Abstract
The purpose of this study was to compare knee kinematics in patients with bi-cruciate preserving total knee arthroplasty and posterior cruciate ligament (PCL) preserving total knee arthroplasty. Five knees received PCL-retaining arthroplasty and nine knees received both cruciate-retaining arthroplasty (ACL/PCL knees). We studied treadmill gait, stair stepping, and maximum flexion activities using lateral fluoroscopy and shape matching. For maximum flexion, the ACL/PCL knees showed 6 mm more posterior translation of the lateral condyle (p < 0.05). For the stair activity, posterior translations of the lateral condyle were significantly greater in the ACL/PCL knees from 30° to 70° flexion (p < 0.05). Both condyles in the ACL/PCL knees showed greater posterior translation in the stance and swing phases of gait than in the PCL knees (p < 0.05). Preserving both cruciate ligaments in total knee arthroplasty appears to maintain some basic features of normal knee kinematics in these activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL)-retaining total knee arthroplasty (TKA) is uncommon despite reports of good clinical results [13, 23, 32]. The ACL is sacrificed in the vast majority of TKA prostheses, where the debate has focused on the role of the posterior cruciate ligament (PCL) [8–10, 14, 20, 26, 28, 30, 31, 34]. Proponents of retaining the PCL have argued; it enhances stability, allows femoral roll back, decreases shear forces between implant and bone, and preserves proprioception. Theoretically, ACL retention should provide more physiologic stability, kinematics, and proprioception [4, 16].
The role of ACL in knee kinematics had been studied by several authors. Kärrholm et al. [25] showed that internal rotation and adduction of the tibia were reduced in ACL-injured knees when compared with intact knees in their roentgen stereophotogrammetric examination. Berchuck et al. [11] showed the so-called quadriceps-avoidance gait in patients with unilateral ACL deficiency. Both studies suggested that it is difficult to maintain normal kinematics in the ACL-deficient knee. The same arguments should apply to the knee after TKA. Andriacchi et al. [4] showed that patients treated with the least-constrained bi-cruciate-retaining design of prosthesis were the only group that had a normal range of motion during gait. ACL integrity also affects the survival rate of unicondylar knee arthroplasty [16].
Recently, the kinematics of many knee replacement designs have been characterized using fluoroscopy [5–10, 14, 15, 17, 24, 27, 31, 36], but few ACL-retaining designs have been analyzed. Stiehl et al. [36] compared ACL-retaining TKA and PCL-retaining TKA of different designs for knee bending motions at 0°, 30°, 60°, and 90° flexion. ACL-retaining TKAs showed gradual posterior femoral rollback and limited anterior–posterior translation, but remained posterior to the sagittal plane midline in all positions. Komistek et al. [27] compared ACL-retaining TKA and posterior-substituting TKA in gait motion. Using images at 0, 33, 66, and 100% of stance phases, they concluded that kinematics of the ACL-retaining knees were more similar to the normal knee during gait. These two studies provide important and useful information, but it is not possible to develop a detailed description of knee motions from only four snapshots during one activity. Unicondylar knee arthroplasty can also preserve both cruciate ligaments. Banks et al. [5] studied the kinematics of bi-cruciate-retaining unicondylar and bi-unicondylar knee arthroplasties and found that knee motions during gait, stair-stepping, and deep flexion activities were closer to normal in the knees with bi-cruciate-retaining unicondylar arthroplasty.
The goal of this study was to compare knee kinematics in groups of patients at mid-term follow-up having the same operative procedure by the same surgeon and PCL or ACL/PCL variants of the same prosthesis design. We hypothesized that patients with an intact ACL would show more physiologic antero-posterior (AP) translation of the knee with flexion/extension.
