Abstract
Purpose
The menisci are known to be important secondary constraints to anterior translation of the tibia in the ACL-deficient knee. The effect of meniscal loss on knee stability as measured by the magnitude of the pivot shift following ACL reconstruction is unknown. The objective of this investigation was to determine the effect of meniscectomy on knee stability following two single-bundle ACL reconstruction strategies.
Materials and Methods
A mechanized pivot shift was performed on cadaveric specimens in the ACL-intact and ACL-deficient state. Tibiofemoral translation was recorded using a surgical navigation system. The ACL was reconstructed utilizing a nonanatomic graft (n = 10) extending from the posterolateral tibial footprint to the anteromedial femoral footprint, or an anatomic anteromedial single-bundle graft extending from the anteromedial tibial footprint to the anteromedial femoral footprint (n = 10) and testing repeated. The medial or lateral meniscus was sectioned and the examination repeated. The other meniscus was sectioned and the examination subsequently repeated.
Results
Lateral compartment translation during the pivot shift was significantly reduced following anatomic ACL reconstruction. In the nonanatomic group, lateral compartment translation increased by 9.1 mm (P < 0.001) after unicomparmental meniscectomy and 11.5 mm (P < 0.001) after bicompartmental meniscectomy. In the anatomic reconstruction group, lateral compartment translation increased by 7.6 mm (P < 0.001) after bicompartmental meniscectomy.
Conclusion
With isolated ACL injury, anatomic single-bundle ACL reconstruction controlled the pivot shift during time zero testing. However, significant increases in lateral compartment translation during the pivot shift are seen following bicompartmental meniscectomy. Nonanatomic ACL reconstruction was less effective in controlling the pivot shift at time zero testing, and significant increases in lateral compartment translation during the pivot shift were seen following both unicomparmental and bicompartmental meniscectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meniscal injury following ACL reconstruction is a common clinical scenario [17]. In a recent epidemiologic study by Lyman et al., meniscectomy was cited as one of the most common surgical procedures performed in the first year following ACL reconstruction [18]. It is widely accepted that the medial meniscus, and to a lesser degree the lateral meniscus, plays an important role as secondary restraints to anterior tibial translation in the ACL-deficient knee [1, 8, 15, 16]. Accordingly, meniscal preservation has the theoretical advantage of limiting anterior translation following ACL reconstruction. However, the effect of subsequent meniscal loss on knee stability and rotational kinematics following ACL reconstruction is not well described.
In a cadaveric study, Papageorgiou et al. [22] demonstrated that medial meniscectomy following single-bundle ACL reconstruction resulted in a significant increase in in situ graft forces; however, anterior tibial translation was unaffected. Conversely, Seon et al. [24] found that single-bundle ACL reconstruction following subtotal medial meniscectomy significantly reduced anterior tibial translation at all flexion angles in the meniscus-deficient knee. However, this reconstruction strategy did not restore knee kinematics to the intact state. In a more recent investigation, Bedi et al. [3] demonstrated that, in a knee with significant meniscal injury resulting in a high-grade pivot shift, double-bundle ACL reconstruction may better restore knee kinematics.
The aforementioned studies have yielded conflicting conclusions regarding the effect of meniscectomy on stability of the ACL-reconstructed knee. Moreover, there is a paucity of data in the current literature on the effect of meniscal loss on dynamic measures of knee stability such as the pivot shift. The pivot shift involves a pathologic, multiplanar motion path elicited by a combined axial and valgus load applied to the knee as it is brought from extension into flexion [2]. The presence of a pivot shift in the setting of ACL-insufficiency has been correlated with subjective instability, failure to return to previous level of play, poor outcome scores, and future arthrosis of the knee [12]. We have developed a mechanized pivot shift device to standardize this complex examination maneuver and have previously reported on the reproducibility of this technique in measuring translation of the medial, central, and lateral compartments of the knee during the pivot shift examination [6, 21].
