Abstract
Purpose
Despite increasing interest in utilizing quadriceps tendon (QT) grafts in anterior cruciate ligament reconstruction (ACLR), data on the optimal quadriceps graft thickness are limited. The purpose of this study was to characterize the mechanical properties for the quadriceps tendon, comparing full-thickness (FT) QT grafts with and without bone to a partial-thickness (PT) QT graft, and comparing the three QT grafts to four-stranded semitendinosus (4-SST) and bone-patellar tendon-bone (BTB) grafts and one experimental graft, the two-stranded rectus femoris (RF).
Methods
Forty-eight (n = 48) young cadaveric grafts (mean age 32 ± 6 years) were utilized for testing with N = 8 specimens in each of the following groups; (1) FT QT with bone, (2) FT QT without bone, (3) PT QT without bone, (4) BTB, (5) RF, and (6) 4-SST. Each specimen was harvested and rigidly fixed in custom clamps to a dynamic tensile testing machine for biomechanical evaluation. Graft ultimate load and stiffness were recorded. Independent groups one-factor ANOVAs and Tukey’s pairwise comparisons were performed for statistical analyses.
Results
FT QT with bone and 4-SST grafts demonstrated similar ultimate loads to BTB grafts (both n.s), whereas PT QT demonstrate statistically significantly lower ultimate loads to BTB grafts (n.s) and 4-SST grafts (n.s). Furthermore, no statistically significant differences were observed between the ultimate loads of FT QT vs. PT QT grafts without bone (n.s) or between FT QT with vs. without bone (n.s). FT QT grafts with bone did not demonstrate statistically significantly greater ultimate loads than PT QT grafts without bone (n.s). The RF graft demonstrated statistically significantly lower ultimate loads to BTB grafts (p < 0.005) and 4-SST grafts (p < 0.014).
Conclusions
Full thickness QT grafts with bone had similar material properties to BTB and a 4-SST grafts, while Partial thickness QT graft without bone had significantly lower material properties than BTB and 4-SST, in a biomechanical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The dominant prevalence of anterior cruciate ligament (ACL) injuries is ubiquitous in orthopedics, and particularly in the younger population, age 16–40 years old, with an estimated annual incidence of 85 per 100,000 citizens in this group [9, 21,22,23]. The “gold standard” treatment for ACL injuries in the young active population currently favors single-bundle ACL reconstructions (ACLR) [7, 36] with the predominant graft choice being BTB and HT autografts [3, 28].
There has been an increased interest in utilization of QT autograft for ACLR due to complications after BTB harvesting, such as anterior knee pain [2, 8, 10], patella fracture [28], and patellofemoral osteoarthritis (OA) [9, 17]. In addition, HT autografts have been associated with increased risk of postoperative joint laxity, functional hamstring weakness, and increased graft failure and revision rates [9, 21, 22]. Some authors utilize a FT QT graft, others advocate for a PT QT graft [6, 27]. QT graft has reported similar mechanical properties in comparison with the BTB or the HT grafts [11, 26, 29, 30]. To the authors’ knowledge, direct mechanical properties of BTB, HT, and different types of QT grafts have not previously been evaluated in a single study.
When reconstructing the ACL, it is important to choose a graft that has similar properties to the native ACL. This study provides a comparison of biomechanical properties of several potential grafts in ACL reconstruction in specimens younger than 40 years of age. Therefore, the purpose of this study was to characterize the mechanical properties of the quadriceps tendon, comparing FT QT grafts with and without bone to a PT QT graft, and comparing the three QT grafts to 4-SST, BTB grafts, and one experimental graft, the two-stranded rectus femoris (RF). It was hypothesized that there will not be any difference in ultimate load and stiffness between the tested grafts.
Materials and methods
A total of 48 allografts suitable for ACLR grafts were obtained for this study. The cadaveric specimens utilized in this study were donated to a tissue bank for medical research and then purchased by our institution. All specimens were stored at − 20 °C and thawed at room temperature for 24 h prior to preparation. All specimens were under 40 years of age with no history or signs of previous injury, surgical history or gross abnormality.
