Abstract
Purpose
Localized full thickness defects of the femoral condyle can be highly symptomatic. Treatment options for these lesions are numerous in young patients, however they become increasingly challenging in middle aged and older patients. In order to delay traditional joint replacement procedures and to provide a soft tissue and bone sparing alternative, this study assess a focal inlay resurfacing procedure.
Methods
Between 2004 and 2008, a consecutive series of 27 patients were treated with the Arthrosurface HemiCAP® Focal Femoral Condyle Resurfacing Prosthesis and were assessed to study the clinical benefit of this procedure. Outcome measures included the KOOS, IKDC, HSS and WOMAC as well as physical and radiographic evaluation.
Results
Nineteen patients met the inclusion/exclusion criteria, 18 were available for review at a median follow-up of 34 months (range 20–57).The median age was 49 years (range 43–78). 63% had early arthritis, 5.2% localized osteonecrosis, and 31.6% had a focal traumatic full thickness defect. The follow-up total WOMAC score averaged 90.1 ± 9.3, The KOOS showed very good to excellent scores in all domains and also when compared to age-matched normative data. Significant improvement was seen with the HSS Score. On IKDC examination, 83.4% had normal or nearly normal results.
Conclusion
Focal femoral condyle resurfacing demonstrated excellent results for pain and function in middle-aged, well selected patients with full thickness cartilage and osteochondral defects. Patient profiling and assessment of confounding factors, in particular mechanical joint alignment; meniscal function; and healthy opposing cartilage surfaces, are important for an individual treatment approach and successful outcomes.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Single focal full thickness cartilage and osteochondral defects can be painful and disabling with a poor capacity to heal and usually progress to osteoarthritis if left untreated [9, 10, 18, 20],
For younger patients, many surgical options exist to stabilize defect margins and restore a weight bearing articular surface. With increasing age, cartilage repair becomes more complex and the outcome is less predictable [13]. Microfracture has been the mainstay of primary and repeat biological procedures. However, results have been less successful in older patients [13, 27, 30, 31, 35]. Revision of symptomatic lesions previously treated with bone marrow stimulation may show satisfactory fill rates, but often inferior biomechanical characteristics of the repair tissue.
Despite promising results in young patients, surgical treatment options, such as osteochondral grafting and chondrocyte implantation have had inconsistent results when used in older patients [10, 13, 15, 24, 35]. Unicompartmental or total knee arthroplasties increase the risk of revision surgery and associated morbidity when used in younger patients [11, 12, 17, 19, 25, 33].
To date, most available management techniques provide inconsistent results for the treatment of a full thickness, isolated articular cartilage defect in the knee joint of the middle-aged patient (40–60 years old) [13, 27]. This raised the challenge to develop a solution that would effectively manage pain, improve function and delay arthroplasty [1].
The purpose of this study was to evaluate the primary clinical results, indications and pit-falls of a novel metallic resurfacing prosthesis (HemiCAP® Focal Femoral Condyle Resurfacing Prosthesis, Arthrosurface Inc., Franklin, MA, USA) in middle-aged patients with a single focal femoral condyle defect. We hypothesized that focal resurfacing would effectively manage pain and function in the targeted population.
Materials and methods
Patients were selected in three participating centers. Between 2004 and 2008, twenty-seven patients presenting with isolated full thickness cartilage or osteochondral defects were treated with a contoured articular inlay prosthesis. All procedures were performed by the three senior co-authors (MB, BV and JB) at their respective institutions. Only isolated medial or lateral condylar defects were suitable for inclusion in this study. Exclusion criteria were BMI >35; kissing lesions; diameter >20 mm; inflammatory arthritis; ligamentous instability and a coronal malalignment of >7°. Based on these criteria, 8 patients were excluded: two had BMI >35 kg/m2; one had inadequate implant coverage; one had ACL instability; one had two full thickness defects in the femoral condyle; and three had large defects on their tibial plateau.