To our knowledge, there is no data on the effects of meniscectomy on the pivot shift examination following single-bundle ACL reconstruction. The purpose of this investigation was to determine the effects of lateral and medial meniscectomy on knee stability following single-bundle ACL reconstruction as measured by the kinematics of a navigated Lachman and pivot shift examination. We hypothesized that a single bundle placed in an “anatomic” position (a graft that courses from the anteromedial footprint of the tibia to the anteromedial footprint of the femur) would better control the Lachman and the pivot shift tests than a “nonanatomic” or “mismatch” graft (a graft that courses from the posterolateral footprint of the tibial to the anteromedial footprint of the femur) in this mensical loss model.
Materials and methods
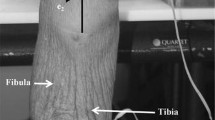
Five fresh frozen cadaveric hip-to-toe lower extremity specimens (10 knees) were utilized for this study (mean age 62 years, range 57–70). Specimens were thawed for 48 h at room temperature prior to testing, to ensure full mobility of the hip and knee joints. Specimens were stored in a cold room overnight, and the contralateral extremity was tested the following day. During the testing procedure, room temperature was consistently kept at 22°C. Specimens were placed supine on an operating room table, allowing for a free unrestricted range of motion at the hip and knee. Physical examination was carried out, a medial parapatellar arthrotomy of the knee was performed, and specimens were examined for alignment, deformities, ligamentous integrity, as well as the for absence of significant meniscal and articular cartilage lesions. Only specimens without major deformities; without previous meniscus surgery; and without gross osteoarthritis, were tested in this study.
The PraximSurgetics surgical navigation system (PraximMedivision, Grenoble, France) with dedicated ACL software was used for kinematic data acquisition. Rigid bodies were fixed to Steinman pins that were drilled in the distal femur and proximal tibia. A rigid array was fixed to Steinman pins in the distal femur and proximal tibia, and reflective markers were traced by an infrared camera as previously described [5, 7]. Surface landmarks were recorded, intraarticular surface geometry was mapped, and a three-dimensional (3D) model of the knee was created [25]. The knee was cycled from full extension to 90° of flexion with a proximally directed axial force to keep the tibial and femoral condyles in contact, at all flexion positions. This represented the passive reference path from which the deviation was measured during each pivot shift examination. The accuracy of this system has been demonstrated to be 1 mm/1 degree [10, 11].
Instrumented laxity testing consisted of a Lachman test and pivot shift test. A 68-N Lachman test was performed with a tensiometer attached to a 6.5-mm screw in the anterior tibia. Optical tracking of joint position allowed for consistent testing at 30° of knee flexion. Anterior knee translation was recorded by the navigation system during the instrumented Lachman examination. This testing protocol has been shown to demonstrate repeatability when compared with a robotic manipulator [23].
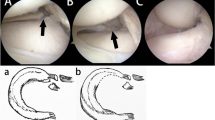
A standardized mechanized pivot shift maneuver was performed as previously described [6, 21] (Fig. 1). During the mechanized pivot shift, the navigation system recorded the 3D motion path of a tracked point at the center of the tibia, center of the medial tibial plateau, and center of the lateral tibial plateau. Motion of these points was analyzed throughout a given motion path with respect to a tracked central point in the notch of the femur. ACL-specific software allowed for the comparison of the motion path during the pivot shift with the reference motion path of flexion–extension [7, 14]. The navigation software is a dedicated ACL program that allows for navigated guidance of tunnel positioning as well as for the tracking and quantification of knee kinematics during a stability examination. In the medial and lateral compartments, maximum tibial translation during the pivot shift maneuver was reported as the difference between reference motion path and pivot shift motion path. The primary advantage of this navigation system is the ability to analyze kinematics during a dynamic stability test rather than a “simulated pivot shift”. The utilization of a surgical navigation system during clinical laxity examinations has been shown to be reliable and repeatable. The high intraclass correlation coefficients were recorded for the surgical navigation system in comparison with a robotic manipulator (ICC 0.998) [23].
