Abstract
Purpose
The UniCAP® implant for femoral resurfacing treatment of large cartilage lesions and early OA was introduced in 2006. The outcome of the present study is from a prospective cohort study of 64 patients, followed 2 years clinically and 7 years for revisions.
Methods
From 2009 to 2013, 64 patients were treated with femoral resurfacing using the UniCAP implant. Indication for treatment with UniCAP implant was symptomatic huge cartilage lesion or early OA at the femoral condyle demonstrated by MRI or arthroscopy, which was ICRS grades 3–4 and more than 4 cm2. There were 28 males and 36 females with a median age of 51 (range 35–65) years. Patients were followed for 2 years clinically with Knee Society subjective outcome scores (KSS), pain scores and radiographic evaluations and for 7 years with complications and reoperations.
Results
At 2 years, the follow-up mean KSS improved from 49 (6.9) to 88 (17.1), the mean KSS function score improved from 46 (8.0) to 90 (17.1), and the mean Pain score improved from 7.4 (0.5) to 2.3 (1.4). 47 % of the implants were revised within 7 years to arthroplasty due to the progression of cartilage lesions, progressing of osteoarthritis or increased knee pain. The reoperation rate did not show any significant difference between females and males. The Kaplan–Meier survival rate was 50 % at 7 years, no difference among females and males.
Conclusion
The present study demonstrated an improved subjective outcome and reduced pain after femoral resurfacing using the UniCAP® implant in a relatively large cohort of patients with symptomatic large cartilage lesions or early OA. A 47 % reoperation rate with conversion to arthroplasty was found. The femoral resurfacing implantation can be a temporary treatment for large cartilage lesions or early OA that is expected to develop into osteoarthritis. For younger patients who are ineligible for arthroplasty treatment, this implant can offer a temporary solution.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treating localized, full-thickness femoral condyle cartilage defects or early osteoarthritis (OA) in middle-aged, active patients is a surgical challenge, because micro fracturing [15, 16, 23, 26] or biological treatment (cartilage- and chondrocyte transplantation) [9, 10, 17, 21, 24] does not relieve the symptoms sufficiently, and a total knee arthroplasty (TKA) or unicompartmental knee arthroplasty (UKA) is considered to be an exceptionally comprehensive type of surgery, since patients aged 35–55 years often have healthy cartilage in the remaining parts of the knee joint.
There is thus a treatment gap in managing these patients. An estimated 20 % of the patients with symptomatic knee OA in the US fall into this treatment gap [20]. An effective treatment would have a substantial positive social and economic impact [19].
Reducing and changing the functionality combined with intensified pain treatment has been the gold standard for treating these patients [20] until the point, where conventional TKA or UKA becomes the preferred option.
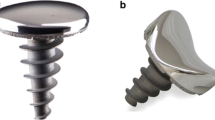
In 2006 an anatomic metallic implant for femoral resurfacing (UniCAP® Focal Femoral Condyle Resurfacing Prosthesis, Arthrosurface Inc., Franklin, MA, USA) was introduced for treatment of larger full-thickness femoral chondral lesions or early OA. Both femoral condyle and tibial implants have been designed (Fig. 1). After clinical tests in Europe and the USA [3, 6, 14, 25], together with multicenter studies with clinical and radiological evaluation [2, 4, 18], the device was introduced in Denmark in 2009.
UniCAP miniprosthesis. (Artrosurface Inc., Franklin, Massachusetts) Component: Cobalt–Chromium Alloy (Co–Cr–Mo) Undersurface Coating: Titanium (CP Ti) Fixation Stud: Titanium Alloy (Ti–6Al–4V). We did not use the Tibial part of this miniprostheses, but solely the femoral component for isolated cartilage lesions or beginning arthritis mainly on the femoral side and sizes bigger than addressable with the HemiCAP (20 mm diameter)
However, the evidence concerning the clinical outcome for this device has thus far been limited. Two case series with HemiCAP®, both with some 20 patients [2, 4] and one cohort study with 61 patients [18], all with varying osteochondral pathology, have demonstrated reduced pain and improved knee function, based on subjective outcome scores. There have yet to be any studies that have presented a clinical outcome with UniCAP® implants, and there is a need for more long-term clinical evidence in larger patient groups treated with condylar implants.
