Abstract
Purpose
To evaluate changes in midflexion rotational laxity before and after posterior-stabilized (PS)-total knee arthroplasty (TKA).
Methods
Twenty-nine knees that underwent PS-TKA were evaluated. Manual mild passive rotational stress was applied to the knees, and the internal–external rotational angle was measured automatically by a navigation system at 30°, 45°, 60°, and 90° of knee flexion.
Results
The post-operative internal rotational laxity was statistically significantly increased compared to the preoperative level at 30°, 45°, 60°, and 90° of flexion. The post-operative external rotational laxity was statistically significantly decreased compared to the preoperative level at 45° and 60° of flexion. The post-operative internal–external rotational laxity was statistically significantly increased compared to the preoperative level only at 30° of flexion. The preoperative and post-operative rotational laxity showed a significant correlation at 30°, 45°, 60°, and 90° of flexion.
Conclusion
Internal–external rotational laxity increases at the initial flexion range due to resection of both the anterior or posterior cruciate ligaments and retention of the collateral ligaments in PS-TKA. Preoperative and post-operative rotational laxity indicated a significant correlation at the midflexion range. This study showed that a large preoperative rotational laxity increased the risk of a large post-operative laxity, especially at the initial flexion range in PS-TKA.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Accurate alignment and proper soft tissue balance are crucial for a successful clinical outcome after total knee arthroplasty (TKA) [13, 14]. Appropriate soft tissue balance is largely dependent on the surgeon’s intuitive judgment during surgery, and joint instability is recognized as one of the major causes for early TKA failure [9, 25]. Inappropriate soft tissue balance causes overload on the weight-bearing surface and induces abrasive wear [6, 10]. In addition, activities of daily living often cause mechanical load to the knee joint in full extension and in midflexion. Midflexion stability is considered a key factor for improving the outcome of TKA.
Intraoperative laxity has been measured using various methods [7, 18–20, 23]. However, there is a paucity of research on how to best evaluate midflexion laxity intraoperatively. A navigation system has been developed to assist with precise bone cutting and accurate placement of prosthetic components. Navigation systems are also useful for monitoring joint positioning and kinematics intraoperatively [2, 4]. There are some reports on anterior–posterior, varus–valgus laxity, and gap balance; however, there are few reports on the rotational laxity at the midflexion range [3, 11, 21, 23, 27]. The cruciate ligaments are thought to serve as stabilizers of the knee during internal and external rotational stress [1, 15]. However, the influence of cruciate ligament resection due to TKA on post-operative laxity has not been fully investigated. It is hypothesized that post-operative midflexion rotational laxity is greater than preoperative laxity and that preoperative laxity impacts post-operative laxity throughout the range of motion (ROM) in posterior-stabilized (PS)-TKA. The purpose of the present study was to evaluate midflexion rotational laxity before and after PS-TKA using a navigation system.
Materials and methods
Twenty-nine patients underwent TKA with the PS prosthesis NexGen LPS-flex (Zimmer, Warsaw, IN, USA) using a navigation system (Precision Knee Navigation Software, version 4.0; Stryker, Kalamazoo, MI, USA). To fairly assess and minimize the influences of clinical variables, patients with a valgus deformity, preoperative severe flexion (<90°), and extension (>20°) restriction were excluded. The patient population comprised 16 women and 13 men with a mean age of 78 ± 5.0 years. The study population was normally distributed. The average hip-knee-ankle angle was 13.0° ± 5.6° in varus preoperatively.
The femoral rotational axis was defined by referring to the average rotational axis perpendicular to the Whiteside line and the transepicondylar axis. The tibial rotational axis was set parallel to the line connecting one-third of the tibial tubercle to the centre of the cut surface. The joint capsule was temporarily closed with four strands of suture after registration.
The investigator gently applied physiologically allowable maximal manual internal–external rotation stress to the knee without angular acceleration, and the mechanical femoral–tibial rotational angle was measured automatically by the navigation system at 30°, 45°, 60°, and 90° of knee flexion. These measurements were performed in the presence of osteophytes and soft tissues; thus, the anterior cruciate ligament was preserved.
Next, the distal femur was cut using the navigation-assisted measured resection technique. An incision was made into the proximal tibial by using a measured resection approach, and extramedullary alignment rods were placed. After removing the osteophytes, trial components were placed, and the knee was manually manoeuvred throughout ROM to assess the medial–lateral balance. When the soft tissue balance was inappropriate, the medial collateral ligament, posterior knee capsule, or other tissue was carefully released in an incremental manner for proper adjustment. After confirming that the TKA components and inserts were firmly placed in an appropriate position, the surgical incision was completely closed.
