Abstract
Purpose
The purpose of this study was to determine the effects of a lateral meniscus posterior root tear, partial meniscectomy, and total meniscectomy on knee biomechanics in the setting of anterior cruciate ligament (ACL) reconstruction.
Methods
Thirteen fresh-frozen cadaver knees were tested with a robotic testing system under an 89.0-N anterior tibial load at full extension (FE), 15°, 30°, 60° and 90° of knee flexion and a simulated pivot-shift loading (7.0 Nm valgus and 5.0 Nm internal tibial rotation) at FE, 15° and 30° of knee flexion. Anterior tibial translation (ATT) and the in-situ force of ACL graft under the different loadings were measured in four knee states: (1) ACL reconstruction with intact lateral meniscus (Intact meniscus), (2) ACL reconstruction with lateral meniscal posterior root tear (Root tear), (3) ACL reconstruction with lateral posterior partial meniscectomy (Partial meniscectomy) and (4) ACL reconstruction with total lateral meniscectomy (Total meniscectomy).
Results
Under anterior tibial loading, compared with an intact meniscus, root tear significantly increased ATT at 15° and 30° of knee flexion (p < 0.05) and partial meniscectomy had almost same increased ATT as with root tear at any knee flexion between FE and 90°. Under simulated pivot-shift loading, total meniscectomy increased ATT compared with intact meniscus, root tear, partial meniscectomy at FE (p < 0.05).
Conclusion
Under anterior tibial and simulated pivot-shift loading, partial meniscectomy has no significant effect on the stability of ACL-reconstructed knee with lateral meniscal posterior root tear, while total meniscectomy increased laxity at less than 30° of knee flexion. Clinically, in cases of irreparable meniscal root tears or persistent pain a partial meniscectomy can be considered in the setting of ACL reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The menisci have been recognized as the secondary restraint to anterior–posterior translation and rotational movement in the knee [21, 26, 38]. Injuries to the posterior medial meniscus root attachments have been shown to be related to clinically significant meniscal extrusion [20], which patently affects meniscal biomechanics, finally resulting in degenerative changes within the knee joint [4, 14, 16, 30]. Clinically, meniscal injuries are common and frequently involved in ACL injury [3, 5, 13]. Several studies recently have reported that posterior lateral meniscus root tears occurred in 6.6–14% of patients with ACL tear [6,7,8, 24, 34].
Regarding posterior lateral meniscus root tear, the best treatment currently remains controversy [28]. The treatment options include non-operative treatment, meniscectomy (partial and total) and meniscal root repairs [4, 25]. Although indications for meniscal repair are constantly expanding, both for symptomatic relief and prevention of degenerative joint disease [4], meniscectomy is still widely performed for root tears or avulsions, providing short-term symptomatic relief with unknown long-term consequences [31]. It has been reported that partial meniscectomy and repair significantly both improve subjective outcome scores at a mean follow-up of 4 years [15].
Biomechanical studies have shown that meniscus root tears effectively destroyed the meniscus as a load-bearing structure by reducing the capacity to resist hoop stresses [10, 19]. Several recent studies suggest lateral meniscus posterior root tears increase significantly the peak tibiofemoral contact pressure in the lateral compartment reaching up to 50% [18, 33, 36]. A partial meniscectomy of the lateral meniscus concurrent with a slack anterior cruciate ligament substantially alter cartilage contact pressures [1]. For a posterior medial meniscal root tear, one study determined that it had a similar effect on knee peak tibiofemoral contact pressures as a total meniscectomy [37]. However, for a posterior lateral meniscal root tear, most of these studies focused on the contact pressure in the lateral compartment and ACL-deficient knee models [9, 11]. Nevertheless, the effect of meniscectomy over non-surgical treatment during ACL reconstruction on knee stability, that is more common to the clinical practice, is currently unknown.
Therefore, the purpose of this study was to assess how partial and total meniscectomy effect the anterior stability translation (ATT) of the knee and the in-situ force of ACL graft after ACL reconstruction combined with posterior lateral meniscus root tear. It is hypothesized that partial meniscectomy has no significant effect on the stability of the ACL-reconstructed knee while total meniscectomy would further increase the ATT compared with the root tear of the posterior lateral meniscus.