The aim of the present study was to present the clinical outcome in a prospective cohort of patients treated with the UniCAP® femoral part for full-thickness cartilage lesions or early OA on the femoral condyles. It was hypothesized that the implant would reduce pain and improve knee function after femoral resurfacing treatment.
Materials and methods
From 2009 to 2013, patients were treated with femoral resurfacing using the UniCAP® implant at a single centre. Indication for the treatment was symptomatic large cartilage lesion or early OA at the femoral condyles demonstrated by standing radiographs (KL grade), MRI or arthroscopy, with a ICRS grade 3–4 and size exceeding 400 mm2. Patients were not offered treatment if younger than 35 or older than 65, if they had a valgus or varus malalignment exceeding 5 degrees, ligament instability, more than 50 % meniscus removal or a BMI of more than 40. All of the patients were followed clinically for 2 years and up to 7 years with regard to revision.
Device description
The UniCAP® resurfacing implant consists of two components: fixation and modular articular components, the two connected by a morse taper. (UniCAP® Focal Femoral Condyle Resurfacing Prosthesis, Arthrosurface Inc, Franklin, MA, USA) The fixation component is a titanium cancellous screw with full-length cannulation. The cobalt chrome articular component is available in 20 × 35 mm diameter and comes in 16 different offset configurations corresponding to the superior/inferior and medial/lateral radius of curvatures at the implant site (Fig. 1). A polyethylene 20 mm inlay is available for the tibial lesion.
Surgical Procedure
The procedure was initiated with a standard arthroscopy to identify cartilage status and indication and treat any concomitant intra-articular pathology. The defect was exposed using a small para-patellar incision, and the cartilage lesion was sized. A special centralized drill guide was used to place a k-wire perpendicular and central to the articular cartilage surface. The reaming for the fixation screw was performed over the k-wire, and the fixation screw was implanted into bone. Mapping instruments measured the surface curvature, and matching surface reamers prepared the inlay implant bed. Sizing trials were used to confirm an accurate fit to the surrounding cartilage. The resurfacing implant was fixed press-fit onto the fixation screw and seated flush or slightly recessed 0.5 mm to the surrounding articular cartilage surface. A standardized rehabilitation protocol with free range of motion was allowed immediately after the operation. For the first 2 weeks, patients were touch weight-bearing walking, followed by full weight-bearing when walking (Fig. 2).
Outcome evaluation
Patients were assessed after 3 months, 1 and 2 years by radiological status, Knee Society Scores (KSS) objective and function subscales and pain score using numerical rank scale (0–10), 10 being the worst possible pain. For the KSS function score, we defined a response rate of good outcome as having an increase in 20 points or greater in the KSS function from the preoperative to follow-up time.
Information concerning complications and reoperations was obtained from the National Joint Replacement Register (DKR) [7]. Analgesic consumption preoperatively and at follow-up time-points was assessed to document improvements in pain level.
Radiographic evaluation
Osteoarthritis (OA) grade was evaluated using the Kellgren–Lawrence grade (KL) [13] for both medial and lateral tibiofemoral compartment preoperatively and at 2-year follow-up to investigate OA development after surgery [18].
The study was approved by the regional ethical committee of Region South Jutland # 13/6614-57093/13.
Statistical analysis
Demographics and baseline characteristics were presented as mean value and standard deviations. Chi-square and Student’s t test were used for the comparison of proportional and paired data. The Kaplan–Meier survival analysis was used with revision or death as the endpoint and 95 % confidence interval (CI). For the statistical analysis, Stata 13 was used. P values less than 0.05 were considered statistically significant.
