Abstract
Purpose
There is an increased interest in treating arthritis of the medial and patellofemoral compartments without using a total knee arthroplasty. The purpose of this study was to measure kinematics in knees with a monoblock bicompartmental arthroplasty to see whether maintaining the cruciate ligaments and lateral compartment resulted in consistent kinematics more similar to healthy knees than those observed in replaced knees.
Methods
The kinematics of ten knees with monoblock bicompartmental arthroplasty were observed using fluoroscopy during three weight-bearing activities. Model-image registration techniques were used to quantify the three-dimensional motions of the knee joints.
Results
During kneeling, lunging, and stair-step activities, the medial condyle remained relatively close to the centre of the tibial plateau, while the lateral condyle typically moved posteriorly with flexion. Knees generally exhibited motion patterns consistent with retained cruciate ligament function, but individual patterns varied significantly.
Conclusions
Bicompartmental knee arthroplasty has the potential to retain more natural knee function. Improved tools for aligning the implants and increased implant sizing options may be required to achieve highly consistent results and realize the clinical benefit of a knee arthroplasty with intact cruciate ligaments.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is an increased interest in bone- and cruciate ligament-preserving treatments for knees with severe medial compartment and patellofemoral arthritis [3, 4, 19]. The challenge is to resurface these two compartments in a manner that works well with the intact lateral compartment and cruciate ligaments and that is simple, reproducible, and cost-effective to perform. In most cases, total knee arthroplasty (TKA) is used to treat bicompartmental knee osteoarthritis, with unicompartmental knee arthroplasty (UKA) reserved for knees with only a single arthritic compartment. It has been reported that UKA leads to faster recovery time, less bone loss, and better knee kinematics when compared with TKA, e.g. [23], making it attractive to extend this bone- and ligament-sparing approach to knees with bicompartmental disease.
Several approaches to bicompartmental knee arthroplasty (BKA) have been reported [10, 19, 20, 22]. These approaches include separate resurfacing of the medial and patellofemoral compartments [19], monoblock off-the-shelf BKA prostheses [10, 20], and patient-specific custom monoblock BKA prostheses [22]. The Journey Deuce™ prosthesis was developed as an off-the-shelf monoblock BKA, available in six sizes, to provide a minimally invasive alternative to TKA for bicompartmental disease [10, 20]. Similar to UKA, this prosthesis spares both cruciate ligaments and the healthy lateral compartment for patients with diseased medial and patellofemoral compartments. A monoblock BKA has potential advantages over the use of separate medial and patellofemoral compartmental implants because there are fewer parts with a correspondingly simpler surgical procedure [20].
Previous studies on the clinical and functional performance of monoblock BKA have reported mixed conclusions. Monoblock BKA has been reported to produce good results that restore mechanical alignment and have kinematics similar to healthy knees during daily motor tasks [10, 12, 21, 27]. Monoblock BKA also showed positive results when compared with TKA in biomechanical studies [28]. However, other studies reported monoblock BKA provided inconsistent pain relief and functional outcomes, poor short-term survival with high revision rates, leading the authors not to recommend monoblock BKA as an alternative to TKA and UKA [16, 18, 24, 25]. These inconsistent findings motivate further study to determine whether off-the-shelf monoblock BKA consistently provides knee function similar to UKA.
No study has yet reported intra-articular dynamic motions in patients with monoblock BKA, and thus, there remain open questions whether these devices maintain close-to-physiologic knee mechanics and whether clinically variable results are manifestations of inconsistent mechanics at the joint level. Therefore, the purpose of this study was to analyse the 3D kinematics of knees with monoblock BKA in three weight-bearing activities to address two questions: (1) Do knees with off-the-shelf monoblock BKA show stable kinematics consistent with retained cruciate ligament and lateral compartment function? and (2) Are kinematics in knees with monoblock BKA as consistent as those previously reported for TKA and UKA?