For each cadaver specimen, one knee was randomly assigned to either medial or lateral unicompartmental meniscectomy, followed by bicompartmental meniscectomy. The testing protocol consisted of instrumented Lachman and mechanized pivot shift evaluation in the (1) intact state, (2) after complete ACL transection, (3) after ACL reconstruction, (4) after ACL reconstruction and unicompartmental meniscectomy, and (5) subsequent bicompartmental meniscectomy. The testing protocol is demonstrated in Fig. 2.
The ACL was transected by carefully dissecting the synovial sheath from the ACL at 90° of flexion and dissecting the tissue between the ACL and PCL. The femoral insertion of the ACL was dissected off of the femoral wall using a number 15 blade with the knee at 120° flexion. The stump was then retracted anteriorly, and the tibial insertion was resected off of the tibia.
Hamstring grafts were utilized for single-bundle ACL reconstruction. A quadrupled gracilis-semitendinosus tendon (diameter 7–8 mm) was used for all of the single-bundle reconstructions. The tunnel positions in this study were anatomically based and not according to conventional surgical tunnel placement reference systems (o’clock positions). For the NA-ACLR reconstruction (nonanatomic), a size appropriate tunnel was drilled in the center of the posterolateral ACL footprint of the tibia using an ACL tibial aiming device (Arthrex, Naples, FL). A femoral tunnel was drilled in the center of the anteromedial femoral ACL footprint by flexing the knee and drilling through the open arthrotomy. For the AM-ACLR reconstruction (anatomic), a size appropriate tunnel was drilled in the center of the anteromedial ACL footprint of the tibia using the ACL tibial aiming device. A femoral tunnel was drilled in the center of the anteromedial femoral ACL footprint.
The grafts were passed in standard fashion. On the femoral side, a continuous loop Endobutton (Endobutton CL, Smith and Nephew, Andover, Massachusetts) was used to achieve fixation. Prior to final fixation of the grafts on the tibia, the knee was cycled ten times with tension on the graft to account for stress relaxation in the graft-fixation complex [13]. The graft was fixed on the tibial side at 20° of knee flexion. Axial tension of 44 N on the draw sutures was applied to each graft, and the sutures were secured over a screw post [19, 26].
For the medial meniscectomy, a total medial meniscectomy was performed with a curved meniscectomy blade through the previous arthrotomy. Deep knee flexion and mild valgus were applied. The deep medial collateral ligament (MCL) was left intact. In the lateral meniscectomy group, a complete lateral meniscectomy was performed through the arthrotomy. This was performed by cutting and elevating the anterior horn of the lateral meniscus with a No. 15 scalpel. The anterior horn was clamped with a Kocher clamp, and the body of the meniscus was resected at the meniscocapsular junction under axial tension on the Kocher clamp and with the knee at 90° of flexion and mild varus stress. With the knee in full flexion, the lateral meniscus was dislocated into the notch and the posterior horn was resected. The popliteus tendon was left intact. Extreme care was taken to avoid violation of the joint capsule on the medial or lateral compartment during meniscectomy and to protect the ACL reconstruction. The knee underwent navigated Lachman and pivot shift examination, followed by meniscectomy of the opposite compartment.
Instrumented testing was carried out for each of the four conditions: (1) NA-ACLR/unicompartmental meniscectomy, (2) NA-ACLR/bicompartmental meniscectomy, (3) AM-ACLR/unicompartmental meniscectomy, and (4) AM-ACLR/bicompartmental meniscectomy.
Statistical analysis
Repeated measures analysis of variance with a post hoc Tukey multiple comparison test was used to compare the translations in the Lachman examination and for each tracked point during the pivot shift examination within each group. Based on historical data, we estimated a priori that 10 knees would be required to detect a 3 mm increase in tibiofemoral translation across conditions in the Lachman examination and in the pivot shift with 0.80 power at the 95% confidence level. All statistical analysis was performed using GraphPad Prism (GraphPad Software, San Diego, California). Significance was set at α = 0.05.