Mean specimen age was 32 ± 6 years (range 18–39 years). PT QT grafts consisted of the rectus femoris and a partial thickness vastus medialis and vastus lateralis tendon graft [12, 14]. The rectus femoris graft in this study was an isolated rectus femoris (dissected of a QT) and folded to create a double layer, or as referred to in this article, a two-stranded rectus femoris graft (RF). Six groups of viable allografts for ACLR were obtained for this study: group 1: FT QT with bone, group 2: FT QT without bone, group 3: PT QT without bone, group 4: BTB, group 5: RF, and group 6: 4-SST. There were 8 specimens per group. Young adult cadavers were utilized primarily because the majority of patients treated undergoing ACLR are < 40 years of age. There were no significant differences in specimen age, BMI, and weight between the groups.
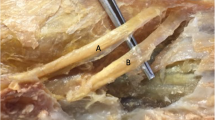
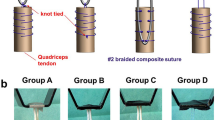
The grafts were prepared to the allocated size (Fig. 1). The QT grafts of group 1–3 were prepared with a 10-mm-wide double-bladed knife (Storz Medical AG, Tägerwilen, Switzerland) to ensure symmetric size of the tendon graft and a minimum length of 80 mm. All QT grafts had 25 mm of exposed tendon between the two clamps in order to try to simulate a native ACL length [1, 19, 32]. For bone plug harvesting, a 10 mm width and a 25 mm length were measured, and a sagittal saw (Smith & Nephew Inc., Andover, Massachusetts) was used to harvest the bone plug. The PT QT grafts in group 3 were further prepared with a 5 mm separator knife (Storz Medical AG, Tägerwilen, Switzerland) to ensure symmetric thickness (resulting in harvesting of the RF tendon and partial harvesting of the “second layer” of the QT consisting of the vastus medialis and vastus lateralis [12, 14]). Group 4, BTB, were harvested with a 10 × 25 mm bone plug from the patella and tibial tubercle using an oscillating saw, and the tendon part using the 10 mm double-bladed knife. The soft-tissue or patellar tendon part of the BTB graft had a median length 47 mm (range 30–60 mm). Group 5, RF, were harvested using the 10 mm double bladed knife from the central part of the RF tendon. A total length of 140 mm was dissected out by peeling of the superficial layer of the QT and stripping of the muscle belly of the rectus femoris muscle on the proximal part of the RF tendon. The tendon was then folded at the midpoint of the graft to form a double layered (two-stranded) 10-mm-wide graft with a total length of 70 mm. Group 6, 4-SST, were a minimum of 28 cm in length and were folded to form a four-stranded ST graft with a mean diameter 8.5 mm. All grafts were stored at − 20 °C and thawed at room temperature on the day of testing.
Each end of the tendons was enclosed within nylon tubing secured via suture; nylon tubing was used to reduce the destructive pressure of the graft at their site of clamping, as has been observed in our pilot studies (Fig. 2). A double whip-stitch suture with a braided suture (Ultrabraid suture, Smith & Nephew Inc., Andover, Massachusetts) was used to ensure equal tension of all four strands on the ST specimens.
Specimens were randomly organized a priori such that one tendon from each of the six groups was tested in a given testing cycle, and this was repeated for eight cycles. The order in which the tendons were tested was otherwise randomized.