Methods and materials
Ten patients (nine female and one male) enrolled in this study. Preoperative inclusion criteria required subjects having painful medial and patellofemoral osteoarthritis, intact anterior and posterior cruciate ligaments, varus deformity less than 15°, maximum 10° flexion contracture, arthritic degeneration of Outerbridge grade 3–4 for the medial and patellofemoral joints, and Outerbridge 0–1 for the lateral compartment. Intraoperative assessment confirmed Outerbridge grade 4 disease in the medial compartment of all ten knees, Outerbridge grade 3–4 (four knees) and grade 4 (six knees) for the patellofemoral compartment, and maximum Outerbridge grade 0–1 for the lateral compartment in all ten knees. Post-operative inclusion criteria required knee motion from full extension to 120° flexion and the ability to perform the study exercises. Subjects had to consent to a post-operative CT scan, the fluoroscopic examination, and unreimbursed travel to the study site. The strict inclusion/exclusion criteria, and high demands upon subjects to participate, limited enrolment to ten patients from the 64 patients who received this prosthesis at a single clinic (16 %).
At the time of the surgery, the patients averaged 65 (5) years with average 28 (2) BMI. Each subject received unilateral Journey Deuce™ (Smith & Nephew Orthopedics, Memphis, TN) BKA with both cruciate ligaments retained an average of 2.6 (0.6) years prior to this study. Analysis of post-operative CT scans and clinical films showed 2° (3°) correction of varus deformity, 0° (7°) change in medial tibial posterior slope, 2 mm (2 mm) elevation of the medial joint line, 7° (4°) internal rotation of the femoral component relative to the surgical transepicondylar axis, and 9° (8°) external rotation of the medial tibial component relative to the tibial plateau. Skyline views of the post-operative patellofemoral joint showed an average lateral patellar tilt of 9° (8°) relative to the prosthetic femoral trochlea. At the time of the study, mean clinical outcome scores were 97 (3) and 95 (7) for the Knee Society knee and function scores, 16.4 (4.8) for the Oxford Knee Score, and 6.5 (0.9) for the UCLA activity score and knees had an average 137° (4°) range of motion.
Bone and implant models were segmented from post-operative CT scans of the knee (DICOM format images, 512 × 512 image matrix, average pixel dimensions of 0.2818 × 0.2818 mm, with average 0.8 mm slice thickness) using manual segmentation with open-source software (ITK-Snap, www.itksnap.org). Surface models of the implants were registered to the segmented implant surfaces to provide a higher fidelity model for model-image registration with a composite of bone and implant [5]. Metal artefact significantly affected the CT image quality of the lateral femoral condyle, so the surface of the segmented lateral condyle was reconstructed using spherical patches fitted to the posterior and distal condylar surfaces (Fig. 1). Femoral and tibial articular surfaces were subdivided until the distance between adjacent surface points was less than 0.5 mm. The femoral bone/implant model was aligned to a coordinate system similar to that frequently used for TKA implants [14, 15]. The tibial coordinate system was determined following previously reported procedures (Fig. 2, [4]). Briefly, the centroid of the tibial transverse section at 40, 55, and 70 mm from the articular surface was determined, and the superoinferior axis was the best-fit line through these points (Geomagic Studio, Geomagic Inc., Morrisville, NC). The tibial origin was taken to be the point where the superior/inferior axis intersected the proximal surface of the tibia. The anteroposterior axis intersected the origin and defined a sagittal plane intersecting a point 10 mm medial to midpoint of the tibial tubercle. The mediolateral axis was determined as the cross product of the superoinferior and anteroposterior axes.
The tibial coordinate system was aligned with the tibial shaft (left) and oriented so the anteroposterior axis was 10 mm medial of the midpoint of the tibial tubercle (right, [4])
Patients were observed using dynamic fluoroscopy during lunge, kneeling, and step-up/step-down activities [5, 8, 14, 15]. For lunge and kneeling activities, the patients were asked to apply their full body weight to achieve maximum comfortable knee flexion. 3D–2D model-image registration techniques were used to determine 3D knee kinematics (Fig. 3, [6]). The femoral implant model and the tibia/fibula/implant models were projected onto the undistorted fluoroscopic images, and the position and orientation of the models were adjusted to match the projected images using open-source software (sourceforge.net/projects/jointtrack). Measurement uncertainties for the femoral or tibial poses are ±1 mm for sagittal translations and ±1° for any rotation [1, 6, 13]. An average of 62 (13) fluoroscopic images per knee was used for quantifying knee kinematics during the step-up/step-down activity. Images showing the greatest knee flexion were used for lunge and kneeling.