The 19 remaining patients signed an informed consent, completed a KOOS (which contains the WOMAC questions) questionnaire [5, 32, 34], and were subjected to an IKDC knee examination [23]. Demographics and past history were obtained. These nineteen patients matching the study selection criteria were treated with focal femoral condyle resurfacing. There were 18 females and 1 male, with a median age of 49 years (range 43–78). Sixty-three percent (12/19) were diagnosed with early arthritis, 5% (1/19) had osteonecrosis, and 32% (6/19) had localized traumatic full thickness defect. Sixty-three percent of patients received a 15 mm surface diameter prosthetic, 37% a 20 mm implant. Seventeen implants were in the medial femoral condyle, two in the lateral (Table 1). Three patients had a concomitant tibial osteotomy to address a mechanical axis deviation greater than 4°. One patient was lost to follow-up. Eighteen of these patients were available for review, with a median follow-up of 34 months (range 20–57).
Pre-operative preparation included clinical examination; standard radiographs of the knee; assessment of the mechanical weight bearing axis with full leg radiographs; and MRI or diagnostic arthroscopy. Based on defect size; location and grade; concomitant findings; surgical history; rehabilitation and recovery expectations an individual treatment was chosen.
In order to compare the pre-operative status of the patients to the post-operative status, a detailed chart review was performed and data was collected for the Hospital for Special Surgery Knee Score [22]. In order to better understand how our patients compared to patients with normal knees and to put results into better perspective, we compared the KOOS and WOMAC scores at follow-up to published data for normal populations.
Device description
The HemiCAP® resurfacing system is designed to match the shape and contour of the patient’s individual cartilage surface. It is a ‘patch’ for focal arthrosis and necrosis designed to provide a load sharing, contoured new surface while protecting the remaining, healthy cartilage margins.
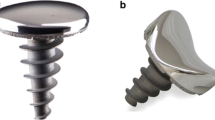
The prosthesis consists of two components: a fixation component and a modular articular component, connected with a morse taper. The fixation component is a titanium cancellous screw with full-length cannulation (Fig. 1). The cobalt chrome articular component is available in 15 or 20 mm diameter size and comes in 16 different offset configurations which correspond to the superior/inferior and medial/lateral radius of curvatures at the implant site (Fig. 2). Intra-operative mapping of the surface curvature and implantation of a matching articular component allows the surgeon to find a close fit to the patients’ original anatomy.
Operative technique
The procedure is initiated with a standard arthroscopy to ascertain proper indication and address any concomitant findings. Upon completion, using a small para-patellar incision over the center of the defect, the surgeon defines a working axis perpendicular and central to the articular cartilage surface with a drill guide. A guide pin is placed into the center of the defect and the fixation component is implanted into bone. Mapping instruments measure the surface curvature and a matching surface reamer prepares the inlay implant bed. Sizing trials confirm an accurate fit to the surrounding periphery. The articular component is aligned on the implant holder and is seated slightly recessed (minimum 1.0 mm) to the surrounding articular cartilage surface.
Standardized rehabilitation protocol focusing on range of motion is followed by strengthening exercises. Transition from one phase to the next is symptom based, however the primary implant stability allows for an accelerated recovery and rehabilitation plan. Patients are permitted to bear weight once post-operative pain and swelling have subsided.
Results
All follow-up KOOS and WOMAC subscales showed very good to excellent results. When compared to normative data for this population, all subscales showed results that were within reach of normative values [28, 32] (Figs. 3, 4).
KOOS sub-domain comparison HemiCAP® to normative* data. *KOOS normal scores from Paradowski et al. [32] (females age 35–54)
WOMAC total and sub-domains comparison to normative* data. *WOMAC normal scores from Lieberman [28] (mixed age 58–64)
For the overall IKDC knee examination, 83.4% (15/18) showed normal or nearly normal results (Table 2).
The post-operative HSS scores were significantly better (P > 0.001) when compared to pre-operative scores. The % change for the Knee Score was 42% while the % change for the function score was 48% (Table 3).
A second look arthroscopy was performed in a 48-year-old female who returned 8 months following high tibial osteotomy (HTO) and focal inlay resurfacing. The patient complained of prominent HTO hardware and requested to have it removed. It is important to note that only the HTO hardware was removed. Arthroscopy showed a well-fixed resurfacing implant with cartilage flow over the edges of the articular component and a stable cartilage border. The tibial plateau was graded as 1A and showed no signs of tibial response to the femoral resurfacing implant (Fig. 5). Follow-up radiographic examination at 2 years (Fig. 6) showed no signs of peri-prosthetic radiolucency; device disassembly; subsidence or cyst formation. No secondary signs of arthritis such as osteophytes or subchondral sclerosis had developed.
