Abstract
Background
Randomized, controlled trials comparing breast-conserving therapy (BCT) with mastectomy have demonstrated equivalent overall survival (OS), but recent observational studies have shown improved OS in patients undergoing BCT. These studies provide limited data on young patients who are traditionally offered mastectomy due to perceived higher disease risk. This study examines the OS in a contemporary series of young women with breast cancer undergoing upfront BCT compared with mastectomy.
Methods
Women ≤40 years old with primary invasive T1-T2, N0-N1 breast cancer were identified from the National Cancer Database between 2006 and 2016. Patient cohorts were based according to locoregional treatment: BCT, mastectomy alone (Mx), and mastectomy with radiotherapy (Mx/RT). Kaplan-Meier method followed by Cox proportional-hazards regression with inverse probability of treatment weighting (IPTW) were performed to account for treatment selection bias effects in OS.
Results
A total of 15,611 patients met the study criteria; 9,509 patients (60.9%) had BCT, 4,020 (25.8%) had Mx/RT, and 2,082 (13.3%) had Mx alone. The median follow-up was 4.6 years (interquartile range [IQR] 3.0–6.4). After IPTW-adjustment, the 5-year OS was similar for BCT (95%), Mx (95%), and Mx/RT (94%), and there was no significant difference in OS in Mx (hazard ratio [HR] = 1.16, 95% confidence interval [CI] 0.90–1.51) and Mx/RT (HR = 1.08, 95% CI 0.88–1.34) compared with BCT. Mx/RT was associated with decreased survival in patients with pT2N0 (HR = 1.78, 95% CI 1.12–2.84).
Conclusions
Among young patients with early-stage breast cancer, overall survival was equivalent regardless of surgical approach. Breast-conserving therapy remains a safe option in young women despite the clinical tendency to offer upfront mastectomy in young patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer in patients younger than 40 years old accounts for only 4% of all invasive breast cancer in the United States. In 2019, approximately 1 in 65 women developed the disease by the age of 40.1 Notably, young women are more likely to present with aggressive disease at diagnosis, with more advanced-stage, higher-grade tumors, and a higher proportion of HER2-positive and triple-negative breast cancer in comparison with patients older than aged 40 years.2,3
Previous pivotal randomized controlled trials comparing breast-conserving therapy (BCT), defined as breast-conserving surgery followed by radiation therapy, with mastectomy have consistently shown equivalent overall survival (OS).4,5,6,7,8,9 More recently, several cancer registry database analyses have challenged the survival equivalence of BCT and mastectomy, demonstrating a disease-free survival and overall survival advantage in women with both node-negative and node-positive, early-stage breast cancer treated with BCT.10,11,12,13 However, these studies lack a specific evaluation of the impact of the locoregional therapies in young patients, who are disproportionately offered mastectomy due to increased perceived risk of local recurrence. Recently, increased trends of mastectomy in patients with early-stage breast cancer have been reported, where younger women were more likely to undergo mastectomy irrespective of tumor size, without evidence of survival advantage.14
Using the National Cancer Database, we compared the overall survival rates for young women with early-stage breast cancer (T1-2, N0-1) treated with upfront BCT compared with women treated with upfront mastectomy with or without radiotherapy.
Methods
Data Source
All-female patients with invasive breast cancer from 2006 to 2016 were selected from the National Cancer Database (NCDB) breast cancer dataset, according to the International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) codes C50.0-C50.9. The NCDB contains data from more than 1500 CoC-accredited facilities that collect 70% of newly diagnosed cancer cases in the United States.15 Due to the deidentified nature of the data, this study received institutional review board exemption status after an independent regulatory review.
Study Design and Patients
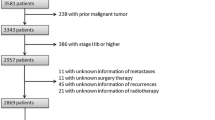
We included women aged ≤40 years with primary, invasive, unilateral, and early-stage breast cancer (i.e., T1-T2, N0-N1) who underwent upfront surgery of the primary tumor. We excluded all patients with ductal carcinoma in situ (stage 0) and clinically inoperable breast cancer (N2 disease, stage IIIB, IIIC, and stage IV).16,17 Additionally, patients were excluded if they had received neoadjuvant systemic therapies, had a history of prior cancer, or had missing survival data (Fig. 1).