Results
There were 28 males and 36 females, mean age 51 (35–65) years. The demographic characteristics of the total patient population are shown in Table 1. Clinical and radiographic evaluation at 12-week, 1- and 2-year follow-up was completed by 100, 78 and 53 % of the patients, respectively. The reason for lost to follow-up at 1 and 2 years was patients not being reached at evaluation time or having had a revision performed. The evaluation of the failure endpoint revision to arthroplasty was completed by all of the patients, since the national registry for knee arthroplasty—DKR [7] in Denmark ensures the tracking of all arthroplasty procedures.
Objective and subjective outcomes
The fractions of patients with different degrees of KL grading as well as the fraction of patients changed to a more severe OA grade, both in revised and unrevised patients, are presented in Table 2. Objective outcomes based on KSS knee score improved significantly. KSS improved for the implants from 49 (6.9) to 88 (17.1) after 2 years p < 0.01. The subjective KSS function and pain scores also improved significantly.
The proportion of patients with a clinically relevant improvement in function score of >20 point was 95 % at 1-year and 92 % at the 2-year follow-up. There was no tendency to any difference in this response rate between patients.
Analgesic consumption
Preoperatively, all of the patients used some type of oral analgesic medicine (Paracetamol, NSAID and/or morphine). At 2-year follow-up, analgesic consumption was reduced and VAS was reduced significantly from 7.4 (0.5) preoperatively to 2.3 (1.2) at 2-year follow-up.
Radiographic osteoarthritis evaluation
Preoperative—KL OA grade was 1.9 (0.5) in the medial and 1.2 (0.4) in the lateral compartment. At 2-year follow-up, KL OA grade was 2.4 (0.5) in the medial and 1.7 (0.6) in the lateral compartment—for both compartments a significant worsening. At revision time, the patient’s KL grade was significantly worse compared to unrevised at 2-year follow-up—(3.1 (0.8) in medial and 2.4 (0.6) in lateral), indicating a rapid progression of OA. When comparing the KL grade at revision with unrevised patients’ latest KL grade, a significant progression in the revised patients compared to the unrevised patients was found.
Failures and complications
Thirty (47 %) implants were revised to arthroplasty due to progression of cartilage lesions over the 7-year follow-up period (Fig. 3). In most cases, peri-implant unicompartmental cartilage wear or multicompartmental OA progression was seen (Fig. 4), and the KL grade was significantly worsened compared to patients at 2-year follow-up. In two cases, implant screw loosening was observed. No difference between females and males was found for reoperation rates.
Discussion
The most important finding of the present study was that condylar resurfacing treatment with the UniCAP implant demonstrated clinically relevant improvements in both function and pain reduction within the first 24 months of follow-up in patients with unicompartmental localized traumatic or degenerative cartilage lesions (early OA), but with a mean time to revision at 50 months. We found a 7-year survival rate at 50 % for this cohort of “middle-aged” patients suffering from knee pain and disability to an extent that is comparable to other patients with severe knee arthritis [11].
The present study is the largest case series with UniCAP femoral resurfacing treatment presented until now.
The clinical results are consistent with the few previously published studies concerning condylar resurfacing treatment. Bollars et al. [4] found a significant improvement, the subjective score reaching a level equal to a matched normal population in 27 patients treated with the HemiCAP implant. Becher et al. [2] and Laursen et al. [18] demonstrated similar significant improvements in the subjective outcome in 21 and 61 patients, respectively.
There are not presently any published clinical studies concerning the UniCAP, but an introductory paper exists presenting the UniCAP as an alternative for unicompartmental arthritis (early OA) [22].