Materials and methods
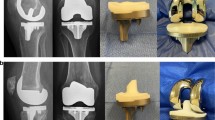
Twelve patients with 14 knee arthroplasties were studied. All patients provided written consent for this IRB approved study. Patients were recruited at clinical follow-up based solely on their having the specific prostheses of interest and their willingness to participate in the study. All patients had surgery by a single surgeon (J.P.C.). Five knees received PCL-retaining arthroplasty (Natural-Knee®, Zimmer GmbH, Winterthur, Switzerland) and nine knees received ACL/PCL-retaining arthroplasty using the same femoral component and a tibial baseplate shaped to permit ACL retention (N2C, Zimmer GmbH, Winterthur, Switzerland) (Table 1). The tibial articular surfaces were similar. The ACL/PCL-retaining plateau was flat, whereas the PCL-retaining plateau had a central flat region bounded by slight dishing at both anterior and posterior margins. The main difference between groups was retention or sacrifice of the ACL at the time of surgery. The components were placed to reproduce normal anatomical joint surfaces, including slope and joint line.
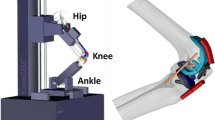
Patients’ knee motions were recorded using lateral fluoroscopy during treadmill gait at 1 m/s, single limb stepping up and down on a 25 cm stair, maximum flexion in a lunge with the foot placed on the 25 cm step, maximum flexion kneeling on a padded stool, and weight-bearing straight-leg stance. The images were recorded on digital videotape at 30 frames/s for gait and 10 frames/s for all other activities. Gait data were available for seven of the nine ACL/PCL knees (Fig. 1). The digitized images were corrected for optical distortion using bilinear interpolation [7]. The Canny edge detector was used to identify the implant boundaries [12].
The three-dimensional position and orientation of the proximal and distal knee segments were determined using a toolbox of model-based shape-matching techniques, including previously reported techniques [7], manual matching, and automated matching using nonlinear least-squares (modified Levenberg–Marquardt) techniques. Three thousand nine hundred and twenty fluoroscopic images, an average of 280 images per knee, were analyzed. The optical geometry of the fluoroscopy system (principal distance, principal point) was determined from images of a calibration target [7]. The implant surface model was projected onto the geometry-corrected image, and its three-dimensional pose was iteratively adjusted to match its silhouette with the silhouette of the subject’s knee components. The results of this shape-matching process have standard errors of approximately 0.5° to 1.0° for rotations and 0.5–1.0 mm for translations in the sagittal plane [7].
Joint kinematics were determined from the three-dimensional pose of each TKA component using Cardan/Euler angles [38]. The anterior/posterior locations of each condyle were determined by transforming the joint pose into a reference system parallel to the transverse plane of the flat tibial component and finding the lowest point on each condyle.
For the stair, kneeling, and lunge activities, kinematics were expressed relative to the joint pose in straight-leg weight-bearing stance. For gait, the kinematics was expressed relative to the joint pose at heel-strike. Kneeling and lunge data were compared using t tests. In addition, linear regression analysis was performed to characterize the trends in tibial rotation and condylar translation as a function of knee flexion, combining the PCL and ACL/PCL knees. For the stair and gait data, an average curve for each knee was created from four trials of data. These average curves were then combined to create group averages. Statistical comparisons for the stair and gait data were performed using a two-factor, repeated-measures analysis of variance (ANOVA) with post hoc pair-wise comparisons (Tukey’s honestly significant difference or T-HSD). The level of significance was set at p ≤ 0.05.
Results
For the kneeling and lunge activities, there were no differences between the PCL and ACL/PCL knees for maximum flexion, tibial rotation, or medial translation (Table 2). In the lunge activity, the lateral condyle in ACL/PCL knees was in a more posterior location than in the PCL knees (p < 0.05). For all knees combined, the maximum flexion angle has only weak correlation with tibial rotation during kneeling (r = 0.42). The condylar contact positions did not have statistically significant correlations with maximum flexion angle (Table 3).