Results
Lachman examination
Transection of the ACL resulted in a significant increase in anterior translation of the tibia during Lachman examination as compared with the intact state (6.3 ± 2.5 mm vs. 3.3 ± 1.9 mm, P < 0.05 for ACL-deficient vs. ACL intact).
Following nonanatomic ACL reconstruction, anterior tibial translation during Lachman testing was reduced to the near intact state (4.2 ± 2.9 mm vs. 3.3 ± 1.9 mm, (n.s.) for nonanatomic vs. ACL-intact). Unicompartmental meniscectomy following nonanatomic ACL reconstruction resulted in a significant anterior translation of 2.7 mm (6 ± 3.0 mm vs. 3.3 ± 1.9 mm, P < 0.05 for nonanatomic + unicompartmental meniscectomy vs. ACL-intact), while bicompartmental meniscectomy also resulted in a significant 4.7 mm increase in mean anterior translation (8 ± 2.9 mm vs. 3.3 ± 1.9 mm, P < 0.05 for NA-ACLR + bicompartmental meniscectomy vs. ACL-intact). Results are depicted in Fig. 3a.
Effect of meniscectomy following nonanatomic (NA-ACLR) and anteromedial (ACLR) reconstruction on a 68 N Lachman examination. Note the increase in anterior translation following uni- and bicompartmental meniscectomy in the NA-ACLR group (a) (P < 0.05). No increase in anterior translation was noted after uni- or bicompartmental meniscectomy in the AM-ACLR group (b)
Similarly, anatomic ACL reconstruction reduced anterior tibial translation to the intact state (3.3 ± 2.3 mm vs. 3.3 ± 1.9 mm, (n.s.) for anatomic vs. ACL-intact). Neither unicompartmental nor bicompartmental meniscectomy resulted in an increase in anterior tibial translation following anatomic ACL reconstruction (3.2 ± 2.6 mm vs. 3.3 ± 1.9 mm, (n.s.) for anatomic + unicompartmental meniscectomy vs. ACL-intact; 3.3 ± 2.1 mm vs. 3.3 ± 1.9 mm, (n.s.) for anatomic + bicompartmental meniscectomy vs. ACL-intact). Results are depicted in Fig. 3b.
Pivot shift
Lateral compartment translation
Transection of the ACL resulted in a significant increase in anterior lateral compartment translation during the mechanized pivot shift examination as compared with the intact state (9.8 ± 2.5 mm vs. 0.7 ± 1.9 mm, P < 0.05 for ACL-deficient vs. ACL-intact).
Lateral compartment translation during the mechanized pivot shift examination was not well controlled by nonanatomic ACL reconstruction (8.5 ± 5.6 mm vs. 0.7 ± 5.8 mm, P < 0.05 for nonanatomic vs. ACL intact). Both unicompartmental and bicompartmental meniscectomy resulted in a significant increase in lateral compartment translation as compared with the intact state. (9.8 ± 6.2 mm vs. 0.7 ± 1.9 mm, P < 0.05 for nonanatomic + unicompartmental meniscectomy vs. ACL-intact; 12.2 ± 4.4 mm vs. 0.7 ± 1.9 mm, P < 0.05 for nonanatomic + bicompartmental meniscectomy vs. ACL-intact). Results are depicted in Fig. 4a.