Materials and methods
Prior approval was obtained at the University of Pittsburgh for this human cadaver study from the Committee for Oversight of Research and Clinical Training Involving Decedents (CORID #785) and cadaver knee specimens were procured from approved tissue suppliers.
Arthroscopic inspection was performed on test specimens before inclusion to exclude serious osteoarthritis, meniscus injury and any ligamentous injuries. Eighteen fresh-frozen human cadaveric knee specimens were used and thirteen met the inclusion criteria. Six were female and seven were male with a mean age of 47 years (range from 42 to 59 years).
Prior to the testing, the knees were kept frozen at − 20 °C and thawed at room temperature for 24 hours. Once thawed, one surgeon removed the soft tissues beyond 15 cm proximal and distal to the knee joint line, with all capsular structures and ligaments kept intact. The distal ends of tibia and proximal femur bone were potted in an epoxy compound.
A robotic system (CASPAR Stäubli, Orto MAQUET) was used to test the knee kinematics that can repeat a position within ± 0.02 mm at each joint and a load cell (UFS; Model 4015; JR3 Inc.) with a force and moment accuracy of ± 0.2 N and ± 0.1 N m, respectively. A custom MATLAB program with a multitask operating system (Math Works Inc., Natick, Massachusetts, USA) was utilized to monitor knee kinematics and calculate the in-situ forces of the ACL and the reconstructed graft, with high test‐retest reliability.[2, 27, 29, 35, 41, 42, 44, 45] During the experiment, this testing system was operated in both the force- and displacement-control modes. With the tibia was attached to the robot while the femur was secured to a fixed platform, the passive flexion–extension path from FE to 90° of knee flexion was found by minimizing the external forces and moments applied to the joint at 0.5° increments of flexion [35]. At each incremental angle of knee flexion, the forces and moments generated by the specimen in the remaining 5-degree-of-freedom were minimized by the iterative algorithm of the robot control software.
The anatomic single bundle ACL reconstructions were performed using the three-portal technique. All reconstructions were performed arthroscopically and followed anatomic reconstruction principles [43] by the same surgeon. Previously harvested cadaver hamstring tendon grafts sized to 8-mm diameter were prepared for the ACL reconstructions. The ACL was sharply transected using a 11# blade and resected using a shaver. The femoral tunnel was drilled with an 8-mm cannulated femoral reamer using the transportal technique and the tibia tunnel was drilled using a tibial drill guide system (Smith and Nephew Endoscopy, Andover, MA) with an 8-mm diameter and 55° aimer angle. Following graft placement, the graft at the femoral end was fixed outside of lateral femoral cortex with an extra-cortical button. The graft at the tibial side was fixed using interference screw at 15° of knee flexion (measured with a manual goniometer) and 40 N using a manual tensioner (Meira Corp) [2]. Lastly, the suture of the graft at the tibial end was further fixed on a tibia using a post tie technique.
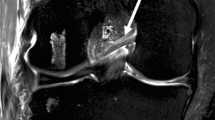
The lateral meniscal posterior root tear was made by cutting the root attachment under arthroscopy from the middle portal, and a punch was used from the anterior lateral portal to transect the lateral meniscal posterior root close to attachment including meniscofemoral ligament (MFL) (Fig. 1a). A posterior medial approach was built to help completely cut the MFL. A probe was used to confirm the mobility of the posterior lateral meniscus root to ensure full disruption of the lateral posterior root including the MFL. A Partial meniscectomy was performed by removing one third of the posterior lateral meniscus (Fig. 1b). A punch was first used and then a motorized shaver was used to remove the redundant of the inner edge of meniscus, making the rest of lateral meniscus smooth and stable. The total meniscectomy was made by a 11# sharp blade and punch and shaver. All of the meniscus tissue was removed from the capsule of the lateral knee (Fig. 1c).
