Abstract
The study evaluates the biomechanical properties of single-strand and single-loop tibialis (anterior and posterior) tendon allografts. A comparison was made with bone-patellar tendon-bone (BPTB) allografts. Sixty-four tendon allografts were evaluated in this study. Sixteen of these were single-strand tibialis anterior (TA) and 16 single-strand tibialis posterior (TP) tendons. Sixteen single-loop TA and TP tendons were also tested. The fourth group was composed of 16 BPTB allografts. The biomechanical properties determined were maximal load, stiffness, cross-sectional area and elongation. The results of this study showed that the maximal load of the single-loop tibialis tendons (1,553 ± 62 N) was greater than of the BPTB (1,139 ± 99 N), TA (776 ± 43 N) and TP (888 ± 64 N) tendons. The stiffness of the single-loop tibialis tendons (236 ± 10 N/mm) was also greater than of the BPTB (168 ± 13 N/mm), TA (60 ± 2 N/mm) and TP (73 ± 5 N/mm) tendons. The cross-sectional area of the BPTB tendons was 67 ± 5 mm2, of the single-loop tibialis tendons 36 ± 2 mm2, of the TA tendons 20 ± 1 mm2, and of the TP tendons 23 ± 1 mm2. The elongation of the single-loop tibialis tendons and of the BPTB tendons was almost similar (7 ± 0.4 mm). The same applied to the TA and TP tendons (14 ± 0.6 mm). The results of this in vitro mechanical study suggest that fresh-frozen single-loop TA and TP tendons, and BPTB allografts are an acceptable substitute for hamstrings in anterior cruciate ligament reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allograft tendons can be very useful in the reconstruction of ruptured anterior cruciate ligaments (ACL). Some patient characteristics dictate the use of one graft source over another. For example, athletes are better served with autograft tendons while patients over 45 years of age are good candidates for allograft tissues because they recover more quickly [14]. The morbidity from graft procurement is eliminated and extensor mechanism problems are less likely to occur with allografts [14, 15]. Individuals with a history of patellofemoral pain or previous patellar surgery (e.g. realignment, tendon repair, fracture) are good candidates for allografts, because postoperative anterior knee pain can occur if an autologous hamstring tendon is used [14, 15]. Avoidance of donor site morbidity with use of allograft tissues allows early return to work. Allografts are considered to be a good substitute for autografts in revision of ACL reconstruction and in knees with multiple ligament injuries [14, 15].
The use of allograft tissue allows for a smaller incision. Patients undergoing ACL reconstruction with an allograft tendon have less postoperative pain and quickly recover muscle strength [14].
The issues related to either the success or failure of an allograft transplant include immunogenicity, type of preservation, disease transmission, remodelling, tunnel position, graft position, initial graft tension and rehabilitation methods [17]. Previous clinical studies on the use of allograft tissue to reconstruct the ACL reported no evidence of rejection when the tissue had been frozen [3, 7, 10]. The risk of transmitting diseases, such as human immunodeficiency virus, is minimal with secondary gamma irradiation and donor screening [3, 7, 10]. However, a small percentage of donors may have a transmittable disease but have not yet formed identifiable antibodies for disease detection. Gamma irradiation can significantly diminish the strength of tendons at doses higher than 2.5 Mrad [14].
In general, infection is a rare complication of autograft and allograft ACL reconstruction [14].
Remodelling studies have shown that although ligamentization of allografts takes longer than of autografts, the final clinical results are largely similar [3, 7]. Although initial cell viability is slightly lower in allografts, the entire allograft is populated by cells after 9 months with normal orientation of collagen bundles [3, 7]. A histological study of tendon allograft biopsy specimens obtained during follow-up arthroscopy showed that new collagen was formed in the third postoperative month and that collagenization and remodelling continued until the second postoperative year, at which time there no longer was a significant biomechanical difference between allografts and autografts [15].
The purpose of this study was to determine the maximal load to rupture, stiffness, cross-sectional area and elongation of single-strand and single-loop TA and TP tendons, and BPTB tendons. These groups were compared with each other and also with the mechanical properties of normal ACL, reported in previous studies [1–3, 5, 8, 9, 13, 16].
Materials and methods
Tissue procurement and graft preparation
Sixteen BPTB tendons and 48 tibialis tendons (24 TA and 24 TP) were evaluated in this study. Another eight tendons were excluded because they had been damaged during the preparations for the experiment.
The TA and TP tendons were harvested from different donors with a mean age of 57 years (range 16–82 years). The BPTB tendons were harvested from different donors with a mean age of 59 years (range 16–82 years).
All the tendons were fresh-frozen after harvesting within 24 h postmortem. The night before the experiment they were thawed to 4°C and then kept at room temperature 1 h before the start of the experiments.
The tibialis tendons were prepared in the same way as for the reconstruction procedure. The muscle tissue was removed and the two ends were gripped with a soft isolating surface to avoid damaging the tendons.
To test the BPTB complex, bone cubes containing the tendon ends were prepared and clamped without applying any tensile load on the tendon itself, but on the bony part of the BPTB complex. The full width of the BPTB tendons was used to avoid damaging the tendon.