Discussion
The most important finding of this study was the clinical benefit demonstrated by this procedure. KOOS and WOMAC subscales showed very good to excellent levels at a follow-up of almost 3 years. Our results agree and confirm the conclusion drawn by Becher et al. [4] in their recent publication stating that the device was an effective treatment option for large lesions of the knee in middle-aged patients.
In synovial joints, articular cartilage and the subchondral bone are important units for load transmission. Osteochondral defects lead to an impairment of this load transmission in the affected part of the joint. If the lesion involves the weight-bearing surface, the incongruity may cause stress concentrations in adjacent regions. Large osteochondral defects are therefore considered to be a predisposing factor for the development of osteoarthritis [9, 20, 21].
Lesion progression is multifactorial. Defects characteristics such as size; depth; location; chronicity; and response to initial treatment are important in lesion progression. Patient factors such as age, level of activity; obesity, and genetic make-up also contribute. Finally, co-morbidities such as cruciate ligament deficiency, limb malalignment, and meniscal damage are all contributing factors into a lesion’s risk for progression to osteoarthritis [14, 15]. It is therefore desirable that these defects are treated effectively in order to prevent or slow progression to osteoarthritis.
When the patients’ charts were scrutinized and data collected that corresponded to the Hospital for Special Surgery Knee Score, the results showed significantly better post operative scores when compared to the pre-operative scores. These results combined with the comparison to normative data as demonstrated by the outcome scores on the KOOS and WOMAC across all domains that are equal or better after surgical intervention than those of normal subjects, show very strong support for this procedure.
Single focal full thickness cartilage and osteochondral defects are very common in the working population and can be painful, limiting daily activities and decreasing quality of life to the same extent as patients with severe arthritis [18]. Recently, numerous new techniques have been developed to provide hyaline or hyaline-like repair for articular defects. These include methods of resurfacing with biomaterials, periosteal or perichondral grafts. Cytokine or gene therapies, provide encouraging experimental data but unpredictable clinical results [16]. Clinical experience with autogenous and allogenous osteochondral grafting has shown that the transplanted hyaline cartilage had a good rate of survival [7, 13]. Despite this, osteochondral autografts are technically demanding, have associated donor site morbidity and work best in the younger patient (<40 years old). Allografts have the added risk of disease transmission and immune-mediated rejection [23]. Similarly, autologous chondrocyte implantation demonstrated good results [7, 13, 30, 36], but is a cost-prohibitive two-stage procedure with lengthy and difficult rehabilitation.
In active young patients, early arthroplasty increases the risk of revision surgery and associated morbidity since total joint replacement has a limited implant survivorship [12, 16, 19, 25, 33]. For older patients with a reduced level of activity a total knee prosthesis appears to be the most adequate solution especially in cases of advanced joint degeneration [12, 19, 25, 30].
The treatment of focal lesions in the 40–60 years age group with a solution that would effectively manage pain and improve function, but would be less aggressive than surgical solutions such as conventional arthroplasty has been achieved with the HemiCAP® Focal Femoral Condyle Resurfacing Prosthesis. The concept allows for an eventual arthroplasty should it be required without the likelihood of early revisions [1].
The effect of a metallic implant articulating with intact opposing tibial articular cartilage and meniscus up until now has remained largely unanswered. An experimental study assessing the functional and biological response to its use in a goat model resulted in good clinical outcomes [26]. After 1 year, no ongoing degenerative joint disease was apparent and the opposing tibial plateau cartilage surface was generally intact. The outcome was substantially better by comparison to other reported experimental animal studies in goats with untreated full thickness defects [8]. Becher et al. [2, 3] reported that the HemiCAP® does not lead to increased contact pressure with correct implant placement. In this study we had the opportunity for a second look at the implant (Fig. 5). We found neither indication of wear on the opposite articular surface nor any signs of progressive arthritis. This is very encouraging and provides some of the first answers to questions regarding focal resurfacing in the clinical application.