A Arthroscopic anterior lateral portal view of lateral meniscus root tear including MFL (arrow) and a) schematic view of lateral meniscus root tear and cut MFL. B Partial meniscectomy-removal of one third of posterior lateral meniscus (arrow) b) schematic dotted black line indicating partial meniscectomy. C Total meniscectomy—removal of all the lateral meniscus tissue
Each group was evaluated with the following ACL and lateral meniscus states: (1) ACL reconstruction with intact lateral meniscus (Intact meniscus), (2) ACL reconstruction with posterior lateral meniscus root tear (Root tear), (3) ACL reconstruction with partial meniscectomy of posterior lateral meniscus part (Partial meniscectomy) and (4) ACL reconstruction with total lateral meniscectomy (Total meniscectomy). Since the focus of this study was on the lateral meniscal state and not on the ACL reconstruction, which has been well studied, the gold standard that was used was for comparison was the ACLR knee with an intact meniscus. Two different external loads were applied to the knees during testing: (1) an 89-N anterior tibial load, a simulated KT1000 test, to test anterior tibial translation (ATT) (mm) at full extension (FE), 15°,30°, 60° and 90° of knee flexion [41, 45], (2) a combined 5.0 Nm internal tibial and 7.0 Nm valgus torque, a simulated pivot-shift test, was applied to the specimen at full extension and at FE, 15° and 30° of knee flexion [17, 44].
The in-situ force of the ACL graft was calculated between the ACL deficient and ACL-reconstructed conditions at the same joint positions and loading [22, 32]. After each ACL and lateral meniscus status, external loads were applied to the ACL-reconstructed knee, and the motion was measured. After removal of the graft, the motion was replayed to determine the in-situ force experienced by the graft. By the principle of superposition, the change in the force before and after graft removal, with the knee in the same position, represents the in-situ force in the graft [22, 35].
Statistical analysis
One-way repeated-measures analysis of variance (ANOVA) was performed for each flexion angle to detect the overall effect of meniscus condition on ATT of the knee and the in-situ force of ACL graft. A Post hoc Tukey test was used for the statistical analysis between different ACL graft and meniscus status (SPSS version 17.0, SPSS, Chicago, IL, USA) with statistical significance when p < 0.05. To estimate the number of samples, an a priori power analysis, based on a 2-tailed paired t test, was performed (G*Power, v 3.1.9.2) with a significance level of 0.05, a power of 0.80, and a hypothesized effect size of d = 1.0, which resulted in a sample size of n = 10.
Results
Kinematics
After a root tear in the ACL-reconstructed knee, the amount of ATT increased significantly in comparison with the intact meniscus at 15° and 30° of knee flexion. With a partial meniscectomy, ATT was not different from a root tear, while a total meniscectomy increased ATT in comparison with the intact meniscus at all lower angles of knee flexion (Fig. 2).
Under simulated pivot-shift loading, the ATT after a total meniscectomy increased relative to all other knee states at FE, with respect to a partial meniscectomy at 15° and compared to the intact meniscus and root tear of flexion at 30° of knee flexion (Fig. 3).
Kinetics
Although meniscal damage tended to increase the ACL graft force, no significant differences were observed in the graft for the different knee states under anterior tibial loading (Fig. 4).
Also, no differences in graft force were found under simulated pivot-shift loading for the four knee states (Fig. 5).
Discussion
The most important findings of this cadaver study were that a root tear after ACL reconstruction increased ATT under anterior tibial loading at 30° or less of knee flexion and a partial meniscectomy did not significantly change the ATT while total meniscectomy significantly increased the ATT under anterior tibial loading and simulated pivot-shift loading. These findings support our hypotheses that a partial meniscectomy treatment for a lateral meniscal posterior root tear has no significant side effect on stability of the ACL-reconstructed knee while total meniscectomy increases the instability of knee after ACL reconstruction. For the in-situ force of ACL graft, no significantly difference was observed between intact meniscus, root tear, partial and total meniscectomy after ACL reconstruction at any knee flexion, although root tear, partial meniscectomy and total meniscectomy had a tendency to increase the in-situ force of ACL graft compared with intact meniscus at 15° and 30° of knee flexion angles under anterior tibial loading.