Effect of meniscectomy following nonanatomic (NA-ACLR) and anteromedial (ACLR) reconstruction on lateral compartment translation during the mechanized pivot shift. Note that nonanatomic ACL reconstruction was ineffective at controlling lateral compartment translation, and subsequent meniscectomy resulted in further increases in lateral compartment translation. Conversely, anteromedial ACL reconstruction restored lateral compartment translations to the intact state. Bicompartmental meniscectomy resulted in a significant increase lateral compartment translation as compared with the intact state (P < 0.05)
Conversely, anatomic ACL reconstruction reduced anterior lateral compartment translation to the near intact state (3.1 ± 5.6 mm vs. 0.7 ± 5.8 mm, (n.s.) for anatomic vs. ACL-intact). While unicompartmental meniscectomy did not have a significant effect on lateral compartment translation following anatomic anteromedial ACL reconstruction (4.5 ± 6.6 mm vs. 0.7 ± 5.8 mm, (n.s.) for anatomic + unicompartmental meniscectomy vs. ACL-intact), bicompartmental meniscectomy significantly increased lateral compartment translation (8.3 ± 3.3 mm vs. 0.7 ± 58 mm, P < 0.05 for anatomic + bicompartmental meniscectomy vs. ACL-intact). Results are depicted in Fig. 4b.
Medial compartment translation
Transection of the ACL resulted had no effect on medial compartment translation during the mechanized pivot shift examination as compared with the intact state (−1.5 ± 7.0 mm vs. −3.2 ± 6.1 mm, (n.s.) for ACL deficient vs. ACL-intact).
Medial compartment translation during the mechanized pivot shift examination was not affected by nonanatomic ACL reconstruction (−1.3 ± 6.4 mm vs. −3.2 ± 6.1 mm, (n.s.) for nonanatomic vs. ACL-intact). Subsequent unicompartmental and bicompartmental meniscectomy had no effect on medial compartment translation as compared with the intact state (−1.6 ± 6.7 mm vs. −3.2 ± 6.1 mm, (n.s.) for nonanatomic + unicompartmental meniscectomy vs. ACL-intact; −1.2 ± 9.6 mm vs. −3.2 ± 6.1 mm, (n.s.) for nonanatomic + bicompartmental meniscectomy vs. ACL-intact).
Similarly, anteromedial ACL reconstruction had no effect on medial compartment translation during the pivot shift (−2.1 ± 6.5 mm vs. −3.2 ± 6.1 mm, (n.s.) for anatomic vs. ACL-intact). Subsequent unicompartmental and bicompartmental meniscectomy had no effect on medial compartment translation as compared with the intact state. (−4.1 ± 4.7 mm vs. −3.2 ± 6.1 mm, (n.s.) for anatomic + unicompartmental meniscectomy vs. ACL-intact; −3.4 ± 5.0 mm vs. −3.2 ± 6.1 mm, (n.s.) for anatomic + bicompartmental meniscectomy vs. ACL-intact).
Discussion
The most important finding of the present study was that following nonanatomic or “mismatch” ACL reconstruction, unicompartmental meniscectomy resulted in a significant increase in anterior laxity during the Lachman examination that was amplified by subsequent bicompartmental meniscectomy. Conversely, anatomic anteromedial ACL reconstruction was effective at controlling abnormal anterior tibial translation following both unicompartmental and bicompartmental meniscectomy.
Moreover, anatomic anteromedial ACL reconstruction was effective in controlling the pivot shift maneuver in the isolated ACL injury as well as after ACL injury and unicompartmental meniscal loss. However, following subsequent bicompartmental meniscectomy, a significant increase in lateral compartment translation was noted during the pivot shift after an anatomic ACL reconstruction. Nonanatomic ACL reconstruction was less effective at controlling lateral compartment translation during the pivot shift, and further increases in translation were noted following both unicompartmental and bicompartmental meniscectomy. Collectively, these findings suggest that anatomic ACL reconstruction is able to control the Lachman test even after bicompartmental meniscal excision. However, while an anatomic ACL reconstruction may control the pivot shift in an isolated ACL injury and after unicompartmental meniscal loss, profound meniscal deficiency may render the knee less stable during pivoting events. Conversely, nonanatomic ACL reconstruction appears to be sensitive to meniscus status even during the Lachman examination. While nonanatomic ACL reconstruction may control the Lachman in an isolated ACL injury, subsequent meniscus loss may result in aberrant Lachman examinations. Additionally, nonanatomic ACL reconstruction exhibited poor control of the pivot even in a meniscal competent knee. Meniscal loss after nonanatomic ACL reconstruction rendered the knee progressively more unstable during the pivoting maneuver.