Each tendon was biomechanically evaluated on a dynamic tensile testing machine (Instron ElectroPuls E10000; Instron Systems, Norwood, Massachusetts, USA; full-scale range: ± 10 kN; stroke: ± 30 mm). Measurement error of the device was certified within the year by Instron to be ≤ ± 0.300% of the indicated displacement and ± 1.0% of the indicated force [13]. The nylon-enclosed ends of the grafts were rigidly fixed in custom clamps to the tensile testing machine for biomechanical evaluation. A length of 25 mm of graft was exposed between the clamps with exception of the BTB grafts that were clamped at the bone plugs. A minimum residual length of 2 mm of nylon was left exposed above or below the edge of the clamps in order to prevent direct contact of the specimen with the teeth of the clamps. All clamps were evenly tightened with 1.8 kg m of torque using an analogue torque-wrench (Proto J6113F; Stanley Black & Decker, Southington, CT, USA). Grafts were initially tensioned to 10 N, then cyclically loaded between 10 and 400 N [31] for 5 cycles at 1 Hz; force and displacement data were recorded at 100 Hz. This cyclic loading was implemented to ensure there was no slippage of the specimens within the clamps and to allow for a measure of cyclic graft stiffness before failure. After the cyclic loading, the grafts were finally pulled to failure at a rate of 1 mm/s; force and displacement data were recorded at 500 Hz. At failure, the mode and site of failure were documented.
Statistical analyses
Raw data were accurately measured and recorded to the third and fourth decimal place for displacement and force, respectively; data were preserved in this format throughout all calculations and ultimately reduced (by rounding) to preserve only 3 significant figures for simplicity in interpretation of the results. Linear regressions were calculated in MATLAB (R2019b, The MathWorks, Inc., Natick, Massachusetts, USA) using force data as a function of displacement data during the linear portion of each cycle of graft tensioning from 10 to 400 N. Cyclic graft stiffness was calculated by averaging the slopes of these regressions for an adjusted 4 cycles, excluding the first cycle that characteristically represents nonlinear elongation as the tendons settled into the clamps [15]. Similarly, the pull-to-failure graft stiffness was calculated using a linear regression of the linear portion of the load vs. displacement curve during the pull-to-failure stage of testing. The ultimate load was taken as the maximum force observed on the actuator before a 5% reduction in force occurred.
Means and standard deviations were reported for each group. Mean differences among graft groups with respect to ultimate tensile force and stiffness were compared using independent samples analysis of variance (ANOVA). In cases where the overall null hypothesis of no group difference was rejected, Tukey post hoc pairwise comparisons were performed. Tukey-adjusted p values smaller than 0.05 were considered statistically significant. All statistical analysis was performed using the statistical computing language R version 4.0.3 (access date January 13, 2021; R Core Team, R Foundation for Statistical Computing, Vienna, Austria).
Statistical power was considered with respect to a fixed feasible sample size. Assuming two-tailed testing and a type-1 error rate per pairwise comparison of 0.05, 8 specimens per group were sufficient to detect a Cohen’s effect size of d = 1.51 with 80% statistical power.
Results
Ultimate load
Relative to the baseline of BTB grafts, only 4-SST and FT QT with bone grafts demonstrated similar ultimate loads (both n.s). Both PT QT and FT QT without bone grafts demonstrated statistically significantly lower ultimate loads than the BTB (p < 0.001 and p = 0.025, respectively) and were not statistically significantly different from each other (n.s). FT QT grafts with bone did not have a statistically significant greater ultimate load than PT QT grafts without bone (mean difference = 479 N, 95% Confidence Interval (CI) [− 985, 28], p = n.s). The relative distributions of ultimate load and stiffness for each group are demonstrated graphically in Figs. 3 and 4 and numerically in Table 1. The results of all adjusted Tukey pair-wise post hoc comparisons made for ultimate load are presented in Table 2.