Three cohorts were created according to the locoregional treatment: breast-conserving surgery followed by radiation therapy (aka, breast-conserving therapy, BCT), mastectomy alone (Mx), and mastectomy with radiotherapy (Mx/RT).
Sociodemographic characteristics included age at diagnosis, race/ethnicity, comorbidity score (Charlson/Deyo score), and type of health facility. Clinical and pathological tumor size and lymph node status were categorized and grouped in anatomic stages according to the 8th edition of the AJCC Cancer Staging Manual.18 Additional tumor features included histologic type and grade, lymphovascular invasion, hormone receptor (HR) status (i.e., estrogen receptor (ER), progesterone receptor (PgR)), and human epidermal growth factor receptor 2 (HER2) statuses. Additionally, patients were classified into four breast cancer subtypes: HR-positive/HER2-negative, HR-positive/HER2-positive, HR-negative/HER2-positive, and HR-negative/HER2-negative (aka, triple-negative breast cancer).
Statistical Analysis
Baseline characteristics were compared using chi-squared tests and ANOVA analysis or Kruskal-Wallis rank-sum test for categorical and continuous variables, respectively. Overall survival (OS) was calculated from the time of diagnosis until death or last known follow-up. To account for selection bias, univariate followed by multivariable Cox proportional-hazards regression analyses were performed. Cox proportional-hazards regression with inverse probability of treatment weighting (IPTW) using propensity score method for the comparisons of OS between study cohorts also was performed using the R/twang package.19,20 The stabilized inverse probability weights were derived from the GBM-ATE (generalized boost models with average treatment effect) predicted probabilities of treatments on age, race/ethnicity, insurance, income, education, comorbidities, facility type, city type, histologic type and grade, lymph-vascular invasion (LVI), breast cancer subtypes (based on hormone receptor and HER2 statuses), AJCC clinical and pathological stages, tumor size, lymph node status, and adjuvant systemic therapy. We assessed the balance of the covariates in the weighted samples between study cohorts using standardized mean differences. No correction was made for multiple comparisons. Trends over time in BCT versus mastectomy were compared using chi-squared tests for trend. Multivariable logistic regression also was performed to predict the likelihood of the receipt of mastectomy. All statistical tests were two-sided, and P < 0.05 was considered significant. All statistical analyses were performed in R version 3.6.3 (R Core Team, 2020).
Results
Patient Characteristics
Of the 15,611 patients who met the inclusion criteria, 9,509 patients (60.9%) underwent BCT, 4,020 (25.8%) had Mx/RT, and 2,082 (13.3%) had Mx alone (Fig. 1). There were significant differences in patient demographics and tumor features among the unadjusted cohorts (Table 1). Briefly, patients in the Mx/RT cohort more frequently had larger tumors (clinical and pathological T2) and lymph node metastatic involvement (both pN1 and pN2) than patients in BCT and Mx alone cohorts, which was reflected in more advanced pathological stage tumors (IIB: 36.1% in Mx/RT vs. 11.3% in BCT vs. 13.8% in Mx alone, P < 0.001; IIIA: 18.3% in Mx/RT vs. 2.9% in BCT vs. 1.8% in Mx alone, P < 0.001). Additionally, there were fewer low-grade tumors (grade I), more frequent lymph-vascular invasion, and HER2-positive breast cancers in the Mx/RT group. There were no significant differences among the cohorts after adjustment (Supplementary Fig. 1).