There was a significant difference in tibial rotation between the ACL/PCL and PCL knees. For stair and gait activities, the ACL/PCL knees showed an average of 4.9° more tibial internal rotation (p ≪ 0.01, RM-ANOVA) than the PCL knees. This rotational offset also manifests itself as a more anterior AP position of the medial condyle in the ACL/PCL knees during gait (p = 0.04). From extension to flexion during the stair activity, knees in both groups showed linear tibial internal rotation from 0° to 70° of flexion, 6.5° in the ACL/PCL knees, and 4.3° in the PCL knees (p > 0.05). The range of tibial rotation during the stance phase of gait was 5.9° for the ACL/PCL knees and 4.3° for the PCL knees (p > 0.05).
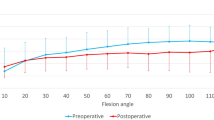
For the stair activity, there were greater posterior translations of the medial and lateral condyles in the ACL/PCL group (Fig. 2). From 20° to 70° flexion, these posterior condylar translations were significantly greater in the ACL/PCL knees (ANOVA, p ≪ 0.01). Both groups showed maximum medial condyle posterior translation at 50° flexion, 1 mm in the PCL knees and 3.5 mm in the ACL/PCL knees. Posterior lateral condylar translations averaged 1 mm from 0° to 70° in the PCL knees and 6 mm in the ACL/PCL knees.
Knee kinematics during stair differed between the ACL/PCL and PCL knees (mean ± 1 standard deviation). AP translations of the medial (top) and lateral (bottom) condyles are shown. Posterior translations of the medial and lateral condyles were significantly greater in the ACL/PCL knees (ANOVA, p ≪ 0.01), with significant pair-wise differences from 20° to 70° flexion (T-HSD, p < 0.05)
The ACL/PCL knees showed greater knee flexion than the PCL knees all through the gait cycle, with statistically significant pair-wise differences from the last part of swing phase to the middle of the stance phase (p < 0.05) (Fig. 3a). The ACL/PCL knees showed greater tibial internal rotation throughout the gait cycle (p ≪ 0.01), but there were no statistically significant pair-wise differences (Fig. 3b). The ACL/PCL knees showed greater posterior condylar translation than the PCL knees in the middle of stance and swing phases of gait (p < 0.05) (Fig. 3c, d).
Knee kinematics during gait differed between the ACL/PCL and PCL knees (mean ± 1 standard deviation). a The ACL/PCL knees showed significantly greater flexion from the last part of swing to the middle stance. b ACL/PCL knees showed greater tibial internal rotation. c, d Both condyles in ACL/PCL group have greater posterior translation in the middle of both stance and swing phase than in PCL group. Data zeroed at heel-strike (c, d). The two gray regions on each graph indicate gaps in the fluoroscopic data, when the contralateral knee occludes the view, which are filled by interpolation
Discussion
Many factors, including operative procedures, prosthesis design, and different weight-bearing activities, affect knee kinematics after TKA [4, 8, 9, 31]. We measured knee motions during four activities in two groups of knees with unicruciate or bi-cruciate sparing variants of the same TKA design. Kneeling and lunge activities were analyzed at maximum knee flexion, whereas gait and stair activities were analyzed over the entire motion cycle. The ACL-retaining knees showed greater tibial internal rotation and posterior translations during the maximum flexion activities.
The dominant motions of the knee during deep flexion consist of posterior translation and external rotation of the femur with respect to the tibia. Static MRI studies of normal knees have shown that the lateral condyle translated more than the medial condyle in deep knee flexion [19, 22]. The ACL/PCL knees showed greater posterior translation of the lateral condyle than PCL knees during the kneeling and lunge activities. But greater condylar translations in the ACL/PCL knees did not result in greater maximum flexion in either activity. MRI studies of healthy knees in deeply flexed postures show tibial rotations up to 28°, whereas we observed rotations averaging 5–10° in maximum flexion. These findings are consistent with previous studies of deep flexion with TKA that have shown tibial rotation is less than normal, that maximum flexion is not correlated to the amount of tibial rotation, and that tibial rotation appears to be primarily determined by limb position in sitting and squatting postures [24]. It seems likely that force equilibrium in deep flexion is reached with different condylar translations and tibial rotations in meniscal intact and deficient knees.