Then the same procedure as described for the pre-TKA measurements was repeated to measure and record the femoral–tibial rotational angles at 30°, 45°, 60°, and 90° by using the navigation system. The navigation system enabled us to assess the internal–external rotational angle independently of the knee flexion angle and varus–valgus angle (internal–external rotational laxity was expressed as the sum of the absolute internal and external stress angles. Positive values indicate internal orientation, and negative values indicate external orientation). The accuracy of the navigation system has been established at 0.5°.
The test–retest reliability of these internal–external rotational stress angle indicated that interclass and intraclass correlation coefficients (ICCs) were sufficiently high, with values >0.9 at 30°, 45°, 60°, and 90°, respectively.
This study was approved by the institutional review board of Ehime University (Identification Number: 1411020), and informed consent was obtained from all patients.
Statistical analysis
Non-parametric tests were used due to the small sample size, although an arithmetically sufficient normal distribution was found. Preoperative and post-operative TKA comparisons were performed by using the non-parametric Wilcoxon’s signed-rank test. Correlations were evaluated by using Spearman’s correlation coefficients. Analyses were performed with JMP, version 11.0 (SAS Institute, Tokyo, Japan). p < 0.05 was considered statistically significant. Statistical analyses for ICCs were performed by using IBM SPSS, version 23 (IBM, Corp., Armonk, NY, USA). An ICC >0.81 was judged as an almost perfect correlation. A sample size calculation was performed by using Power and Sample Size Calculations software, version 3.1.2 (Vanderbilt University, Nashville, TN, USA). After measuring rotational laxity in the first 10 patients, the mean and standard deviation of the preoperative and post-operative TKA data were calculated. To achieve a correlation of δ = 3, σ = 5 with 80 % power, and an α = 0.05, we determined that a minimum sample size of 24 patients would be required. To compensate for the small sample size, 29 patients were assessed.
Results
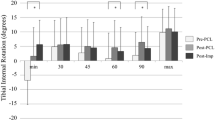
The average preoperative and post-operative values of internal rotational laxity were 8.9° ± 7.4°, 10.6° ± 7.2°, 11.6° ± 6.7°, and 14.1° ± 6.9° and 12.5° ± 7.8°, 13.3° ± 6.9°, 14.5° ± 6.8°, and 16.9° ± 7.3° at 30°, 45°, 60°, and 90° of flexion, respectively (Fig. 1). The post-operative internal rotational laxity values were significantly higher than the preoperative values at 30°, 45°, 60°, and 90° of flexion (p < 0.0001, <0.0001, 0.0002, and 0.004 at 30°, 45°, 60°, and 90° of flexion, respectively; Fig. 1).
Comparison of internal rotational laxity at 30°, 45°, 60°, and 90° of flexion angle between preoperative and post-operative total knee arthroplasty. For both charts: Y-axis label, joint laxity (°); X-axis label, knee flexion angle (°). Upper whiskers indicate the standard deviation. *p < 0.05, Wilcoxon’s signed-rank test
The average preoperative and post-operative values of external rotational laxity were −8.9° ± 7.1°, −11.2° ± 5.9°, −11.0° ± 6.1°, and −7.8° ± 5.4° and −9.0° ± 7.7°, −9.5° ± 7.7°, −8.8° ± 7.3°, and −6.6° ± 6.2° at 30°, 45°, 60°, and 90° of flexion, respectively (Fig. 2). The values of post-operative external rotational laxity were significantly lower than those at the preoperative level at 45° and 60° of flexion [p = not significant (n.s.), 0.048, 0.004, and n.s. at 30°, 45°, 60°, and 90° of flexion, respectively; Fig. 2].