Survival Data Analysis
The median follow-up was 4.6 years (IQR 3.0–6.4). Unadjusted analyses showed that the BCT cohort was associated with an OS advantage (Fig. 2A). However, in the Kaplan-Meier survival analyses after IPTW adjustments, the OS was similar for BCT, Mx alone, and Mx/RT (5-year OS: 95%, 95%, and 94%; 7-year OS: 93%, 92%, and 92%, respectively, Fig. 2B). Additionally, in the Cox proportional-hazards regression analyses with IPTW adjustment, there was no significant difference in hazard of death in Mx (HR = 1.16, 95% CI: 0.90–1.51) and Mx/RT (HR = 1.08; 95% CI 0.88–1.34) compared to BCT (Figs. 2B and 3). Similarly, multivariable Cox proportional-hazards regression analysis showed that surgery type was not independently associated with the hazard of death (Table 2). In the subgroup analysis stratified by age categories, pathological stages, and breast cancer subtypes, there was no difference in risk of death among the groups except for Mx/RT, which was associated with an increased risk of death in patients with pathological stage T2N0 (HR = 1.78, 95% CI: 1.12–2.84, P = 0.01; Fig. 2D). Mastectomy alone was associated with an increased risk of death in patients with pathological stage IIIA, especially T2N2 (HR = 2.65, 95% CI: 1.15–6.11, P = 0.02; Fig. 2H and 3).
Overall survival by Locoregional Treatment Group. Unadjusted Kaplan-Meier curves for overall survival in all patients (A). Cox proportional-hazards regression with IPTW using propensity score method for the comparisons of overall survival in all patients (B) and pathological anatomical stages pT1N0 (C), pT2N0 (D), pT1N1 (E), pT2N1 (F), pT1N2 (H), and pT2N2 (I). IPTW inverse probability of treatment weighting; BCT breast-conserving therapy; Mx mastectomy; RT radiotherapy
Mortality hazard ratios compared to BCT in all patients and subgroup analysis after IPTW adjustment. Forest plot showing the comparison of overall survival among surgery types, taking BCT as a reference using Cox proportional-hazards regression with IPTW for all patients as well as subgroups stratified by age categories, pathological anatomical AJCC stages, and breast cancer subtypes. The stabilized inverse probability weights were derived from the GBM-ATE (average treatment effect) predicted probabilities on age, race/ethnicity, insurance, income, education, comorbidities, facility type, city type, histologic type and grade, lymph-vascular invasion, breast cancer subtypes, AJCC clinical and pathological stages, tumor size, lymph node status, and adjuvant endocrine therapy, adjuvant chemotherapy, and adjuvant targeted therapy. IPTW inverse probability of treatment weighting; HR hazard ratio, BCT breast-conserving therapy; Mx mastectomy; RT radiotherapy
Trends in Treatments and Predictors of Mastectomy
Due to the lack of robust data from 2006 to 2009, we focused our trend analysis from 2010 to 2016. Breast-conserving therapy decreased over the study period from 67.4% in 2010 to 57.2% in 2016 (P < 0.001). Conversely, mastectomy followed by radiotherapy and mastectomy alone increased from 20.1 to 27.3%, and 12.5 to 15.5%, respectively (Supplementary Fig. 2). Logistic regression analysis identified multiple predictors for receipt of mastectomy (Supplementary Table 1). After controlling for competing factors in the multivariable analysis, the odds of receiving mastectomy were significantly higher for patients with clinical stage IIB (odds ratio [OR]: 3.86, 95% CI: 3.43–4.34, P < 0.001), the presence of LVI (OR: 2.20, 95% CI: 2.04–2.38, P < 0.001), lobular histology (OR: 2.02, 95% CI: 1.64–2.49, P < 0.001), and HR-negative/HER2-positive tumors, but significantly lower for African-American women (OR: 0.78, 95% CI: 0.70–0.86, P < 0.001) or triple-negative breast cancer (OR: 0.76, 95% CI: 0.68–0.86, P < 0.001).