Knee rotations were determined using Cardan/Euler angles and analysed as a function of flexion angle [26]. Since natural proximal tibial geometry is so varied, all the joint rotations and translations are reported relative to the knee pose in 5° weight-bearing flexion [5, 15]. The anteroposterior translations of the medial and lateral condyles were determined by computing a distance map between the prosthetic medial and reconstructed lateral femoral condyles and the tibial articular surfaces. The estimated contact locations were computed as the geometric centroid of all surface points having less than 5 mm separation [2, 11]. Cubic spline interpolation was used to resample the kinematics of each knee at 5° flexion increments for group statistics.
This study was reviewed and approved by the Freiburger Ethik-Kommission International (09/1392) and by the University of Florida Institutional Review Board (286-2011).
Statistical analysis
Representative kinematic parameters for the BKA knees were determined as the mean (standard deviation). Comparisons of kinematics across activities were performed using paired t tests. Relationships between implant alignment and knee kinematics were explored using univariate linear regression.
Results
Knee kinematics during maximum flexion lunge and kneeling activities showed the medial condyle remained central on the tibia, while the lateral condyle translated posteriorly with external femoral rotation (Table 1). Flexion was greater during the kneeling activity (p = 0.004), but the other knee pose parameters were not significantly different. The tibia internally rotated an average of 10° (6°) and 12° (10°) for the lunge and kneel postures, respectively.
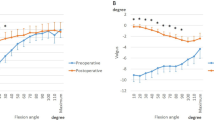
For the step-up/step-down activity, average tibial internal rotation increased slightly less than 2° from 5° to 70° flexion (Fig. 4). The range of tibial rotation for individual knees averaged 6° (5°). Tibial rotation varied an average of 7° at 70° flexion. Both condyles showed posterior translation to mid-flexion, then medial condylar anterior translation to 70°. Nine out of ten knees showed some posterior condylar translation from extension to early flexion.
Kinematics for ten knees with monoblock BKA during step-up/step-down activity: Tibial internal rotation (top) increased an average of 2° from extension to 70° flexion but was highly variable. Medial (middle) and lateral (bottom) condylar contact moved posteriorly from extension to 35° flexion, and medial contact moved anterior from 35° to 70° flexion. Thin grey lines show kinematics for each knee, the thick black line represents the mean for ten knees, and the shaded region indicates one standard deviation above and below the mean
Linear regression analysis of implant-to-bone alignment and joint kinematics showed the greatest correlations between increased tibial component posterior slope and total medial condylar translation (R 2 = 0.47) and average tibial rotation angle (R 2 = 0.42). The correlation between change in posterior tibial slope, either less or more, and increased medial condyle translation was even greater (R 2 = 0.65). All other correlations between surgical alignment measures and joint kinematics had R 2 values less than 0.30.
Discussion
Knees with monoblock BKA show evidence of retained cruciate ligaments but highly variable kinematics in patients with excellent clinical outcomes. Kinematics were evaluated during three weight-bearing activities in knees with minimum 2-year follow-up in a cohort of subjects with excellent clinical outcomes. The anteroposterior knee translations were stable and consistent with intact cruciate function, but the knee rotations and absolute locations of condylar contact were highly variable (Fig. 4). Our observations may help explain the mixed results for monoblock BKA found in previous studies and point to areas where technical improvements could yield more consistently successful results with this treatment.
An important potential benefit to any available BKA treatment is retention of the cruciate ligaments and maintenance of more natural knee function. We observed a centralized medial condyle and posteriorly translated lateral condyle during deep flexing, weight-bearing activities (Table 1). Maximum flexion and tibial internal rotation during lunge and kneeling activities were comparable to previously reported UKA and well-performing TKA subjects [5, 15]. For step-up/step-down activity, the femoral condyles showed posterior translation to mid-flexion, with the medial condyle returning to a centralized AP position at 70° flexion. Kinematics for these BKA knees were closer to previously reported kinematics of knees with UKA than TKA, as expected, due to the fact that the cruciate ligaments were retained and the native lateral compartment was unaltered [5]. Only one knee showed evidence of anterior femoral translation during early flexion, indicating retained integrity of natural AP stabilizing structures in the remaining nine knees. More specifically, posterior femoral translations in early flexion and the tibiofemoral pose in deeper flexion indicate retained cruciate ligament function [14, 15]. These results agree with previously reported studies for arthroplasties that retained the cruciate ligaments [12, 27, 28].