The ACL/PCL and PCL knees showed approximately 20° less maximum flexion during lunge and kneeling activities than passive flexion measured in the clinic. Two factors likely explain this difference. First, fluoroscopically measured flexion angles represent the angle between the implant components and do not account for the component alignment with respect to the bones. Banks et al. [6] showed that anterior bow of the femur and posterior slope of the tibial plateau place the prostheses in approximately 9° of hyperextension relative to the sagittal mechanical axis of the bones. The ACL/PCL and PCL knees had an average implant hyperextension of 10° relative to the sagittal mechanical axis. Second, muscle contraction and joint pose can also affect maximum flexion in weight-bearing activities. Several previous TKA studies have shown greater maximum knee flexion in non-weight-bearing positions compared with weight-bearing positions [18, 29]. These factors may have accounted for about 10° difference between the weight-bearing and clinical flexion measures in the ACL/PCL and PCL knees.
Two dynamic activities were analyzed in this study: treadmill gait and a stair activity. For both stair and gait activities, the PCL knees showed a 5° bias of tibial external rotation compared with the ACL/PCL knees. This rotational bias could have resulted from at least three factors: baseplate alignment, tibial insert geometry, or ACL integrity. First, the measured tibial rotation is determined from the orientation of the implanted components, so differences in baseplate alignment would result in a rotational bias. However, a single surgeon implanted all components using identical alignment techniques and anatomic references. Second, the ACL/PCL and PCL-only tibial inserts have only slightly different geometries. Both surfaces are flat in the mid-range of translation, and tibiofemoral contact was confined mostly to this articular region. Therefore, it is unlikely that the articular surfaces imposed a tibial rotation offset. Third, the rotational bias could have resulted from the presence or absence of the ACL. Andriacchi and Dyrby [3] reported a comparison of knee kinematics in healthy and ACL-deficient knees, and found an average 2.9° less tibial external rotation in the ACL-deficient knees. This rotational difference is opposite to the difference observed in this study, where the ACL-deficient knees (PCL knees) exhibited greater tibial external rotation. However, the rotational bias observed in the knee replacement patients is consistent with kinematics and wear patterns on retrieved implants [17] and suggests that the medial meniscus (lacking in TKA) may play an important role in the axial alignment of the ACL-deficient knee. Finally, the ACL-retaining TKA procedure is potentially more difficult than that retaining only the PCL, such that other surgical factors may introduce a bias in axial knee alignment.
Dynamic condylar translations in the PCL knees were smaller than previously has been reported for normal knees in dynamic and static studies, including stair and gait activities [15, 19, 22, 35]. The finding is consistent with some prior in vivo studies of PCL-retaining TKA [14]. Condylar translations were greater in the ACL/PCL knees during the stair activity, with most translation taking place in the first 30–40° flexion. Not surprisingly, similar kinematics have been observed during stair-stepping in ACL/PCL-retaining bi-unicondylar knee replacements [5]. Similar kinematics have also been observed for knee bending motions with ACL-retaining TKA [36]. Stair kinematics in the ACL/PCL knees showed similar patterns to normal knees during a knee bending motion [15]. Medial translations were similar, but lateral condylar translations were much greater in the normal knees, presumably due to the convex geometry and mobile meniscus of the intact knee. ACL/PCL knee kinematics during gait were also similar to previous studies of normal knees and ACL-retaining replaced knees. Both condyles moved posterior twice within the gait cycle. This biphasic tibiofemoral translation has been reported in the normal knee [35], and in unicondylar and bi-unicondylar replaced knees [5]. We observed greater medial than lateral condylar translations during gait, similar to the motions observed in ACL/PCL-retaining bi-unicondylar knees [5]. Only one study has reported in vivo gait kinematics of knees with ACL-retaining TKA [27], but there is poor correspondence with motions from the present study. It is possible that the poor correspondence results from experimental differences: the current study utilized treadmill gait images at 30 frames/s for a minimum of four gait cycles (120 images per knee), whereas the prior study processed four equispaced images from the first stance phase upon gait initiation.