A Boxplot model showing ultimate load (N) among the different ACL graft types tested. Dots represent individual specimen observations. Thick horizontal lines represent group medians, while top and bottom of boxes represent the 25th and 75th percentiles, respectively. Asterisks and brackets represent significant pairwise comparisons between groups (p < 0.05). BTB bone-patellar tendon-bone, FT QT no bone full thickness quadriceps tendon with no bone, FT QT with bone full thickness quadriceps tendon with bone, PT QT no bone partial thickness quadriceps tendon with no bone, two-stranded RF two-stranded rectus femoris, 4-SST four-stranded semitendinosus
A Boxplot model with a comparison of stiffness, cyclic loading, and pull-to-failure. Boxplots comparing stiffness (N/mm) during A cyclic loading and B pull-to-failure among ACL graft groups. Dots represent individual specimen observations. Thick horizontal lines represent group medians, while top and bottom of boxes represent the 25th and 75th percentiles, respectively. Asterisks and brackets represent statistically significant pairwise comparisons between groups (p < 0.05). Dashed brackets are to clarify p values of specific comparisons. BTB bone-patellar tendon-bone, FT QT no bone full thickness quadriceps tendon with no bone, FT QT with bone full thickness quadriceps tendon with bone, PT QT no bone partial thickness quadriceps tendon with no bone, two-stranded RF two-stranded rectus femoris, 4-SST four-stranded semitendinosus
Cyclic loading stiffness
RF and 4-SST grafts demonstrated statistically significantly higher stiffness than all other ACL grafts (all p < 0.05); however, RF and 4-SST grafts were not significantly different from each other (n.s). All variations of QT demonstrated similar cyclic loading stiffness compared to BTB. Mean stiffness was within 25 N/mm and not statistically different among the FT QT with bone, FT QT without bone, PT QT without bone, and BTB graft groups.
Pull-to-failure stiffness
During the pull-to-failure stage of testing, all grafts demonstrated similar stiffness values comparable to BTB (all n.s). PT QT without bone demonstrated statistically significantly lower stiffness values compared to FT QT with bone (p = 0.006) and 4-SST (p < 0.001). The 4-SST graft also demonstrated statistically significantly higher stiffness than both the FT QT without bone (p < 0.001) and the RF graft (p = 0.003); however, no differences were observed between 4-SST and FT QT with bone grafts (n.s).
Failure site
Each graft primarily failed in specific ways. FT QT with bone grafts all failed at the bone tendon interface (8/8). FT QT without bone failed at the proximal end of the graft (5/8) and universal stretch (3/8). PT QT without bone failed at the distal end (5/8) via universal stretch and via a mid-substance rupture. BTB grafts failed at the deeper fiber structures of the patella interface (6/8) and (2/8) at the deep layer of the tibial bone interface. Two-stranded RF tendons failed via universal stretch (5/8) and via mid-substance rupture (3/8). Finally, 4-SST grafts failed equally between universal stretch (4/8) and mid-substance tears (4/8).
Discussion
The most important finding of this study was that a FT QT graft with bone demonstrated an equivalent ultimate load as BTB and 4-SST grafts, while PT QT graft without bone had a significantly lower ultimate load than BTB and 4-SST grafts in a biomechanical setting. Furthermore, there was no difference in biomechanical properties between the different QT grafts; however, the load to failure for PT QT was 44–55% lower than native ACL [20, 35].
The biomechanical analysis of the native ACL by Noyes et al. [20] and Woo et al. [35] reported ultimate load of 1725 ± 269 N and 2160 ± 157 N, respectively. In this study, it was found that FT QT grafts with bone (1450 ± 362 N) were the only graft to demonstrate similar ultimate load, cyclic stiffness, and pull-to-failure stiffness to the BTB graft and 4-SST graft. BTB (1810 ± 397 N) and 4-SST (1750 ± 316 N) ultimate load values in this study were also higher than the ultimate load for the native ACL reported in the literature by Noyes et al. [20]. In addition, they were generally stronger than PT QT grafts without bone (972 ± 372 N), although not significantly different. Future larger biomechanical studies may be able to demonstrate these potentially clinically meaningful differences with statistical significance. The FT QT with bone in this study have reported < 16% lower ultimate load values in load to failure than the native ACL, and the FT QT without bone were 27% lower [20]. PT QT without bone reported 44% lower ultimate load value compared to the study by Noyes et al. [20] and as high as 55% lower ultimate load value compared to the ultimate load of the native ACL in the study by Woo et al. [35].
