joint J 96:325–331
Goldman AB, Pavlov H, Rubenstein D (1988) The Segond fracture of the proximal tibia: a small avulsion that reflects major ligamentous damage. AJR Am J Roentgenol 151:1163–1167. doi:10.2214/ajr.151.6.1163
Helito CP, Demange MK, Bonadio MB, Tírico LEP, Gobbi RG, Pécora JR, Camanho GL (2013) Anatomy and histology of the knee anterolateral ligament. Orthop J Sports Med 1:2325967113513546. doi:10.1177/2325967113513546
Helito CP, Helito PVP, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL, Demange MK (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol 43:1421–1427. doi:10.1007/s00256-014-1966-7
Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy. doi: 10.1016/j.arthro.2015.04.089
Hughston JC, Andrews JR, Cross MJ, Moschi A (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. J Bone Joint Surg Am 58:173–179
Irvine GB, Dias JJ, Finlay DB (1987) Segond fractures of the lateral tibial condyle: brief report. J Bone Joint Surg Br 69:613–614
James EW, LaPrade CM, LaPrade RF (2015) Anatomy and biomechanics of the lateral side of the knee and surgical implications. Sports Med Arthrosc Rev 23:2–9. doi:10.1097/JSA.0000000000000040
Kennedy MI, Claes S, Fuso FAF, Williams BT, Goldsmith MT, Turnbull TL, Wijdicks CA, LaPrade RF (2015) The anterolateral ligament: an anatomic, radiographic, and biomechanical analysis. Am J Sports Med 43:1606–1615. doi:10.1177/0363546515578253
LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L (2007) The anatomy of the medial part of the knee. J Bone Joint Surg Am 89:2000–2010. doi:10.2106/JBJS.F.01176
Lerat JL, Chotel F, Besse JL, Moyen B, Binet G, Craviari T, Brunet-Guedj E, Adeleine P, Nemoz JC (1998) The results after 10–16 years of the treatment of chronic anterior laxity of the knee using reconstruction of the anterior cruciate ligament with a patellar tendon graft combined with an external extra-articular reconstruction. Rev Chir Orthop Reparatrice Appar Mot 84:712–727
Macchi V, Porzionato A, Morra A, Stecco C, Tortorella C, Menegolo M, Grignon B, De Caro R (2015) The anterolateral ligament of the knee: a radiologic and histotopographic study. Surg Radiol Anat. doi:10.1007/s00276-015-1566-9
Moorman CT, LaPrade RF (2005) Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg 18:137–145
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43:669–674. doi:10.1177/0363546514562751
Porrino J, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS (2015) The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. AJR Am J Roentgenol 204:367–373. doi:10.2214/AJR.14.12693
Rezansoff AJ, Caterine S, Spencer L, Tran MN, Litchfield RB, Getgood AM (2014) Radiographic landmarks for surgical reconstruction of the anterolateral ligament of the knee. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-014-3126-y
Segond P (1879) Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse Progrès médical, 1–85
Sonnery-Cottet B, Archbold P, Rezende FC, Neto AM, Fayard J-M, Thaunat M (2014) Arthroscopic identification of the anterolateral ligament of the knee. Arthrosc Tech 3:e389–e392. doi:10.1016/j.eats.2014.02.009
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S (2015) Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. doi:10.1177/0363546515571571
Taneja AK, Miranda FC, Braga CAP, Gill CM, Hartmann LGC, Santos DCB, Rosemberg LA (2014) MRI features of the anterolateral ligament of the knee. Skeletal Radiol. doi:10.1007/s00256-014-2052-x
Terry GC, Norwood LA, Hughston JC, Caldwell KM (1993) How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med 21:55–60
Vincent J-P, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F, Al-Saati MF, Lustig S, Demey G, Servien E, Neyret P (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20:147–152. doi:10.1007/s00167-011-1580-3
Woods GW, Stanley RF, Tullos HS (1979) Lateral capsular sign: x-ray clue to a significant knee instability. Am J Sports Med 7:27–33
Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP (2006) Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc 14:1060–1069. doi:10.1007/s00167-006-0130-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Coquart, B., Le Corroller, T., Laurent, P.E. et al. Anterolateral ligament of the knee: myth or reality?. Surg Radiol Anat 38, 955–962 (2016). https://doi.org/10.1007/s00276-016-1657-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-016-1657-2