Posterior lateral meniscus root injuries are common and frequently in association with ACL tears [6,7,8, 24, 34] and the optimal treatment of meniscal root tears is still debated. Among these, partial or total meniscectomy, as a traditional surgical procedure, has been performed for meniscus tears or root avulsions for a long time, providing relief from short-term symptoms with possible long-term consequences [15, 32, 40]. Meniscectomy still is widely used. Recent data from the American Board of Orthopaedic Surgery Certification Examination Database (ABOS) showed the number of partial meniscectomies was significantly larger than root repair for treating meniscus injuries during ACL reconstruction [31]. This study analyzed the cases of meniscal repair, partial meniscectomy, and ACL reconstruction from 2004 to 2012. A total of 62,408 cases were treated by partial meniscectomy, while only 6,969 by meniscus repair. During ACL reconstruction, 7,657 cases were treated by meniscectomy, while 3,642 by meniscus repair.
No reports have been found on knee stability after lateral partial meniscectomy following ACL reconstruction. In our study, a root tear was found to increased ATT after ACL reconstruction under both anterior tibial and simulated pivot-shift loading; but no difference was found between root tear and partial meniscectomy. This suggest partial meniscectomy has no effect beyond that of a root tear on stability of ACL-reconstructed knee, which was in consistent with recently clinical studies [12, 39, 40]. In two multicenter, randomized, double-blind, sham-controlled trial in 146 patients who had knee symptoms consistent with a degenerative meniscus tear and no knee osteoarthritis, performed from 2007 to 2014, Sihvonen et al., demonstrated that partial meniscectomy and sham surgery had similar clinical outcomes including the Lysholm score, Western Ontario Meniscal Evaluation Tool (WOMET) score and knee pain at 12 months after operation and 2-year follow-up [39, 40]. In another multicenter, randomized, controlled trial involving symptomatic patients with a meniscal tear and evidence of mild-to-moderate osteoarthritis on imaging, Katz et al. also determined no significant difference on clinical results between partial meniscectomy and non-operative treatment (physical therapy) after 6 months of follow-up [12].
Therefore, for patients with chronic root tears and symptomatic grade 3 or 4 chondral lesions who failed non-operative treatment, or failed suture repair because of lower quality of soft tissue resulting from chronic damages and degenerative changes, patients with positive physical examination findings (i.e., clicking, positive McMurray test, joint line tenderness, and effusion) or patients with partial root tears and a substantial portion of the footprint still intact (exact percentage or quantity of footprint yet to be determined), partial meniscectomy remains the preferred treatment option [4, 23, 25]. After all, knee pain is usually the main reason that patients seek treatment and the advantages of partial meniscectomy over repair include decreased operative time, a less stringent postoperative rehabilitation protocol with no weight bearing restrictions and faster return to activities and sports [4].
Few published biomechanical studies have evaluated the effect of lateral total meniscectomy on laxity of the knee. In a recent study, Musahl et al. assess the stabilizing effect of the medial and lateral meniscus on ACL-deficient knees during the pivot-shift examination [26]. They found the ATT did not increase after lateral meniscectomy in the ACL-deficient knee under anterior tibial loading but significantly increased during the pivot-shift maneuver, which is not completely consistent with our study. This may be because, the model adopted in the Musahl et al. [26] study was the ACL-deficient knee, while in this study it was an ACL-reconstructed knee. The lateral meniscus root tear is more common during clinical ACL-reconstruction process; thus, the data might have the better clinical significance for surgical consideration.
In addition to the study of knee kinematics, data was collected on the effect of meniscectomy on the in-situ force of ACL graft in the four meniscus states. No significant difference was found in the in-situ force of ACL graft between the knee states at any knee flexion, although root tear, partial meniscectomy and total meniscectomy had a tendency to increase the in-situ force of ACL graft at 15° and 30° of knee flexion angles under anterior tibial loading, which is partly inconsistent with one previous study on the medial meniscus [29]. They found that the in-situ forces in the ACL graft increased between 33 and 50% after medial meniscectomy. The changes of the in-situ forces of ACL graft in Papageorgiou et al.’s study was higher than that of our study, which may be explained by that medial meniscus rather than the lateral meniscus was evaluated and anatomic ACL reconstruction was not performed. Clinically, this study supports that a partial meniscectomy treatment may be a selection for treating an irreparable lateral meniscal posterior root tear in the setting of ACL reconstruction, which can relieve the pain and faster return to activities and sports.