Discussion
This study evaluated differences in the overall survival in young patients with early-stage breast cancer based on the locoregional treatment. After adjustment for all confounding factors, including clinical-demographic characteristics, tumor-pathological features, and systemic adjuvant therapies, survival rates were equivalent in young patients undergoing breast-conserving therapy or mastectomy. Additionally, when the multivariable analysis was performed, the type of surgery was not an independent factor of survival.
The most appropriate method to evaluate the clinical outcomes between therapeutic approaches is within the setting of randomized, control trials (RCTs). However, this comparison has not been made in young patients, and it is unlikely to occur. Six pivotal RCTs, including mostly older patients, have demonstrated equivalent OS for breast-conserving therapy and mastectomy.4,5,6,7,8,9 Considering the time of patient enrollment (from 1972 to 1989) in these studies and significant improvements in surgical and adjuvant therapies in recent decades, it is rational to assume that there would be changes in survival. More recent, large, population-based studies have reported improved survival outcomes with BCT compared with mastectomy patients.10,12,13 Several Surveillance, Epidemiology, and End Results (SEER) database and NCDB analyses have documented an association with improved breast cancer-specific and overall survival in women treated with BCT with both stages I and II breast cancer regardless of the lymph node status,10,21 and in patients with triple-negative breast cancer.22,23 Additionally, studies from the Netherlands Cancer Registry and the Swedish National Breast Cancer Register reported an association with improved OS in patients with early breast cancer treated with BCT compared to mastectomy.12,13 In these observational studies, the survival advantage in favor of BCT was more robust in patients older than 50 years, with more advanced disease, or triple-negative breast cancer. In the largest observational study, which included more than 800,000 patients from NCDB, patients who underwent mastectomy were not associated with increased mortality compared with those undergoing BCT.24 In our study, which was restricted to patients aged 40 years or younger from NCDB, the overall survival was equivalent between the cohorts, supporting the existing literature that surgery type does not impact survival.
Several studies have identified young age as an independent predictor of ipsilateral in-breast recurrences after BCT compared with older counterparts.25,26 This may be one of the concerning factors associated with increased rates of unilateral and bilateral mastectomies in younger patients, without a demonstrated survival advantage.14,27 A meta-analysis, including women aged 40 years or younger from five population-based studies, T1-T2 invasive breast cancer, found no overall difference in survival between BCT and mastectomy (HR = 0.88, 95% CI: 0.78–1.01). The studies included in this meta-analysis enrolled 22,398 patients from 1980 to 2007.28 More recently, the Prospective study of Outcomes in Sporadic versus Hereditary Breast Cancer (POSH), a large observational cohort study, included 3,024 women aged 18 to 40 years between 2000 to 2008. In the multivariable analysis, there was no significant difference in OS between BCT and mastectomy (HR = 0.79, 95% CI: 0.61–1.03).29 This is consistent with our study, which focused on a more contemporary series (from 2006 to 2016) and found no differences in OS between the different locoregional approaches.
Patients with pT2N0 disease who underwent mastectomy are usually not candidates for radiation therapy. However, postmastectomy radiotherapy may be considered in patients with high-risk recurrence factors, such as grade 3, estrogen-receptor (ER) negative, or the presence of lymph-vascular invasion.17 In our study, patients with pT2N0 disease within the Mx/RT cohort more frequently had LVI (30% vs. 15–20% in the other cohorts, P < 0.001), without significant differences in other pathologic parameters (Supplementary Table 2). These variables were controlled in our propensity score model. We found that postmastectomy radiation therapy (PMRT) was associated with an increased likelihood of death in patients with pT2N0 compared with BCT (HR = 1.78, 95% CI: 1.12–2.84). de Boniface et al. reported similar findings in older patients, suggesting that more extensive surgeries with radiotherapy do not appear to reduce mortality, but increase the risk of death.13 The need for PMRT was addressed by the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) meta-analysis, using individual data from 22 trials, comparing mastectomy with axillary surgery with or without PMRT (N = 8,135 patients). Women with lymph node-negative disease who underwent PMRT had an absolute increase in overall mortality of 6% at 20 years compared to patients without PMRT (relative risk [RR] = 1.23, 95% CI 1.02–1.49).30 These findings suggest that the absolute benefit of PMRT may be outweighed by its potential toxicities in patients with negative lymph nodes.