The apparent paradox of this study is that smaller dynamic tibiofemoral translations were observed in the presumably less stable PCL-retaining knees than in the cruciate intact ACL/PCL knees. One could reasonably expect the ACL-deficient and unconstrained PCL knees to show abnormal magnitudes and directions of translation, as have been observed in many total knee replacements [8–10, 14, 30, 31]. In vitro and computational studies suggest greater tibiofemoral translation occurs after loss of the ACL [35, 37], but several in vivo studies show tibiofemoral translations are not necessarily increased [3, 25, 30]. In vivo studies with ACL-deficient knees suggest that there can be significant differences in knee function determined by adaptation in muscle firing patterns, especially ACL agonist cocontraction of the hamstrings [1, 2]. Thus, it is possible that the patients in the PCL group had adapted their muscle activation and gait patterns to provide extrinsic AP knee stability. Although we cannot support this suggestion with electromyographic data, their relatively stiff-legged gait during stance phase gives one indication that the PCL knee patients had adapted their muscle firing and gait pattern to accommodate higher intrinsic knee laxity [4, 25].
Patients with bilateral TKAs of two types have preferred either their bi-cruciate-retaining knee or intrinsically stable medial pivot prosthesis [33]. This study showed that the ACL/PCL-retaining knees exhibited more physiologic patterns of motion, despite having clinical scores comparable to the PCL knees. It is possible that knees retaining the cruciate ligaments feel more normal and require fewer dynamic adaptations for daily function [1, 2]. The data support the conclusion that the ACL is not necessary to have a well functioning, clinically successful, and durable knee arthroplasty, but that ACL retention can lead to a knee arthroplasty with more normal kinematics in maximally flexed postures.
References
Alkjaer T, Simonsen EB, Jørgensen U, Dyhre-Poulsen P (2003) Evaluation of the walking pattern in two types of patients with anterior cruciate ligament deficiency: copers and non-copers. Eur J Appl Physiol 89:301–308
Alkjaer T, Simonsen EB, Magnusson SP, Aagaard H, Dyhre-Poulsen P (2002) Differences in the movement pattern of a forward lunge in two types of anterior cruciate ligament deficient patients: copers and non-copers. Clin Biomech 17:586–593
Andriacchi TP, Dyrby CO (2005) Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech 38:293–298
Andriacchi TP, Galante JO, Fermier RW (1982) The influence of total knee replacement design on walking and stair climbing. J Bone Joint Surg Am 64A:1328–1335
Banks SA, Fregly BJ, Boniforti F, Reinschmidt C (2005) Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports Traumatol Arthrosc 13:193–196
Banks SA, Harman MK, Hodge WA (2002) Mechanism of anterior impingement damage in total knee arthroplasty. J Bone Joint Surg Am 84A:37–42
Banks SA, Hodge WA (1996) Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE Trans Biomed Eng 43:638–649
Banks SA, Hodge WA (2004) Design and activity dependence of kinematics in fixed and mobile bearing knee arthroplasties. J Arthroplasty 19:809–816
Banks SA, Hodge WA (2004) Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop 426:187–193
Banks SA, Markovich GD, Hodge WA (1997) In vivo kinematics of cruciate retaining and substituting knee replacements. J Arthroplasty 12:297–304
Berchuck M, Andriacchi TP, Bach BR, Reider B (1990) Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am 72A:871–877
Canny JA (1986) Computational approach to edge detection. IEEE Trans Pattern Anal Mach Intell 8:679–698
Cloutier JM, Sabouret P, Deghrar A (1999) Total knee arthroplasty with retention of both cruciate ligaments: a nine to eleven-year follow-up study. J Bone Joint Surg Am 81A:697–702