There are some limitations in this study. This study is a time-zero cadaver study which applied lower than physiologic loads and involved no muscle forces, but the applied knee loads have been widely used in assessing the biomechanics of different surgical procedures [2, 17, 44]. No significant differences could be found in the ACL graft force with meniscal state. Graft force tends to have a higher variation than knee kinematics, so a larger sample size may have been needed to elicit this difference. Lastly, this study did not include tibial-femoral contact pressure testing to evaluate the biomechanical effects on the meniscus. Nevertheless, this study supported our hypotheses that a partial meniscectomy treatment may be an option for treating an irreparable lateral meniscal posterior root tear.
Conclusion
Root tear after ACL reconstruction increased ATT at low flexion angles under anterior tibial loading and a partial meniscectomy has no further significant effects on knee laxity in the treatment of the lateral meniscal posterior root tear. However, in the ACL-reconstruction knee a total meniscectomy significantly increased laxity under simulated pivot-shift loading in comparison to a partial meniscectomy at low flexion angles. That suggests in cases of irreparable meniscal root tears or persistent pain that a partial rather than a complete meniscectomy should be considered in the setting of ACL reconstruction.
References
Allaire R, Muriuki M, Gilbertson L, Harner CD (2008) Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 90:1922–1931
Araujo PH, Asai S, Pinto M, Protta T, Middleton K, Linde-Rosen M et al (2015) ACL graft position affects in situ graft force following ACL reconstruction. J Bone Joint Surg Am 97:1767–1773
Bellabarba C, Bush-Joseph CA, Bach BR Jr (1997) Patterns of meniscal injury in the anterior cruciate-deficient knee: a review of the literature. Am J Orthop (Belle Mead NJ) 26:18–23
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF (2014) Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med 42:3016–3030
Bray RC, Dandy DJ (1989) Meniscal lesions and chronic anterior cruciate ligament deficiency. Meniscal tears occurring before and after reconstruction. J Bone Joint Surg Br 71:128–130
Brody JM, Lin HM, Hulstyn MJ, Tung GA (2006) Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology 239:805–810
De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K (2009) MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol 192:480–486
Forkel P, Reuter S, Sprenker F, Achtnich A, Herbst E, Imhoff A et al (2015) Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc 23:112–118
Forkel P, von Deimling C, Lacheta L, Imhoff FB, Foehr P, Willinger L et al (2018) Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 26:2302–2309
Greis PE, Bardana DD, Holmstrom MC, Burks RT (2002) Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg 10:168–176
Gupta RKA, Mittal N, Soni A, Khatri S, Masih GD (2018) The role of meniscal tears and meniscectomy in the mechanical stability of the anterior cruciate ligament deficient knee. Knee 25:1051–1056
Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL et al (2013) Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med 368:1675–1684
Keene GC, Bickerstaff D, Rae PJ, Paterson RS (1993) The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med 21:672–679
Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ et al (2013) Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc 21:2121–2125
Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG et al (2011) Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy 27:346–354
Koenig JH, Ranawat AS, Umans HR, Difelice GS (2009) Meniscal root tears: diagnosis and treatment. Arthroscopy 25:1025–1032
Kondo E, Merican AM, Yasuda K, Amis AA (2010) Biomechanical comparisons of knee stability after anterior cruciate ligament reconstruction between 2 clinically available transtibial procedures: anatomic double bundle versus single bundle. Am J Sports Med 38:1349–1358
LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF (2014) Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 96:471–479
Lee H, Petrofsky JS, Daher N, Berk L, Laymon M, Khowailed IA (2013) Anterior cruciate ligament elasticity and force for flexion during the menstrual cycle. Med Sci Monit 19:1080–1088
Lerer DB, Umans HR, Hu MX, Jones MH (2004) The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skeletal Radiol 33:569–574
Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am 64:883–888
Livesay GA, Fujie H, Kashiwaguchi S, Morrow DA, Fu FH, Woo SL (1995) Determination of the in situ forces and force distribution within the human anterior cruciate ligament. Ann Biomed Eng 23:467–474