It has been reported that chondral or osteochondral lesions of the knee are found in up to 60 % of the patients undergoing knee arthroscopy [5] and most of these are located at the medial femoral condyle with a mean size around 2 cm [12]. Smaller lesions may have a capacity to heal, but seldom lesions more than 10 mm [8]. Untreated symptomatic lesions may progress with articular degeneration and upcoming OA [6], and debilitate the patients with progressing impairment and increasing pain [11, 18]. The loss of working ability may be fatal to the patients still at work, and the economic costs for society enormous, especially for these patients aged 35–55 in the mentioned “Treatment Gap”. In the USA 3.6 million patients (20 %) with symptomatic knee pain fall into this group [5].
The first metallic inlay resurfacing device—the HemiCAP (Arthrosurface Inc., Franklin, MA, USA)—was introduced for this purpose to address these full-thickness cartilage defects (introduced in the USA in 2003, in Denmark in 2007. There have yet to be any long-term studies; only register studies from the Australian Joint Replacement Registry, 2013 [1] with 5-year revision rates at 30 % in 176 patients, but it is unknown, if it is only HemiCAP or a mixture of HemiCAP/UniCAP. The reason for revision was progressing OA 59 %, loosening 15 % and pain 7 %. The same rates are shown in the Danish Knee Registry (DKR), 2013 [7] with a 6-year survival rate in 230 caps of 45 %, but again this is a mixture of HemiCAP/UniCAP, and not all caps in Denmark are registered in DKR, as we know, that around 430 Hemi- and UniCAPs were implanted (data from the Distributor in DK).
There is follow-up of all of the resurfacing devices (both HemiCAP [18] and UniCAP, 61 and 64 respectively). This paper focuses on the UniCAP, knowing it is two very different devices, and the indication for the UniCAP is large chondral lesions on the femoral condyles or early OA in one chamber, with the possibility to address minor lesions on the tibial side.
A 50 % 7-year survival rate would be far too high compared to TKA or UKA, with 10-year survival rates of 95 and 80 % respectively, as shown in the Danish Knee Registry [7], but cartilage procedures and UKA/TKA cannot be compared, as the indications regarding patient age, workload and functionality are different. The inclusion and exclusion criteria must be followed very thoroughly and might be sharpened, at least in respect to age (not younger than 40 or older than 65) and only with one small (<20 mm in diameter) cartilage lesion (Grades 3–4) on the femoral condyles. We think a more elongated lesion (20 × 30 mm or more) is more likely to be a progressing chondral disease (early OA) and therefore promotes too early failure. A most concerning 47 % revision rate up to 7 years with conversion to UKA or TKA was found, but the finding of clinically relevant improvement in function and pain reduction suggests that femoral resurfacing implantation can be a temporary treatment for cartilage lesions expected to develop into early OA, but it is recommended, not to address large cartilage lesions or progressing OA with this resurfacing prosthesis.
The advantage of the present study is that it is the first published larger cohort of patients all followed clinically up to 2 years, and arthroplasty reoperation follow-up at 7 years was complete due to national registry data. The study is limited by investigating only short- to mid-term clinical results, and as it is a single-centre case study with only one operating surgeon, the external validity can be weakened.
Conclusion
The present study demonstrated improved subjective outcome and reduced pain after femoral resurfacing using the UniCAP implant in a cohort of 64 patients with large cartilage lesions or early OA in the knee. A 47 % revision rate of up to 7 years was found. Femoral resurfacing implantation can be a temporary treatment for cartilage lesions expected to develop into early OA, but it is recommended, not to address large cartilage lesions or progressing OA with this resurfacing prosthesis.