The knees in this study showed excellent or good clinical outcomes and functional scores, and relatively high activity levels, but there still was very high variability of tibial rotation between patients. Our post-operative measures of implant surgical alignment showed a large range of axial implant alignment for the femoral and tibial implants and a similarly large range of tibial component posterior slope. The amount of tibial rotation during the stair activity (6° ± 5°) was more variable than previously reported for bicruciate-retaining TKA (7° ± 4°) [15], bicondylar UKA (4° ± 3°) [5], UKA (10° ± 3°) [5], or conforming PCL-retaining TKA (7° ± 2°) [7] for the same activity studied using the same methods. This high variability, in a relatively small group of high-performing knees, likely predicts greater variability of knee function in unselected cohorts, where high variability of clinical outcomes has been reported [16, 18]. Müller et al. [16] reported it was technically demanding to align monoblock BKA femoral implants with the six available sizes, and it is reasonable to assume technically demanding procedures will produce more variable results.
Partial or TKA retaining one or both cruciate ligaments has intrinsic uncertainty whether the retained ligaments will function normally after surgery. Knees receiving arthroplasty are diseased, and there is abundant evidence the ligaments are not normal [17]. Resurfacing the medial compartment in appropriate patients can result in near-normal knee kinematics [5], while bicondylar UKA [5] and bicruciate-retaining TKA [15] show less normal kinematics despite retention of both cruciate ligaments. The monoblock BKA knees showed a range of kinematics, in the spectrum between previously reported UKAs and multicompartmental arthroplasties, consistent with resurfacing two diseased knee compartments. In addition, we found reasonably strong correlations between changing the medial tibial posterior slope and greater medial condylar translations, showing kinematics are sensitive to articular surface changes in the cruciate ligament-intact knee. Despite observing less early stiffness, reducing bone resection, and the ability to retain both cruciates with BKA, Müller et al. [16] reported their preference for TKA because of fewer complications and greater consistency of outcomes. Furthermore, Chung and Min recently found no difference in muscle strength or physical performance 1 year after modular BKA or posterior-stabilized TKA, suggesting the theoretical benefits of BKA had not been realized [9].
This study has two important limitations. First, the study cohort was limited to 10 subjects representing 16 % of the clinical cohort. These subjects were included because they had good range of motion and functional outcomes, and they were willing to participate. It is reasonable to assume these subjects represent some of the best performers of this clinical cohort, so that study of the broader population with this treatment would reveal even more variation in knee kinematics. Second, kinematics during a limited set of activities were observed. It is reasonable to expect a wider range of dynamic loads, e.g. during gait, would reveal even more variability between knees, so it is unlikely this limitation would change conclusions based upon observation of deep flexion and step activities.
Conclusion
Monoblock bicompartmental arthroplasty appears to permit functional retention of the cruciate ligaments, consistent with functionally stable knees. However, knee kinematics were not consistent in a relatively small group of high-performing study subjects. Further study is required to identify sources of high variability in the kinematics, such as optimal implant locations, cruciate ligament integrity, and tensioning. Future efforts should focus on providing surgeons objective guidance for optimal implant positioning and sizing and, presumably, more consistent knee kinematics.