Regarding node-positive disease, we found no significant difference in hazard of death in patients with 1–3 positive lymph nodes regardless of surgical approach, reflecting that lesser breast surgery does not change the survival. EBCTCG meta-analysis reported no differences in 20-year all-cause mortality in patients who underwent mastectomy with or without PMRT.30 By contrast, we observed that the lack of radiotherapy (i.e., mastectomy alone) was associated with worse outcomes in patients with larger tumors and high tumor burden in the axilla (i.e., T2N2), reflecting that mastectomy alone is insufficient treatment and increases the risk of mortality (HR = 2.65, 95% CI: 1.15–6.11) compared with those undergoing BCT or Mx/RT. The EBCTCG meta-analysis also revealed that PMRT had a significant absolute reduction of 7.6% in the 20-year all-cause mortality in patients with four or more positive lymph nodes.30
There are conflicting data regarding the appropriate locoregional management of patients according to the breast cancer subtype. For example, triple-negative breast cancer (TNBC) is usually associated with younger age at presentation, BRCA1 mutations, and carries an elevated risk of locoregional recurrences (LRR) after both BCT and mastectomy compared with luminal subtypes.31 Several retrospective institutional and SEER database analyses demonstrated similar or superior overall survival outcomes favoring BCT vs. mastectomy (with or without radiotherapy) in older patients with stage I-II TNBC.22,23,32,33 In our study, which was limited to T1-T2 tumors in younger women, there was no statistical difference in overall survival in TNBC patients who underwent Mx/RT compared with BCT (HR = 1.41, 95% CI: 0.99–2.02, P = 0.06). Similarly, a large NCDB study comparing mastectomy with or without radiotherapy in patients with nonmetastatic TNBC found no overall survival benefit in patients with T1-T2N0.34 Altogether, these findings support the notion that the locoregional option should not be guided only by the TNBC subtype, and the indication of Mx/RT should consider other risk factors, such as LVI or grade, as has been suggested in a recent consensus guideline.35
Age has been postulated as a significant factor related to the increase in mastectomy rates. Some studies have shown that younger than 40 years of age is a significant predictor of mastectomy choice over BCT.36,37 In our study, we observed that breast-conserving therapy decreased by 10.2%, and Mx-RT and Mx alone increased by 7.2% and 3%, respectively, from 2010 to 2016. Several clinicopathological factors have been associated with the surgical choice. Our findings align with several other studies showing an increased likelihood of mastectomy in patients with increasing clinical-stage, lobular histology, and the presence of LVI.38,39 Other factors interplay in the complexity of the decision-making of the surgical choice. Regardless of age, women often choose mastectomy for fear of recurrence and a perceived survival benefit.40 Additional factors to consider are increased hereditary risk—especially in younger patients, preoperative MRI, advances in oncoplastic and reconstruction options influencing surgeon preferences, race, education, comorbidities, tumor location, and feasibility of postoperative RT.41,42
Our retrospective observational study was inherently limited by nonrandomized data and limited variables available in the NCDB. Therefore, causality can not be inferred and the main obstacles to estimate differences among the therapeutical cohorts lean on the confounding variables. To minimize the selection bias, significant baseline differences among the three cohorts necessitated the adjustment of confounders using propensity score methods.19,20 The equivalent survival among the cohorts was similar in the propensity score model and the Cox-multivariable analysis, suggesting that this equivalence is not biased by the model. Unfortunately, the NCDB provides no information on ipsilateral breast recurrences or breast cancer-specific mortality, limiting the analysis to overall survival as the only clinical outcome evaluated. Furthermore, NCDB does not account for other factors that may influence the surgical decision, such as germline mutation (e.g., BRCA1/2 status), multifocality/multicentricity, invasive carcinoma with extensive in situ component, or patient and physician preferences. NCDB lacks granular information regarding adjuvant systemic regimens (chemo/endocrine) and adherence to therapy over time, which also may influence survival. Finally, to evaluate accurately the surgical impact, we excluded patients receiving neoadjuvant therapy. This may have introduced a selection bias by excluding higher-risk patients. Therefore, further studies in young patients with HER2-positive or triple-negative breast cancer who are candidates for neoadjuvant therapy should be performed.