From our experience, patient selection is crucial. Seven of the eight exclusion patients already underwent revision surgery to a Total Knee Arthroplasty due to progressive cartilage disease. A fundamental issue is the fact that the articular component should be redressed approximately 1 mm under the articular surface to reduce the risk of developing a kissing lesion on the tibial plateau. As shown in Fig. 5, the cartilage surrounding the implant tends to grow over the edge of the implant. The prosthetic device seems to be incorporated anatomically in the femoral condyle.
We had excellent results in the treatment of three patients with both a focal full thickness cartilage defect and a malalignment of the lower limb. We believe in the combination of a corrective high tibial osteotomy with the implantation of a HemiCAP®, to improve joint congruency and establish proper mechanical alignment. HTO alone does not address the full thickness articular cartilage defect, therefore a combination procedure between resurfacing and mechanical realignment reduces the risk of overload and further progression of cartilage damage in the affected compartment.
Patient profiling and assessment of confounding factors, in particular mechanical joint alignment; meniscal function; and healthy opposing cartilage surfaces, remain critical patient selection criteria for successful outcomes. A treatment algorithm to assist surgeons in decision-making for this population of patients is proposed and presented (Fig. 7).
One limitation of this study was the relatively small number of study subjects. The population size did not allow further subgroup analysis of suspected confounding factors e.g. HTO (n = 3). Another limitation is the lack of baseline KOOS scores in this retrospective study. Pre-operative scores would have allowed a much stronger assessment of the data, however the study was initiated after the patients underwent treatment. It has been shown that recall data is only valid for a few weeks post surgery [6, 29], therefore patient level answers could not be provided at this time. The HSS knee score however, is based on components that can be reconstructed from a chart review.
The clinical relevance of this study is that the HemiCAP® resurfacing prosthesis offers an interim or alternative treatment strategy for the middle-age patient with a full thickness cartilage defect which preserves normal bone and cartilage allowing easier and better salvage procedures at a later time.
Conclusion
The results of our study show that resurfacing with a Focal Femoral Condyle Resurfacing Prosthesis demonstrates excellent results for pain and function in middle aged patients with full thickness cartilage and osteochondral defects meeting the inclusion criteria. The procedure adds to the existing range of focal cartilage procedures and successfully bridges biological treatment options to standard joint replacement allowing a continuation of localized management. The procedure further supports an individualized treatment approach throughout the management of knee arthrosis and arthritis. Soft tissues and bone stock are preserved providing a delayed exit strategy for traditional arthroplasty as a primary indication.
References
Archibeck MG, White RE (2003) What’s new in adult reconstructive knee surgery. J Bone Jt Surg Am 85(7):1404–1411
Becher C, Huber R, Thermann H, Paessler HH, von Skrbensy G (2008) Effects of a contoured articular prosthetic device on tibiofemoral peak contact pressure: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 16:56–63
Becher C, Huber R, Thermann H, Ezechieli L, Ostermeier S, Wellmann M, von Skrbensky G (2011) Effects of a surface matching articular resurfacing device on tibiofemoral contact pressure: results from continuous dynamic flexion–extension cycles. Arch Orthop Trauma Surg 131:413–419
Becher C, Kalbe C, Thermann H et al (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131:1135–1143
Bellamy N, Buchanan W, Goldsmith CH (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes following total hip and knee arthroplasty in osteoarthritis. Orthop Rheumatol 1:95–108
Bryant D, Norman G, Stratford P, Marx RG, Walter SD, Guyatt G (2006) Patients undergoing knee surgery provided accurate ratings of pre-operative quality of life and function 2 weeks after surgery. J Clin Epidemiol 59:984–993
Cole BJ, Lee SJ (2003) Complex knee reconstruction: articular cartilage treatment options. J Arthroscopy 19(Suppl 1):1–10
Custers RJH, Saris DBF, Dhert WJA et al (2009) Articular cartilage degeneration following the treatment of focal cartilage defects with ceramic metal implants and compared with microfracture. J Bone Jt Surg Am 91(4):900–910