The intention of the experimental RF graft was to see if this graft could be a viable alternative graft choice to the PT QT without bone. There was no significant difference in ultimate load of the RF graft (1160 ± 308) in comparison with the PT QT without bone (972 ± 372). However, the RF graft had 33–47% lower value in ultimate load than the native ACL. This may question the intended use in a clinical setting of an ACL graft to restore the biomechanics of the knee.
Therefore, a FT QT graft with bone, BTB, or a 4-SST graft should be considered for ACLR over FT QT without bone as well as PT QT in order to best restore native ACL material properties. Additionally, harvesting of grafts with a bone plug should be considered when trying to maximize the ultimate load of the FT QT graft in ACLR. PT QT grafts without bone should be used with caution for replacement for the native ACL due to their significantly inferior biomechanical properties.
Previous studies have investigated the biomechanical comparison of either QT to BTB [27] or QT to HT [24, 33] grafts. Schmidt et al. [25] performed a biomechanical study comparing multiple ACL grafts including QT graft. The study did not, however, compare different types of QT grafts to BTB and HT graft. Schmidt et al. [25] reported on the comparison of a FT QT, BTB, HT, and Iliotibial band graft, and the mean age of the specimens was only 9.2 -years old which is a much younger population than the typical ACL patient group [25]. To obtain clinical relevance for adult patients, we included specimens between 18 and 40 years old.
An important finding of the present study was the significantly inferior ultimate load of the PT QT graft when compared to BTB and 4-SST, and also when compared to ultimate load of the native ACL [35]. Many of the current harvesting devices available are designed for partial tendon harvesting to preserve quadriceps strength, and to avoid violation of the suprapatellar pouch and potential muscle herniation [6, 27]. The significantly inferior ultimate load found in this study of the PT QT graft may question the benefit of using partial QT harvesting devices when harvesting a QT graft. In the meta-analyses by Mouarbes et al. [18], they found no significant difference failure rate, functional, and clinical outcomes after ACL reconstruction with the use of QT graft compared to BTB and HT grafts. However, it was not specified what type of QT graft was used. In a different study, Crum et al. [5] compared QT soft tissue to QT with bone graft, also here no difference in re-rupture rate was reported.
On performing the pull to failure tests, several methods of graft fixation were piloted including cryo-clamps. The chosen fixation devise and fixation method for the present study were consistent with the pilots that reported the highest pull to failure values. Some studies have reported both lower [4] and higher [26] pull to failure values for QT grafts than reported in this study. When using cryo-clamps, there may be a greater chance of creating a mid-substance rupture due to the freezing of the graft at the clamp site [26]. When using normal clamps as in the present study, it may simulate a more true-life setting by possibly failing at the weakest point.
One of the strengths of this study was the comparison of the many types of QT grafts directly, not only to BTB grafts, but also to a 4-SST and an isolated RF graft in the same testing mechanism. The present study did report on equivalent and also lower values for ultimate load for the tested grafts compared to the values in other studies [16, 26].
There were some limitations to this study. One limitation was the low number of grafts per group which may not allow for statistical detection of subtle group differences in biomechanical metrics. The low number of grafts in each group was due to limited availability of young donor specimens and the requirement of a large number of QT grafts in total for the study. In addition, testing on three types of QT grafts was completed: Full-thickness with and without bone and partial thickness without bone. It was planned to test all four types of QT grafts, but due to the limited availability of young specimens, the distribution of grafts was prioritized, and it was chosen to not test PT QT grafts with bone.
PT QT grafts had significantly lower ultimate load and stiffness than other potential ACL grafts, such as BTB and 4-SST, whereas the FT QT grafts with bone were comparable to BTB grafts and possessed the ultimate tensile force and stiffness needed to be a viable ACLR graft choice. Some authors have advocated for utilizing partial thickness with mini-invasive harvesting technique with the potential advantage of preserving quadriceps strength and avoiding violation of the suprapatellar pouch and potential muscle herniation [6, 27]. Furthermore, harvesting partial thickness QT is made easier by the available harvesting devices which are not currently available for full thickness QT. The current literature on clinical studies has not demonstrated superiority of full thickness QT over partial thickness QT in terms of outcomes and revision rates. Surgeon surveys regarding use of QT graft have reported that only 2% of US surgeon currently are using QT grafts for ACLR [34]. This study suggests that full thickness QT with bone block has comparable biomechanical properties to BTB and four-strand semitendinosus, and all these 3 are comparable to native ACL and should be considered viable graft for ACLR. Controlled clinical studies with direct comparison of different QT grafts are needed.