Comparison of external rotational laxity at 30°, 45°, 60°, and 90° of flexion angle between preoperative and post-operative total knee arthroplasty. For both charts: Y-axis label, joint laxity (°); X-axis label, knee flexion angle (°). Upper whiskers indicate the standard deviation. *p < 0.05, Wilcoxon’s signed-rank test
As a result, the average values of preoperative and post-operative internal–external rotational laxity were 17.8° ± 4.8°, 21.8° ± 4.5°, 22.6° ± 4.9°, and 21.8° ± 4.8° and 21.5° ± 7.8°, 22.8° ± 7.0°, 23.3° ± 6.5°, and 23.4° ± 7.8° at 30°, 45°, 60°, and 90° of flexion, respectively (Fig. 3). The values of post-operative internal–external rotational laxity were significantly higher than those at the preoperative level at 30° of flexion (p = 0.002, n.s., n.s., and n.s. at 30°, 45°, 60°, and 90° of flexion, respectively; Fig. 3).
Comparison of internal–external rotational laxity at 30°, 45°, 60°, and 90° of flexion angle between preoperative and post-operative total knee arthroplasty. The internal–external rotational laxity is expressed as the sum of the maximum internal and maximum external rotational laxity angle measured under rotational stress. For both charts: Y-axis label, joint laxity (°); X-axis label, knee flexion angle (°). Upper whiskers indicate the standard deviation. *p < 0.05, Wilcoxon’s signed-rank test
The changing ratio of post-operative over preoperative rotational internal–external laxity was 1.24 ± 0.46 at 30° of flexion, whereas flexion angles of 45°, 60°, and 90° had changing ratio values of 1.07 ± 0.38, 1.05 ± 0.33, and 1.09 ± 0.36, respectively (Fig. 4). The changing ratio of internal–external rotational laxity at 30° was significantly different compared to that at 45°, 60°, and 90° of flexion (45°: p = 0.001, 60°: p = 0.004, 90°: p = 0.038; Fig. 4).
Comparison of the post-operative and preoperative changing rate of internal–external rotational laxity. Y-axis label, changing rate of laxity; X-axis label, knee flexion angle (°). Bars show the values dividing the mean post-operative rotational laxity values by the mean preoperative laxity values at 30°, 45°, 60°, and 90° of flexion angle. Upper whiskers indicate the standard deviation. *p < 0.05, Wilcoxon’s signed-rank test
Spearman’s single rank correlation coefficients of preoperative and post-operative rotational laxity were correlated at 30°, 45°, 60°, and 90° of flexion (ρ = 0.55, p = 0.002; ρ = 0.41, p = 0.026; ρ = 0.47, p = 0.01; and ρ = 0.6, p = 0.001 at 30°, 45°, 60°, and 90°, respectively; Table 1).
Discussion
The most important findings of the study were that post-operative rotational laxity at a flexion angle of 30° showed a statistically significant increase from the preoperative levels, whereas no remarkable change was shown at flexion angles of 45°, 60°, and 90°. Internal rotational laxity increased and external rotational laxity decreased post-operatively, resulting in no net change compared to the preoperative internal–external rotational laxity at 45°, 60°, and 90° of flexion. Zaffagnini et al. [29] showed that the implanted tibia was generally more internally rotated compared with the native tibia throughout the range of motion. They discussed this is probably because arthritic knees are often associated with some varus deformity which joint arthroplasty corrects, thereby altering the position of the tibia relative to the femur. Our results are in agreement with these findings.
It has been suggested that internal–external rotational laxity increases at flexion angles of 30° due to resection of both the anterior and posterior cruciate ligaments in PS-TKA. The cause of no further changes in internal–external rotational laxity seen at flexion angles of 45°, 60°, and 90° was likely due to the fact that all subjects had varus osteoarthritis and retained their medial collateral ligaments, which when accompanied by alignment correction, affected rotational laxity. It has been reported that collateral ligaments are elongated after TKA [24]. We reported greater varus–valgus laxity during midflexion, particularly at the initial flexion range, comparison with PS-TKA than with CR-TKA [11]. Minoda et al. [22] also reported that the centre size of the joint gap was loose especially at 30° of flexion. Many researchers have emphasized the importance of anatomically correct component alignment and joint stability for successful TKA surgery [8, 28]. There are relatively few methods for evaluating joint stability during TKA surgery, despite it being clinical significance. In most cases, the surgeon evaluates joint stability by performing a manual stress test intraoperatively, although such methods fall short of providing objective assessment measures. In addition, activities of daily living often cause mechanical load to the knee joint in full extension and in midflexion [16, 17]. However, midflexion rotational laxity is seldom evaluated in clinical practice.