Davis-Tuck ML, Wluka AE, Wang Y et al (2008) The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthr Cartil 16:337–342
de Windt TS, Bekkers JE, Creemers LB, Dhert WJ, Saris DB (2009) Patient profiling in cartilage regeneration: prognostic factors determining success of treatment for cartilage defects. Am J Sports Med 37(Suppl 1):58S–62S
Furnes O, Esehaug B, Lie SA et al (2007) Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Jt Surg Am 89(3):519–525
Gioe TJ, Novak C, Sinner P et al (2007) Knee arthroplasty in the young patient: Survival in a community registry. Clin Orthop Relat Res 464:83–87
Gomoll AH, Farr J, Gilloly SD et al (2010) Surgical management of articular cartilage defects of the knee. J Bone Jt Surg Am 92(14):2470–2490
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA (2004) Osteochondral defects in the human knee: influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med 32(6):1451–1458
Hangody L, Feczko P, Bartha L et al (2001) Mosaicplasty for the treatment of articular defects of the knee and ankle. Clin Orthop Relat Res 391(Suppl):S328–S336
Hangody L, Füles P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing-joints. J Bone Jt Surg Am 85(Suppl 2):25–30
Harrysson OL, Robertsson O, Nayfeh JF (2004) Higher cumulative revision rate of knee arthroplasties in younger patients with osteoarthritis. Clin Orthop Relat Res 421:162–168
Heir S, Nerhaus TK, Rotterud JH et al (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis. Am J Sports Med 38:231–237
Himanen A-K, Belt E (2005) Survival of the AGC total knee arthroplasty is similar for arthrosis and rheumatoid arthritis: finnish arthroplasty register report on 8, 467 operations. Acta Orthop 76:85–88
Hjelle K, Solheim E, Strand T et al (2002) Articular cartilage defects in 1000 knee arthroscopies. J Arthroscopy; 18:730–734
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress. A review of the current status and prospects. Osteoarthr Cartil 10:432–463
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Irrgang JJ, Anderson AF, Al Boland et al (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sport Med 29:600–613
Jakob RP, Franz T, Gautier E et al (2002) Autologous osteochondral grafting in the knee. Clin Orthop Relat Res 401:170–184
Julin J, Jamsen E (2010) Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis: a follow-up study of 32, 019 total knee replacements in the Finnish Arthroplasty Registry. Acta Orthop 81:413–419
Kirker-Head C, Van Sickle D, Ek SW, McCool JC (2006) Safety of and biological and functional response to a novel metallic implant for the management of focal full thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res 24(25):1095–1108
Kreuz PC, Erggelet C, Steinwachs MR et al (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? J Arthroscopy 22:1180–1186
Lieberman J, Hawker G, Wright JG (2001) Hip function in patients > 55 years old: population reference values. J Arthroplasty 16(7):901–904
Marsh J, Bryant D, MacDonald SJ (2009) Older patients can accurately recall their pre-operative health status six weeks following total hip arthroplasty. J Bone Jt Surg Am 91(12):2827–2937
Micheli LJ, Browne JE, Erggelet C et al (2001) Autologous chondrocyte implantation of the knee: multicenter experience and minimum 3-year follow-up. Clin J Sport Med 11:223–228
Mithoefer K, Williams RJ, Warren RF et al (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee. A prospective cohort study. J Bone Jt Surg Am 87(9):1911–1920
Paradowski PT, Bergman S, Sunden-Lumnius A et al (2006) Knee complaints vary with age and gender in the adult population: population-based reference based data for the knee injury and osteoarthritis outcome score (KOOS). BMC Musculoskelet Disord 7:38–45
Rand JA, Trousdale RT, Ilstrup DM et al (2003) Factors affecting the durability of primary total knee prostheses. J Bone Jt Surg Am 85(2):259–265
Roos EM, Roos HP, Ekdahl C, Lohmander LS (1998) Knee injury and osteoarthritis outcome score (KOOS)—validation of a Swedish version. Scand J Med Sci Sports 8:38–48
Steadman JR, Briggs KK, Rodrigo JJ et al (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year followup. J Arthroscopy 19:477–484
Zaslov K, Cole B, Brewster R et al (2009) A prospective study of autologous chondrocyte implantation in patients with failed prior treatment for articular cartilage defect of the knee. Results of the Study of the treatment of Articular Repair (STAR) clinical trial. Am J Sports Med 37:42–55
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bollars, P., Bosquet, M., Vandekerckhove, B. et al. Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20, 1753–1759 (2012). https://doi.org/10.1007/s00167-011-1757-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1757-9