Structural and material tests
The structural and material properties of each graft were determined from a load-to-failure test by using a computerized materials testing machine (LR50K Lloyd) with a constant rate of displacement of 6 mm/min [4, 6, 11].
Before testing, the cross-sectional area (A) of each graft was measured with a self-made area micrometer [4]. Three measurements (two at the ends and one in the middle of the tendons) were averaged. Maximal load, stiffness and elongation were determined.
The tibialis tendons were divided into two groups. The first group consisted of single-strand TA (16) and TP (16) tendons, the second group of single-loop TA (8) and TP (8) tendons. The BPTB group consisted of 16 tendons.
Single strand
At the two ends where the tensile load was applied, two adjustable clamps were used, which could manually be firmly secured to avoid graft slippage. Before securing the tendons in the clamps, their ends were covered with blotting paper to avoid tendon damage. The orientation of the clamps at the two ends was similar for each graft.
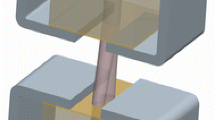
Single loop
The TA and TP tendons were looped around a 6-mm bar fixed to the traction machine, while the two ends of the tendons were clamped together [3].
Care was taken during mounting to prevent preloading of the graft. The moistness of the grafts during testing was maintained by constantly spraying the grafts with a physiological solution (NaCl 0.9).
Data analysis
The structural and material properties of each graft were determined from a plot of load versus elongation. The real elongation of the graft after a tensile load had been applied by the traction machine, was calculated by drawing a tangent to the load versus elongation curve by means of linear regression. The point where tangent and x-axis met, was taken as the real starting point of the elongation of the tendon, and the end point of elongation was the x co-ordinate of the maximal load (Fig. 1).
In this diagram, point A represents the onset of rupture of the tendon. Point B is where the X-axis (elongation of the tendon) meets the straight line that has been drawn from point A. To measure the actual elongation of the tendons, a tangent to the linear phase of the elongation curve was drawn. Next, a perpendicular line from the point of onset of rupture was drawn. The distance between the intersection of the tangent and the perpendicular line was equal to the actual elongation we wished to measure
Statistical analysis
The GraphPad Prism software package was used for statistical analysis of the data. The Turkey-Kramer multiple comparison test was applied. If the Q value was greater than 3.737, then the P value was less than 0.05 and this value was considered to be statistically significant.
Results
The tendons investigated all failed at random either in the middle, at one of their ends or for the patellar tendons at their junctions to bone. The mean value and corresponding standard deviation, and the minimal/maximal values for each of the four structural parameters in the TA, TP, BPTB and single-loop tibialis group are given in Table 2. Figure 2 shows a representative load versus elongation curve for the TA, TP, BPTB and single-loop tibialis group.
The statistical results (Table 1) for the four structural properties, the average maximal load to rupture, stiffness, elongation and cross-sectional area, showed no significant difference between the single-strand TA and TP grafts.
No significant difference in the four parameters was observed between the two single-loop tibialis tendon groups. Consequently, we considered these two groups (8 TA and 8 TP) as one group of 16 tendons, which was compared with the BPTB (16 tendons) group and the single-strand TA (16 tendons) and TP group (16 tendons).
The average maximal load to rupture of the BPTB grafts (1,139.3 N) was significantly greater than of the TA tendon grafts (776.87 N) (P < 0.01). Although the average maximal load to rupture of the BPTB grafts was also greater than of the TP tendon grafts (888.81 N), the difference was not significant (P > 0.05). The average maximal load to rupture of the single-loop tibialis tendons (1,553.0 N) was significantly greater than of the other three groups (P < 0.001) as shown in Fig. 2.
The average stiffness of the TA tendon grafts (60.9 N/mm) and the TP tendon grafts (73.8 N/mm) was significantly less than of the BPTB grafts (168.78 N/mm) (P < 0.001). The average stiffness of the single-loop tibialis tendons (236.33 N/mm) was significantly greater than of the other three groups (P < 0.001), as shown in Fig. 2.
The elongation of the BPTB grafts (7.270 mm) and of the single-loop tibialis tendons (7.58 mm) was significantly less than of the single-strand TA and TP tendons (P < 0.001). No significant difference in elongation was found between the BPTB group and the single- loop tibialis group (P > 0.05).
A significantly larger cross-sectional area (67.843 mm2) was found in the BPTB group compared with the average cross-sectional areas of the TA (20.658 mm2), TP (23.925 mm2) and single-loop tibialis group (36.91 mm2) (P < 0.001). This last group also had a significantly larger cross-sectional area than the TA (P < 0.01) and the TP group (P < 0.05).
Discussion
This study presents the biomechanical properties of substitutes for the human ACL using tissues obtained from adult human donors. Our biomechanical data are only few of many criteria that are important to the clinical success of ACL reconstruction. Equally important are care in graft preparation at surgery, adequate placement and fixation of the tendon ends, and a complex remodelling process including revascularization and ligamentization [3, 14, 15, 17].