Dennis DA, Komistek RD, Mahfouz MR, Hass DB, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop 416:37–57
Dennis DA, Mahfouz MR, Komistek RD, Hoff W (2005) In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38:241–253
Goodfellow J, O’Connor J (1992) The anterior cruciate ligament in knee arthroplasty: a risk-factor with unconstrained meniscal prostheses. Clin Orthop 276:245–252
Harman MK, Banks SA, Hodge WA (2001) Polyethylene damage and knee kinematics after total knee arthroplasty. Clin Orthop 392:383–393
Hass BD, Komistek RD, Dennis DA (2002) In vivo kinematics of the low contact stress rotating platform total knee. Orthopedics 25:s219–s226
Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MAR (2000) Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br 82B:1196–1198
Insall JN (1988) Presidential address to the knee society: choices and compromises in total knee arthroplasty. Clin Orthop 226:43–48
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop 248:13–14
Iwaki H, Pinskerova V, Freeman MAR (2000) Tibio-femoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82B:1189–1195
Jenny JY, Jenny G (1998) Preservation of anterior cruciate ligament in total knee arthroplasty. Arch Orthop Trauma Surg 118:145–148
Kanekasu K, Banks SA, Honjo S, Nakata O, Hiromi K (2004) Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty 19:998–1003
Kärrholm J, Selvik G, Elmqvist LG, Hansson LI (1988) Active knee motion after cruciate ligament rupture. Acta Orthop Scand 59:158–164
Kim YH (1990) Knee arthroplasty using a cementless PCA prosthesis with a porous coated central tibial stem. J Bone Joint Surg Br 72B:412
Komistek RD, Allain J, Anderson DT, Dennis DA, Goutallier D (2002) In vivo kinematics for subjects with and without an anterior cruciate ligament. Clin Orthop 404:315–325
Misra AN, Hussain RA, Fiddian NJ, Newton G (2003) The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg Br 85B:389–392
Myles CM, Rowe PJ, Walker CRC, Nutton RW (2002) Knee joint functional range of movement prior to and following total knee arthroplasty measured using flexible electrogoniometry. Gait Posture 16:46–54
Nabeyama R, Matsuda S, Miura H, Kawano T, Nagamine R, Mawatari T, Tanaka K, Iwamoto Y (2003) Changes in antero-posterior stability following total knee arthroplasty. J Orthop Sci 8:526–531
Nozaki H, Banks SA, Suguro T, Hodge WA (2002) Observations of femoral rollback in cruciate-retaining knee arthroplasty. Clin Orthop 404:308–314
Pritchett JW (1996) Anterior cruciate-retaining total knee arthroplasty. J Arthroplasty 11:194–197
Pritchett JW (2004) Patient preferences in knee prostheses. J Bone Joint Surg Br 86B:979–982
Scott RD, Volatile TB (1986) Twelve years experience with posterior cruciate-retaining total knee arthroplasty. Clin Orthop 205:100–107
Shelburne KB, Pandy MG, Torry MR (2004) Comparison of shear forces and ligament loading in the healthy and ACL-deficient knee during gait. J Biomech 37:313–319
Stiehl JB, Komistek RD, Cloutier JM, Dennis DA (2000) The cruciate ligaments in total knee arthroplasty: a kinematic analysis of 2 total knee arthroplasties. J Arthroplasty 15:545–550
Suggs JF, Li G, Park SE, Steffensmeier S, Rubash HE, Freiberg AA (2004) Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study. J Arthroplasty 19:224–229
Tupling S, Pierrynowski M (1987) Use of Cardan angles to locate rigid bodies in three-dimensional space. Med Biol Eng Comput 25:527–532
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moro-oka, Ta., Muenchinger, M., Canciani, JP. et al. Comparing in vivo kinematics of anterior cruciate-retaining and posterior cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthr 15, 93–99 (2007). https://doi.org/10.1007/s00167-006-0134-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-006-0134-6