The results of this laboratory investigation may have important implications. Lyman et al. showed that the frequency of subsequent surgery on either knee within 1 year of ACL reconstruction was 6.5 with 25% of this patient cohort undergoing meniscectomy [18]. Accordingly, meniscal loss following ACL reconstruction represents a common clinical entity that has not been fully described in the current biomechanical literature.
Multiple authors have reported on the relevance of the menisci in anterior–posterior (AP) knee stability in the ACL-intact and ACL-deficient knee [1, 8, 15, 16]. These previous reports have demonstrated that the medial meniscus is an important secondary restraint to anterior translation in the absence of a functional ACL due to its “wedge effect”. In a more recent study, Musahl et al. have described the effect of meniscectomy on the magnitude of the pivot shift in the ACL-deficient knee [20]. In this cadaveric study, lateral meniscectomy in the absence of an ACL resulted in a significant increase in the translation of the lateral, medial, and central compartments during combined axial, valgus, and rotatory load, while medial meniscectomy had no significant effect on tibial translation during the pivot shift test. The authors concluded that the lateral meniscus is an important restraint to tibial translation during the pivot shift maneuver.
There is a paucity of biomechanical data on the effect of meniscectomy following ACL reconstruction. In a single previous study evaluating anterior knee stability following meniscectomy in the single-bundle ACL-reconstructed knee, the authors found that in situ graft forces increased between 33 and 50% following medial meniscectomy, with no resultant increase in anterior translation under combined 200-N axial and 134-N anterior load [22]. In another cadaveric study, Seon et al. evaluated the effect of subtotal medial meniscectomy on the ACL-deficient and the single-bundle ACL-reconstructed knee subject to an anterior tibial load of 130-N and a quadriceps muscle load of 400-N. They demonstrated that while ACL-reconstruction significantly diminished abnormal anterior tibial translation, it did not restore anterior translation to the intact level with differences ranging from 2.6 mm at 0° to 5.5 mm at 30º of knee flexion [24].
In the current study, both nonanatomic (posterolateral tibia-anteromedial femur) and anteromedial (anteromedial tibia-posterolateral femur) ACL graft configurations were effective at controlling anterior tibial translation as measured by a navigated Lachman examination in the meniscus competent knee. However, the nonanatomic ACL reconstruction was sensitive to meniscus status and demonstrated instability during Lachman testing with both the unicompartmental and bicompartmental meniscectomy testing. The anteromedial ACL reconstruction appeared to provide superior control of anterior translation and to be relatively insensitive to meniscus status. One explanation for these findings may be that graft alignment oblique to the direction of anticipated displacement may result in improved control of that displacement [4]. Anatomic graft placement results in increased graft obliquity in the sagittal plane that should better control anterior translation. Accordingly, in the absence of secondary restraints to anterior translation such has the meniscus, an anatomic graft may be better suited to control anterior translation.
The data also demonstrate that sequential meniscal loss resulted in diminished control of rotational stability of the knee as measured by a mechanized pivot shift examination in both the anatomic and nonanatomic reconstructions. While anatomic graft configurations appeared to provide superior control to nonanatomic configurations following unicompartmental meniscectomy, neither single-bundle reconstruction method was capable of controlling lateral compartment translation following bicompartmental meniscectomy. These increases in observed lateral compartment translation have been previously shown to have a strong correlation with the clinical grade of the pivot shift [14].
In the nonmeniscectomized knee, Herbort et al. [9] have demonstrated similar results in regard to the influence of tunnel position on knee kinematics during single-bundle ACL reconstruction. In a cadaveric study, these authors demonstrated that single-bundle anteromedial reconstruction (anteromedial tibial footprint to anteromedial femoral footprint) more closely restored knee kinematics than nonanatomic reconstructions (posterolateral tibial footprint to anteromedial femoral footprint). Stability testing was not assessed under conditions of meniscal deficiency.