Caution must be exerted in comparing the results of our study with those of others. Differences in the choice of grips are important. Specimens must be held with minimal slippage or crushing effects. While slippage produces errors in elongation measurements, crushing can result in premature failure and lower strength values. The gripping system in this study produced acceptable results with less tissue damage [4, 6, 11].
From Table 2 it appears that the maximal load of the BPTB grafts in this study was very similar to another study in which a mean value of 1085.7 N was reported [12], but the rate of elongation was about 10 times higher than in our study. BPTB grafts have proved to be a good substitute for ACL.
The results of BPTB grafts in this study were compared with those of TA and TP grafts, to verify if tibialis tendons could be used for ACL reconstruction. To obtain tensile structural values of tibialis tendons comparable with (or higher than) those of BPTB tendons, single-loop tibialis tendons should be used, because these tensile properties are additive with the number of strands. Tests with single-loop tibialis tendons (TA and TP) have shown that the maximal load and stiffness are indeed almost double. Looping the tendons doubles the area and gives a diameter close to the diameter of ACL. The stiffness of ACL (242 ± 28 N/mm) as calculated in a recent study, is close to our results for the single-loop TA and TP tendons (236 ± 10 N/mm) [17].
This study provides biomechanical data on potential grafts for ACL reconstruction, in comparison to single-strand BPTB grafts. Tibialis tendons (TA and TP) should be constructed as single loops.
References
Arnauw G, Verdonk R, Harth A, Moerman J, Vorlat P, Bataillie F, Claessens H (1991) Prosthetic versus tendon allograft replacement of ACL deficient knees. Acta Orthop Belg 57:67–74
Chang S, Egami D, Shaieb M, Kan D, Richardson A (2003) Anterior cruciate ligament reconstruction: allograft versus autograft. Arthroscopy 19:453–462
Haut Donahue TL, Howell SM, Hull ML, Gregersen C (2002) A biomechanical evaluation of anterior and posterior tibialis tendons as suitable single-loop anterior cruciate ligament grafts. Arthroscopy 18:589–597
Ellis D (1969) Cross-sectional area measurements for tendon specimens. A comparison of several methods. J Biomech 2:175–186
Engebretsen L, Lewis J (1996) Graft selection and biomechanical considerations in ACL reconstruction (isometry, stress, preload). Sports Med Arthrosc Rev 4:336–341
Gordon L, Dysarz F, Venkateswara K, Mok A, Ritchie R, Rabinowitz S (1999) Flexor tendon repair using a stainless steel external splint. Biomechanical study on human cadaver flexor tendons. J Hand Surg 6:654–657
Grood E, Noyes F (1976) Cruciate ligament prosthesis: strength, creep, and fatigue properties. J Bone Joint Surg Am 58:1083–1088
Noyes F, DeLucas J, Torvik P (1974) Biomechanics of anterior cruciate ligament failure : an analysis of strain-rate sensitivity and mechanisms of failure in primates. J Bone Joint Surg Am 56:236–252
Noyes F, Grood E (1976) The strength of the anterior cruciate ligament in humans and rhesus monkeys. J Bone Joint Surg Am 58:1074–1082
Noyes F, Butler D, Grood E, Zernicke R, Hefzy M (1984) Biomechanical analysis of ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66:344–352
Probst A, Palmes D, Freise H, Langer M, Joist A, Spiegel HU (2000) A new clamping technique for biomechanical testing of tendons in small animals. J Invest Surg 13:313–318
Rupp S, Seil R, Kohn D, Muller B (2000) The influence of avascularity on the mechanical properties of human bone-patellar-tendon-bone grafts. J Bone Joint Surg Br 82:1059–1064
Steenbrugge F, Verdonk R, Vorlat P, Mortier F, Verstraete K (2001) Repair of chronic ruptures of the anterior cruciate ligament using allograft reconstruction and a ligament augmentation device. Acta Orthop Belg 67:252–257
Strickland S, MacGillivray J, Warren R (2003) Anterior cruciate ligament reconstruction with allograft tendons. Orthop Clin N Am 34:41–47
Vorlat P, Verdonk R, Arnauw G (1999) Long-term results of tendon allografts for anterior cruciate ligament replacement in revision surgery and in cases of combined complex injuries. Knee Surg Sports Traumatol Arthrosc 7:318–322
Woo S, Kanamori A, Zeminski J, Yagi M, Papageorgioo C, Fu F (2002) The effectiveness of reconstruction of the anterior cruciate ligament with hamstrings and patellar tendon. J Bone Joint Surg Am 84:907–914
Woo S, Karaoglu S, Dede O (2006) Contributions of biomechanics to ACL reconstruction. Acta Orthop Traumatol Turc 40:94–100
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Almqvist, K.F., Jan, H., Vercruysse, C. et al. The tibialis tendon as a valuable anterior cruciate ligament allograft substitute: biomechanical properties. Knee Surg Sports Traumatol Arthr 15, 1326–1330 (2007). https://doi.org/10.1007/s00167-007-0396-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0396-7