Conclusion
Full thickness QT grafts with bone had similar material properties to BTB and a 4-SST grafts, while Partial thickness QT graft without bone had significantly lower material properties than BTB and 4-SST, in a biomechanical setting.
References
Amis AA, Dawkins GP (1991) Functional anatomy of the anterior cruciate ligament. Fibre bundle actions related to ligament replacements and injuries. J Bone Joint Surg Br 73:260–267
Blauth W (1984) A new drill template for the operative treatment of injuries of the anterior cruciate ligament. Unfallheilkunde 87:463–466
Carmichael JR, Cross MJ (2009) Why bone-patella tendon-bone grafts should still be considered the gold standard for anterior cruciate ligament reconstruction. Br J Sports Med 43:323–325
Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J (2017) Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med 45:1326–1332
Crum RJ, Kay J, Lesniak BP, Getgood A, Musahl V, de Sa D (2021) Bone versus all soft tissue quadriceps tendon autografts for anterior cruciate ligament reconstruction: a systematic review. Arthroscopy 37:1040–1052
Fink C, Herbort M, Abermann E, Hoser C (2014) Minimally invasive harvest of a quadriceps tendon graft with or without a bone block. Arthrosc Tech 3:e509-513
Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS (2015) Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc 23:640–648
Geib TM, Shelton WR, Phelps RA, Clark L (2009) Anterior cruciate ligament reconstruction using quadriceps tendon autograft: intermediate-term outcome. Arthroscopy 25:1408–1414
Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC (2005) Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy 21:791–803
Han HS, Seong SC, Lee S, Lee MC (2008) Anterior cruciate ligament reconstruction: quadriceps versus patellar autograft. Clin Orthop Relat Res 466:198–204
Harris NL, Smith DA, Lamoreaux L, Purnell M (1997) Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: morphometric and biomechanical evaluation. Am J Sports Med 25:23–28
Iriuchishima T, Shirakura K, Yorifuji H, Fu FH (2012) Anatomical evaluation of the rectus femoris tendon and its related structures. Arch Orthop Trauma Surg 132:1665–1668
LaPrade MD, Kallenbach SL, Aman ZS, Moatshe G, Storaci HW, Turnbull TL et al (2018) Biomechanical evaluation of the medial stabilizers of the patella. Am J Sports Med 46:1575–1582
Lippe J, Armstrong A, Fulkerson JP (2012) Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy 28:980–984
Lockwood WC, Marchetti DC, Dahl KD, Mikula JD, Williams BT, Kheir MM et al (2017) High-load preconditioning of human soft tissue hamstring grafts: an in vitro biomechanical analysis. Knee Surg Sports Traumatol Arthrosc 25:138–143
Mabe I, Hunter S (2014) Quadriceps tendon allografts as an alternative to Achilles tendon allografts: a biomechanical comparison. Cell Tissue Bank 15:523–529
Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH (2014) Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc 22:1467–1482
Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E (2019) Anterior cruciate ligament reconstruction: a systematic review and meta-analysis of outcomes for quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring-tendon autografts. Am J Sports Med 47:3531–3540
Norwood LA, Cross MJ (1979) Anterior cruciate ligament: functional anatomy of its bundles in rotatory instabilities. Am J Sports Med 7:23–26
Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66:344–352
Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM et al (2014) Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004–2012. Am J Sports Med 42:285–291
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M (2014) Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. Am J Sports Med 42:278–284
Risberg MA, Oiestad BE, Gunderson R, Aune AK, Engebretsen L, Culvenor A et al (2016) Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med 44:1215–1224