These aforementioned findings may have important clinical implications in patients with meniscal injury in the presence of an ACL graft. Patients undergoing total meniscectomy following single-bundle ACL reconstruction may be at risk of developing recurrent rotational instability and pivoting. Kocher et al. have demonstrated that subjective dissatisfaction following ACL reconstruction is strongly correlated with a positive finding on pivot shift examination [12]. Accordingly, attempts should be made to retain as much meniscal tissue as feasible or repair the torn meniscus in the ACL-reconstructed knee. Moreover, patients should be counseled as to the potential deleterious effects of meniscal loss following ACL reconstruction, particularly if the ACL reconstruction is perceived to be vertical in orientation.
The design of our study has limitations that should be addressed. A major limitation of this study is that no attempt was made to differentiate between the effects of medial and lateral unicompartmental meniscectomy on knee stability. However, the work of Musahl et al. suggests that while the medial meniscus has a greater role in control of anterior tibial translation in the ACL-deficient knee, the lateral meniscus is more important controlling rotational stability of the tibia as measured during a mechanized pivot shift in an identical model [20]. These findings may be extrapolated to the ACL-reconstructed knee, and further investigations are warranted to differentiate the relative contribution of each structure in this model. Another limitation of this study was the evaluation of total meniscectomy on knee stability, as bicompartmental total meniscectomy following ACL reconstruction is an uncommon clinical scenario. Future studies should evaluate the specific effects of partial meniscectomy on knee stability in this setting. Finally, the magnitude of force applied to the knee during the mechanized pivot shift is unknown, complicating comparisons with other biomechanical studies on this topic. However, the mechanized pivot shifter has excellent repeatability for translation magnitude during the pivot shift maneuver, and reliably induces a characteristic pathologic motion path that has been described both clinically and in cadaver studies of ACL insufficiency [14, 21]. Consequently, we are able to discern differences between experimental states in the absence of known forces across the knee joint.
Conclusion
Single-bundle ACL reconstruction can control abnormal anterior and rotational translation in the ACL-deficient knee. However, subsequent meniscal loss may result in recurrent instability as manifest to a lesser extent by increased anterior translation during Lachman examination and to a greater extent rotational instability as measured via the pivot shift. Anteromedial graft configurations may provide somewhat better protection against anterior translation and pivoting in the setting of meniscal loss. Based on the results of this study, surgeons should aim to preserve the meniscus in subsequent knee surgeries following single-bundle ACL-reconstruction to curtail potentially symptomatic instability.
References
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL (2000) Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 18:109–115
Bach BR, Warren RF, Wickiewicz TL (1988) The pivot shift phenomenon: results and description of a modified clinical test for anterior cruciate ligament insufficiency. Am J Sports Med 16:571–576
Bedi A, Musahl V, O’Loughlin P, Maak T, Citak M, Dixon P, Pearle AD (2010) A comparison of the effect of central anatomical single-bundle anterior cruciate ligament reconstruction and double-bundle anterior cruciate ligament reconstruction on pivot-shift kinematics. Am J Sports Med 38:1788–1794
Brophy RH, Pearle AD (2009) Single-bundle anterior cruciate ligament reconstruction: a comparison of conventional, central, and horizontal single-bundle virtual graft positions. Am J Sports Med 37:1317–1323
Brophy RH, Voos JE, Shannon FJ, Granchi CC, Wickiewicz TL, Warren RF, Pearle AD (2008) Changes in the length of virtual anterior cruciate ligament fibers during stability testing: a comparison of conventional single-bundle reconstruction and native anterior cruciate ligament. Am J Sports Med 36:2196–2203