References
Acker S, Li R, Murray H, John PS, Banks S, Wyss U, Deluzio K (2011) Accuracy of single-plane fluoroscopy in determining relative position and orientation of total knee replacement components. J Biomech 44:784–787
Adam C, Eckstein F, Milz S, Schulte E, Becker C, Putz R (1998) The distribution of cartilage thickness in the knee-joints of old-aged individuals measurement by A-mode ultrasound. Clin Biomech 13:1–10
Argenson J-NA, Guillaume JM, Aubaniac JM (1995) Is there a place for patellofemoral arthroplasty? Clin Orthop Relat Res 321:162–167
Banks SA (2009) Haptic robotics enable a systems approach to design of a minimally invasive modular knee arthroplasty. Am J Orthop (Belle Mead. NJ) 38:23–27
Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S (2005) Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sport Traumatol Arthrosc 13:551–556
Banks SA, Hodge WA (1996) Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng 43:638–649
Banks SA, Hodge WA (2004) 2003 Hap Paul Award Paper of the International Society for technology in arthroplasty: design and activity dependence of kinematics in fixed and mobile-bearing knee arthroplasties. J Arthroplast 19:809–816
Banks SA, Markovich GD, Hodge WA (1997) The mechanics of knee replacements during gait. In vivo fluoroscopic analysis of two designs. Am J Knee Surg 10:261–267
Chung JY, Min B-H (2013) Is bicompartmental knee arthroplasty more favourable to knee muscle strength and physical performance compared to total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 21:2532–2541
Engh GA (2007) A bi-compartmental solution: what the Deuce? Orthopedics 30:770–771
Koo S, Gold GE, Andriacchi TP (2005) Considerations in measuring cartilage thickness using MRI: factors influencing reproducibility and accuracy. Osteoarthr Cartil 13:782–789
Leffler J, Scheys L, Planté-Bordeneuve T, Callewaert B, Labey L, Bellemans J, Franz A (2012) Joint kinematics following bi-compartmental knee replacement during daily life motor tasks. Gait Posture 36:454–460
Moro-oka T, Hamai S, Miura H, Shimoto T, Higaki H, Fregly B, Iwamoto Y, Banks S (2007) Can magnetic resonance imaging-derived bone models be used for accurate motion measurement with single-plane three-dimensional shape registration? J Orthop Res 25:867–872
Moro-oka TA, Hamai S, Miura H, Shimoto T, Higaki H, Fregly BJ, Iwamoto Y, Banks SA (2008) Dynamic activity dependence of in vivo normal knee kinematics. J Orthop Res 26:428–434
Moro-oka TA, Muenchinger M, Canciani JP, Banks SA (2007) Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg Sport Traumatol Arthrosc 15:93–99
Müller M, Matziolis G, Falk R, Hommel H (2012) The bicompartmental knee joint prosthesis Journey Deuce: failure analysis and optimization strategies. Orthopade 41:894–904
Nelissen RG, Hogendoorn PC (2001) Retain or sacrifice the posterior cruciate ligament in total knee arthroplasty? A histopathological study of the cruciate ligament in osteoarthritic and rheumatoid disease. J Clin Pathol 54:381–384
Palumbo BT, Henderson ER, Edwards PK, Burris RB, Gutiérrez S, Raterman SJ (2011) Initial experience of the journey-deuce bicompartmental knee prosthesis: a review of 36 cases. J Arthroplast 26:40–45
Parratte S, Pauly V, Aubaniac J-M, Argenson J-NA (2009) Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clin Orthop Relat Res 468:64–72
Rolston L, Bresch J, Engh G, Franz A, Kreuzer S, Nadaud M, Puri L, Wood D (2007) Bicompartmental knee arthroplasty: a bone-sparing, ligament-sparing, and minimally invasive alternative for active patients. Orthopedics 30:70–73
Rolston L, Siewert K (2009) Assessment of knee alignment after bicompartmental knee arthroplasty. J Arthroplast Elsevier Inc 24:1111–1114
Steinert A, Nöth U, Rudert M (2013) The individual-template system combined with individual endoprosthesis: ConforMIS iUni G2, iDuo G2, and iTotal G2. In: Haaker R, Konermann W (eds) Computer and Template Assisted Orthopedic Surgery, Springer, Berlin, pp 53–62
Swienckowski JJ, Pennington DW (2004) Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am 86(A Suppl):131–142
Thienpont E, Price A (2013) Bicompartmental knee arthroplasty of the patellofemoral and medial compartments. Knee Surg Sports Traumatol Arthrosc 21:2523–2531
Tria AJ (2013) Bicompartmental knee arthroplasty: the clinical outcomes. Orthop Clin North Am 44:281–286
Tupling SJ, Pierrynowski MR (1987) Use of Cardan angles to locate rigid bodies in three-dimensional space. Med Biol Eng Comput 25:527–532
Wang H, Dugan E, Frame J, Rolston L (2009) Gait analysis after bi-compartmental knee replacement. Clin Biomech Elsevier Ltd 24:751–754
Wünschel M, Lo J, Dilger T, Wülker N, Müller O (2011) Influence of bi- and tricompartmental knee arthroplasty on the kinematics of the knee joint. BMC Musculoskel Disord 12:7
Acknowledgments
This work was sponsored by research grants to the authors’ institutions from Smith & Nephew plc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, B.H., Leffler, J., Franz, A. et al. Kinematics of monoblock bicompartmental knee arthroplasty during weight-bearing activities. Knee Surg Sports Traumatol Arthrosc 23, 1756–1762 (2015). https://doi.org/10.1007/s00167-014-3427-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3427-1