The cruciate ligaments function as stabilizers against rotational torque [1, 15]. Regardless, few published studies have reported on intraoperative internal–external rotational laxity. Hunt et al. [12] reported no statistically significant difference in laxity between cruciate retaining (CR)-TKA and PS-TKA in a cadaver study. They also reported that internal–external rotational laxity decreased compared to its baseline levels [12]. Differences in our results from those of Hunt et al. [12] can be attributed to factors such as the implant design, soft tissue release, and implant installation angle. Moreover, osteoarthritic knees were evaluated in our study, whereas Hunt et al. [12] evaluated cadavers with near-normal knees, which potentially had a large effect on their results. The rotational tolerance due to the component design can be considered a factor that affects rotational laxity. One feature of the TKA design is its use of either a single radius in which rotation is centred on the sagittal plane, or a multi-radius in which the rotational centre is incrementally displaced. Hunt et al. [12] evaluation of single radius Triathlon knee arthroplasty also led to some results that differed with ours, because multi-radius LPS-flex knee arthroplasty was evaluated in our study. Stoddard et al. [26] hypothesized that displacement in the multi-radius model produces laxity, which leads to midflexion instability. Therefore, they studied midflexion instability with both models. However, this hypothesis was not supported, as they found no significant differences between the two models [26]. Nevertheless, stability improvement has been reported in midflexion laxity of cadavers in which a femoral component was fitted to match the continuous displacement of the rotational centre [5]. Although these were cadaveric studies, their results suggest that differences in midflexion laxity can be due to whether a CR or PS model is selected, the design of the components used, or tibial–femoral size matching; thus, these aspects are potential topics for further research.
Removing the anterior–posterior cruciate ligaments in PS-TKA would lead to greater rotational laxity throughout ROM. However, contrary to our expectations, changes in rotational laxity were only seen at the initial flexion range. In our study, post-operative rotational laxity increased at a flexion angle of 30°, preoperative and post-operative rotational laxity showed a significant correlation at 30° of flexion, which can potentially impact stability due to the effect of daily activities on component wear in PS-TKA. It is suggested by our results that some patients are unable to recover proper rotational stability at the initial flexion range despite the recovery of proper soft tissue balance in 0° of knee extension and 90° of knee flexion. Attention to rotational instability would be necessary when a large preoperative laxity exists at the initial flexion range in PS-TKA.
This study has some limitations. Surgery was performed by inflating the tourniquet and non-load-bearing conditions under general anaesthesia. Bone cutting was performed with the measured resection technique. The study had a small sample size, and only patients with varus-type arthritis were treated. Finally, the procedure involved manual passive stress by the operator. These limitations may restrict the generalization of our results; thus, further research is also necessary to determine the degree of rotational laxity adequate for TKA procedures. Future studies should examine the relationship between rotational laxity and the patient’s clinical course. The findings of this study may shed light on defining suitable laxity for TKA.
It is hypothesized that preoperative laxity impacts post-operative laxity. Using the same coordinate system preoperatively and post-operatively was essential for examining these hypotheses. The strengths of the current study were the use of a navigation system that enabled precise evaluation of rotational position throughout ROM, and using the same coordinate system preoperatively and post-operatively. Additionally, evaluating the preoperative data with the cruciate ligaments and meniscus preserved by using a strong suture at the capsule was clinically meaningful. This study showed that a large preoperative rotational laxity increased the risk of a large post-operative laxity, especially at the initial flexion range in PS-TKA. TKA requires exceedingly fine surgical adjustment of two counter opposed factors: stability and laxity.
Conclusion
Post-operative rotational laxity is greater than preoperative laxity at the initial flexion range in PS-TKA. Preoperative and post-operative rotational laxity indicated a significant correlation at the midflexion range.