Runer A, Wierer G, Herbst E, Hepperger C, Herbort M, Gföller P et al (2018) There is no difference between quadriceps- and hamstring tendon autografts in primary anterior cruciate ligament reconstruction: a 2-year patient-reported outcome study. Knee Surg Sports Traumatol Arthrosc 26:605–614
Schmidt EC, Chin M, Aoyama JT, Ganley TJ, Shea KG, Hast MW (2019) Mechanical and microstructural properties of pediatric anterior cruciate ligaments and autograft tendons used for reconstruction. Orthop J Sports Med 7:2325967118821667
Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J (2016) Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthroscopy 32:71–75
Sheean AJ, Musahl V, Slone HS, Xerogeanes JW, Milinkovic D, Fink C et al (2018) Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med 52:698–701
Slone HS, Romine SE, Premkumar A, Xerogeanes JW (2015) Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 31:541–554
Stäubli HU, Schatzmann L, Brunner P, Rincón L, Nolte LP (1999) Mechanical tensile properties of the quadriceps tendon and patellar ligament in young adults. Am J Sports Med 27:27–34
Stäubli HU, Schatzmann L, Brunner P, Rincón L, Nolte LP (1996) Quadriceps tendon and patellar ligament: cryosectional anatomy and structural properties in young adults. Knee Surg Sports Traumatol Arthrosc 4:100–110
Taylor KA, Cutcliffe HC, Queen RM, Utturkar GM, Spritzer CE, Garrett WE et al (2013) In vivo measurement of ACL length and relative strain during walking. J Biomech 46:478–483
Tran TD, Tran QL (2018) A cadaveric study on the anatomy of anterior cruciate ligament in Vietnamese adults. Asia Pac J Sports Med Arthrosc Rehabil Technol 14:22–25
Urchek R, Karas S (2019) Biomechanical comparison of quadriceps and 6-strand hamstring tendon grafts in anterior cruciate ligament reconstruction. Orthop J Sports Med 7:2325967119879113
van Eck CF, Schreiber VM, Mejia HA, Samuelsson K, van Dijk CN, Karlsson J et al (2010) “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 26:S2-12
Woo SL, Hollis JM, Adams DJ, Lyon RM, Takai S (1991) Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 19:217–225
Zaffagnini S, Signorelli C, Grassi A, Hoshino Y, Kuroda R, de Sa D et al (2018) Anatomic anterior cruciate ligament reconstruction using hamstring tendons restores quantitative pivot shift. Orthop J Sports Med 6:2325967118812364
Funding
This study was funded by Smith & Nephew.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Marc Strauss is a paid for educational consultant for Smith and Nephew and receives research grants from Smith and Nephew. Dr. Martin Lind is a paid for educational consultant for Smith and Nephew. Receives research grants from Smith and Nephew and is on the Editorial Boards of KSSTA and JEO. Dr. Gilbert Moatshe is a paid for educational consultant for Smith and Nephew. Dr. Lars Engebretsen is a paid for consultant for Arthrex and Smith and Nephew. Receives royalties from Arthrex, and research grants from Ossur, Biomet, and Smith and Nephew. Is on the Editorial Boards of AJSM, KSSTA and JEO. Is an editor for JBJS and BJSM. Dr. Robert LaPrade is a paid for consultant for Arthrex, Ossur, Linvatec and Smith and Nephew. Recieves royalties from Arthrex, Ossur, Elsevier and Smith and Nephew and research grants from Ossur and Smith and Nephew. Is on the Editorial Boards of AJSM, KSSTA and JEO. Authors John Miles, Grant Dornan and Mitchell declare that they have no conflicts of interest.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Strauss, M.J., Miles, J.W., Kennedy, M.L. et al. Full thickness quadriceps tendon grafts with bone had similar material properties to bone-patellar tendon-bone and a four-strand semitendinosus grafts: a biomechanical study. Knee Surg Sports Traumatol Arthrosc 30, 1786–1794 (2022). https://doi.org/10.1007/s00167-021-06738-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06738-x