References
Australian Orthopaedic Association National Joint Replacement Registry (2013) Annual report, pp 108–109
Becher C, Huber R, Thermann H, Ezechieli L, Ostermeier S, Wellmann M, von Skrbensky G (2011) Effects of a surface matching articular resurfacing device on tibiofemoral contact pressure: results from continuous dynamic flexion-extension cycles. Arch Orthop Trauma Surg 131:413–419
Becher C, Kalbe C, Thermann H, Paessler HH, Laprell H, Kaiser T, Fechner A, Bartsch S, Windhagen H, Ostermeier S (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131:1135–1143
Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J (2012) Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:1753–1759
Brennan SA, Devitt BM, O’Neill CJ, Nicholson P (2013) Focal femoral condyle resurfacing. Bone Joint J 95-B:301–304
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association with cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum 52:2033–2039
Danish Orthopaedic Association (DOS) (2013) National Joint Replacement Registry (DKR) Annual report
Guettler JH, Demetropoulos CK, Yang KH, Jurist KA (2004) Osteochondral defects in the human knee:influence of defect size on cartilage rim stress and load redistribution to surrounding cartilage. Am J Sports Med 32(6):1451–1458
Görtz S, Bugbee WD (2006) Allografts in articular cartilage repair. J Bone Joint Surg Am 88(6):1374–1384
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85A(Suppl 2):25–32
Heir S, Nerhus TK, Rotterud JH, Loken S, Ekeland A, Engebretsen L, Aroen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38:231–237
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1.000 knee arthroscopies. Arthroscopy 18(7):730–734
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kirker-Head CA, Van Sickle DC, Ek SW, McCool JC (2006) Safety of, and biological and functional response to, a novel metallic implant for the management of focal full-thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res 24:1095–1108
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P, Ghanem N, Uhl M, Sudkamp N (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22:1180–1186
Kreuz PC, Steinwachs MR, Erggelet C, Krause SJ, Konrad G, Uhl M, Südkamp N (2006) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthritis Cartilage 14(11):1119–1125
Laprell H, Petersen W (2001) Autologous osteochondral transplantation using the diamond bone-cutting system (DBCS): 6-12 years’ follow-up of 35 patients with osteochondral defects at the knee joint. Arch Orthop Trauma Surg 121(5):248–253
Laursen JO, Lind M (2015) Treatment of full-thickness femoral cartilage lesions using condyle resurfacing prosthesis. Knee Surg Sports Traumatol Arthrosc. doi:1007/s00167-05-3726-1
Li CS, Karlsson J, Winemaker M, Sancheti P, Bhandari M (2014) Orthopedic surgeons feel that there is a treatment gap in management of early OA: international survey. Knee Surg Sports Traumatol Arthrosc 22(2):363–378
London NJ, Miller LE, Block JE (2011) Clinical and economic consequences of the treatment gap in knee osteoarthritis management. Med Hypotheses 76:887–892
Micheli LJ, Browne JE, Erggelet CF, Fu F, Mandelbaum B, Moseley JB, Zurakowski D (2001) Autologous chondrocyte implantation of the knee: multicenter experience and minimum 3-year follow-up. Clin J Sports Med 11(4):223–228
Miniaci A (2014) UniCAP as an alternative for unicompartmental arthritis. Clin Sports Med 33(1):57–65
Mithoefer K, Williams RJ 3rd, Warren RF, Potter HG, Spock CR, Jones EC (2005) The microfracture technique for the treatment of articular cartilage lesions in the knee: a prospective cohort study. JBJS Am 87(9):1911–1920
Morelli M, Nagamori J, Miniaci A (2002) Management of chondral injuries of the knee by osteochondral autogenous transfer (mosaicplasty). J Knee Surg 15:185–190
Skrbensky G, Becher C, Schmidt M (2008) Resurfacing for sportive patients: HemiCAP results and biomechanic in vitro tests. In: SICOT/SIROT 2008 XXIV triennial world congress, 24–28 August 2008, Hong Kong
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: 11-year follow-up. J Arthroscopy 19:477–480
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Laursen, J.O. Treatment of full-thickness cartilage lesions and early OA using large condyle resurfacing prosthesis: UniCAP® . Knee Surg Sports Traumatol Arthrosc 24, 1695–1701 (2016). https://doi.org/10.1007/s00167-016-4000-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4000-x