References
Amis AA (2012) The functions of the fiber bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc 20:613–620
Bellemans J, D’Hooghe P, Vandenneucker H, Van Damme G, Victor J (2006) Soft tissue balance in total knee arthroplasty: does stress relaxation occur perioperatively? Clin Orthop Relat Res 452:49–52
Casino D, Zaffagnini S, Martelli S, Lopomo N, Bignozzi S, Iacono F, Russo A, Marcacci M (2009) Intraoperative evaluation of total knee arthroplasty: kinematic assessment with a navigation system. Knee Surg Sports Traumatol Arthrosc 17:369–373
Chauhan SK, Scott RG, Breidahl W, Beaver RJ (2004) Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br 86:372–377
Clary CW, Fitzpatrick CK, Maletsky LP, Rullkoetter PJ (2013) The influence of total knee arthroplasty geometry on mid-flexion stability: an experimental and finite element study. J Biomech 46:1351–1357
Collier JP, Mayor MB, Surprenant VA, Surprenant HP, Dauphinais LA, Jensen RE (1990) The biomechanical problems of polyethylene as a bearing surface. Clin Orthop Relat Res 261:107–113
Draganich LF, Pottenger LA (2000) The TRAC PS mobile-bearing prosthesis: design rationale and in vivo 3-dimensional laxity. J Arthroplasty 15:102–112
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24:39–43
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop Relat Res 392:315–318
Feng EL, Stulberg SD, Wixson RL (1994) Progressive subluxation and polyethylene wear in total knee arthroplastys with flat articular surfaces. Clin Orthop Relat Res 299:60–71
Hino K, Ishimaru M, Iseki Y, Watanabe S, Onishi Y, Miura H (2013) Mid-flexion laxity is greater after posterior-stabilised total knee arthroplasty than with cruciate-retaining procedures: a computer navigation study. Bone Joint J 95(B):493–497
Hunt NC, Ghosh KM, Blain AP, Rushton SP, Longstaff LM, Deehan DJ (2015) No statistically significant kinematic difference found between a cruciate-retaining and posterior-stabilised Triathlon knee arthroplasty: a laboratory study involving eight cadavers examining soft-tissue laxity. Bone Joint J 97(B):642–648
Insall J, Tria AJ, Scott WN (1979) The total condylar knee prosthesis: the first 5 years. Clin Orthop Relat Res 145:68–77
Insall JN, Binazzi R, Soudry M, Mestriner LA (1985) Total knee arthroplasty. Clin Orthop Relat Res 192:13–22
Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Aroen A, Engebretsen L, LaPrade RF (2013) Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med 41:2828–2838
Kettelkamp DB, Johnson RJ, Smidt GL, Chao EY, Walker M (1970) An electrogoniometric study of knee motion in normal gait. J Bone Joint Surg Am 52:775–790
Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–43
Louis S, Siebold R, Canty J, Bartlett RJ (2005) Assessment of posterior stability in total knee arthroplasty by stress radiographs: prospective comparison of two different types of mobile bearing implants. Knee Surg Sports Traumatol Arthrosc 13:476–482
Matsuda S, Miura H, Nagamine R, Urabe K, Matsunobu T, Iwamoto Y (1999) Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res 366:169–173
Matsumoto T, Kubo S, Muratsu H, Matsushita T, Ishida K, Kawakami Y, Oka S, Matsuzaki T, Kuroda Y, Nishida K, Akisue T, Kuroda R, Kurosaka M (2013) Different pattern in gap balancing between the cruciate-retaining and posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2338–2345
Matsuda Y, Ishii Y, Noguchi H, Ishii R (2005) Varus–valgus balance and range of movement after total knee arthroplasty. J Bone Joint Surg Br 87:804–808
Minoda Y, Nakagawa S, Sugama R, Ikawa T, Noguchi T, Hirakawa M, Nakamura H (2014) Intraoperative assessment of midflexion laxity in total knee prosthesis. Knee 21:810–814
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T, Tanaka K, Iwamoto Y (2003) Changes in anteroposterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Park KK, Hosseini A, Tsai TY, Kwon YM, Li G (2015) Elongation of the collateral ligaments after cruciate retaining total knee arthroplasty and the maximum flexion of the knee. J Biomech 48:418–424
Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM (2002) Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 404:7–13
Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. J Orthop Res 31:53–58
Van Damme G, Defoort K, Ducoulombier Y, Van Glabbeek F, Bellemans J, Victor J (2005) What should the surgeon aim for when performing computer-assisted total knee arthroplasty? J Bone Joint Surg Am 87(Suppl 2):52–58
Whiteside LA (2002) Soft tissue balancing: the knee. J Arthroplasty 17:23–27
Zaffagnini S, Bignozzi S, Saffarini M, Colle F, Sharma B, Kinov P, Marcacci M, Dejour D (2014) Comparison of stability and kinematics of the natural knee versus a PS TKA with a ‘third condyle’. Knee Surg Sports Traumatol Arthrosc 22:1778–1785
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hino, K., Kutsuna, T., Oonishi, Y. et al. Assessment of the midflexion rotational laxity in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25, 3495–3500 (2017). https://doi.org/10.1007/s00167-016-4175-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4175-1