Lyman S, Oh LS, Reinhardt KR, Mandl LA, Katz JN, Levy BA et al (2012) Surgical decision making for arthroscopic partial meniscectomy in patients aged over 40 years. Arthroscopy 28:492–501.e491
Matheny LM, Ockuly AC, Steadman JR, LaPrade RF (2015) Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc 23:3127–3131
Moatshe G, Chahla J, Slette E, Engebretsen L, Laprade RF (2016) Posterior meniscal root injuries. Acta Orthop 87:452–458
Musahl V, Citak M, O'Loughlin PF, Choi D, Bedi A, Pearle AD (2010) The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 38:1591–1597
Nakamura T Linde MA, Marshall BD, Koga H, Muneta T, Smolinski P, Fu FH (2019) Arthroscopic Centralization restores residual knee laxity in ACL-reconstructed knee with a lateral meniscus defect. Knee Surg Sports Traumatol Arthrosc 27:3699–3704
Pan F, Hua S, Ma Z (2015) Surgical treatment of combined posterior root tears of the lateral meniscus and ACL tears. Med Sci Monit 21:1345–1349
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH (2001) The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med 29:226–231
Papalia R, Vasta S, Franceschi F, D'Adamio S, Maffulli N, Denaro V (2013) Meniscal root tears: from basic science to ultimate surgery. Br Med Bull 106:91–115
Parker BR, Hurwitz S, Spang J, Creighton R, Kamath G (2016) Surgical trends in the treatment of meniscal tears: analysis of data from the American board of orthopaedic surgery certification examination database. Am J Sports Med 44:1717–1723
Pearse EO, Craig DM (2003) Partial meniscectomy in the presence of severe osteoarthritis does not hasten the symptomatic progression of osteoarthritis. Arthroscopy 19:963–968
Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, Prado Novoa M, Espejo-Reina A, Quintero Lopez C et al (2016) Comparative biomechanical study on contact alterations after lateral meniscus posterior root avulsion, transosseous reinsertion, and total meniscectomy. Arthroscopy 32:624–633
Praz C, Vieira TD, Saithna A, Rosentiel N, Kandhari V, Nogueira H et al (2019) risk factors for lateral meniscus posterior root tears in the anterior cruciate ligament-injured knee: an epidemiological analysis of 3956 patients from the SANTI study group. Am J Sports Med 47:598–605
Sakane M, Fox RJ, Woo SL, Livesay GA, Li G, Fu FH (1997) In situ forces in the anterior cruciate ligament and its bundles in response to anterior tibial loads. J Orthop Res 15:285–293
Schillhammer CK, Werner FW, Scuderi MG, Cannizzaro JP (2012) Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 40:2604–2609
Shirazi R, Shirazi-Adl A (2009) Analysis of partial meniscectomy and ACL reconstruction in knee joint biomechanics under a combined loading. Clin Biomech (Bristol, Avon) 24:755–761
Shybut TB, Vega CE, Haddad J, Alexander JW, Gold JE, Noble PC et al (2015) Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 43:905–911
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H et al (2018) Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis 77:188–195
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H et al (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369:2515–2524
Surer L, Michail K, Koken M, Yapici C, Zhu J, Marshall BD et al (2017) The effect of anterior cruciate ligament graft rotation on knee biomechanics. Knee Surg Sports Traumatol Arthrosc 25:1093–1100
Tang X, Marshall B, Wang JH, Zhu J, Li J, Smolinski P et al (2019) Lateral meniscal posterior root repair with anterior cruciate ligament reconstruction better restores knee stability. Am J Sports Med 47:59–65
van Eck CF, Lesniak BP, Schreiber VM, Fu FH (2010) Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 26:258–268
Xu Y, Liu J, Kramer S, Martins C, Kato Y, Linde-Rosen M et al (2011) Comparison of in situ forces and knee kinematics in anteromedial and high anteromedial bundle augmentation for partially ruptured anterior cruciate ligament. Am J Sports Med 39:272–278
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227
Acknowledgements
Not applicable.
Funding
Department of Orthopedic Surgery, University of Pittsburgh.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of this work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
Prior approval was obtained at the University of Pittsburgh for this human cadaver study from the Committee for Oversight of Research and Clinical Training Involving Decedents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tang, X., Marshall, B., Wang, J.H. et al. Partial meniscectomy does not affect the biomechanics of anterior cruciate ligament reconstructed knee with a lateral posterior meniscal root tear. Knee Surg Sports Traumatol Arthrosc 28, 3481–3487 (2020). https://doi.org/10.1007/s00167-020-06209-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06209-9