Citak M, Suero EM, Rozell JC, Bosscher MR, Kuestermeyer J, Pearle AD (2010) A mechanized and standardized pivot shifter: technical description and first evaluation. Knee Surg Sports Traumatol Arthrosc 19(5):707–711
Colombet P, Robinson J, Christel P, Franceschi J-P, Djian P (2007) Using navigation to measure rotation kinematics during ACL reconstruction. Clin Orthop Relat Res 454:59–65
Hanley ST, Warren RF (1987) Arthroscopic meniscectomy in the anterior cruciate ligament-deficient knee. Arthroscopy 3:59–65
Herbort M, Lenschow S, Fu FH, Petersen W, Zantop T (2010) ACL mismatch reconstructions: influence of different tunnel placement strategies in single-bundle ACL reconstructions on the knee kinematics. Knee Surg Sports Traumatol Arthrosc 18:1551–1558
Hufner T, Kendoff D, Citak M, Geerling J, Krettek C (2006) Precision in orthopaedic computer navigation. Orthopade 35:1043–1055
Khadem R, Yeh CC, Sadeghi-Tehrani M, Bax MR, Johnson JA, Welch JN, Wilkinson EP, Shahidi R (2000) Comparative tracking error analysis of five different optical tracking systems. Comput Aided Surg 5:98–107
Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ (2004) Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med 32:629–634
Kwan MK, Lin TH, Woo SL (1993) On the viscoelastic properties of the anteromedial bundle of the anterior cruciate ligament. J Biomech 26:447–452
Lane CG, Warren RF, Stanford FC, Kendoff D, Pearle AD (2008) In vivo analysis of the pivot shift phenomenon during computer navigated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 16:487–492
Levy IM, Torzilli PA, Gould JD, Warren RF (1989) The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 71:401–406
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior–posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Lewis PB, Parameswaran AD, Rue JP, Bach BR Jr (2008) Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med 36:2028–2036
Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG (2009) Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am 91:2321–2328
Mae T, Shino K, Nakata K, Toritsuka Y, Otsubo H, Fujie H (2008) Optimization of graft fixation at the time of anterior cruciate ligament reconstruction. Part I: effect of initial tension. Am J Sports Med 36:1087–1093
Musahl V, Bedi A, Citak M, O’Loughlin P, Choi D, Pearle A (2010) The effect of medial versus lateral meniscectomy on the stability of the ACL-deficient knee. Am J Sports Med 38(8):1591–1597
Musahl V, Voos J, O’Loughlin PF, Stueber V, Kendoff D, Pearle AD (2009) Mechanized pivot shift test achieves greater accuracy than manual pivot shift test. Knee Surg Sports Traumatol Arthrosc 18(9):1208–1213
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Pearle AD, Solomon DJ, Wanich T, Moreau-Gaudry A, Granchi CC, Wickiewicz TL, Warren RF (2007) Reliability of navigated knee stability examination: a cadaveric evaluation. Am J Sports Med 35:1315–1320
Seon JK, Gadikota HR, Kozanek M, Oh LS, Gill TJ, Li G (2009) The effect of anterior cruciate ligament reconstruction on kinematics of the knee with combined anterior cruciate ligament injury and subtotal medial meniscectomy: an in vitro robotic investigation. Arthroscopy 25:123–130
Stindel E, Briard JL, Merloz P, Plaweski S, Dubrana F, Lefevre C, Troccaz J (2002) Bone morphing: 3D morphological data for total knee arthroplasty. Comput Aided Surg 7:156–168
Wu C, Noorani S, Vercillo F, Woo SL (2009) Tension patterns of the anteromedial and posterolateral grafts in a double-bundle anterior cruciate ligament reconstruction. J Orthop Res 27:879–884
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The investigation was carried out in the Computer Assisted Surgery Laboratory at Hospital for Special Surgery, New York, NY.
Rights and permissions
About this article
Cite this article
Petrigliano, F.A., Musahl, V., Suero, E.M. et al. Effect of meniscal loss on knee stability after single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 19 (Suppl 1), 86–93 (2011). https://doi.org/10.1007/s00167-011-1537-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1537-6