Conclusions
The results of our study support the use of breast-conserving therapy as the preferred option whenever suitable in young patients with breast cancer. Despite the clinical tendency to offer mastectomy in young patients, breast-conserving therapy remains a safe option in young women. The recommendation for mastectomy as the primary surgical option should not be based on young age alone.
References
DeSantis CE, Ma J, Gaudet MM, et al. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69(6):438–51.
Partridge AH, Hughes ME, Warner ET, et al. Subtype-Dependent Relationship Between Young Age at Diagnosis and Breast Cancer Survival. J Clin Oncol. 2016;34(27):3308–14.
Kim HJ, Kim S, Freedman RA, Partridge AH. The impact of young age at diagnosis (age <40 years) on prognosis varies by breast cancer subtype: A U.S. SEER database analysis. Breast. 2021;61:77-83.
Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347(16):1233–41.
Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347(16):1227–32.
Arriagada R, Le MG, Guinebretiere JM, Dunant A, Rochard F, Tursz T. Late local recurrences in a randomised trial comparing conservative treatment with total mastectomy in early breast cancer patients. Ann Oncol. 2003;14(11):1617–22.
Poggi MM, Danforth DN, Sciuto LC, et al. Eighteen-year results in the treatment of early breast carcinoma with mastectomy versus breast conservation therapy: the National Cancer Institute Randomized Trial. Cancer. 2003;98(4):697–702.
Blichert-Toft M, Nielsen M, During M, et al. Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol. 2008;47(4):672-81.
Litiere S, Werutsky G, Fentiman IS, et al. Breast conserving therapy versus mastectomy for stage I-II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial. Lancet Oncol. 2012;13(4):412–9.
Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J. Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg. 2014;149(3):267–74.
Hartmann-Johnsen OJ, Kåresen R, Schlichting E, Nygård JF. Survival is Better After Breast Conserving Therapy than Mastectomy for Early Stage Breast Cancer: A Registry-Based Follow-up Study of Norwegian Women Primary Operated Between 1998 and 2008. Ann Surg Oncol. 2015;22(12):3836–45.
van Maaren MC, de Munck L, de Bock GH, et al. 10 year survival after breast-conserving surgery plus radiotherapy compared with mastectomy in early breast cancer in the Netherlands: a population-based study. Lancet Oncol. 2016;17(8):1158–70.
de Boniface J, Szulkin R, Johansson ALV. Survival After Breast Conservation vs Mastectomy Adjusted for Comorbidity and Socioeconomic Status: A Swedish National 6-Year Follow-up of 48 986 Women. JAMA Surg. 2021;156(7):628–37.
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide trends in mastectomy for early-stage breast cancer. JAMA Surg. 2015;150(1):9–16.
Bilimoria KY, Stewart AK, Winchester DP, Ko CY. The National Cancer Data Base: a powerful initiative to improve cancer care in the United States. Ann Surg Oncol. 2008;15(3):683–90.
Chia S, Swain SM, Byrd DR, Mankoff DA. Locally advanced and inflammatory breast cancer. J Clin Oncol. 2008;26(5):786–90.
National Comprehensive Cancer Network. Breast Cancer (Version 3.2022). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed May 18, 2022.
Giuliano AE, Connolly JL, Edge SB, et al. Breast Cancer-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(4):290-303.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79.
Austin PC. Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis. Stat Med. 2016;35(30):5642–55.
Almahariq MF, Quinn TJ, Siddiqui Z, et al. Breast conserving therapy is associated with improved overall survival compared to mastectomy in early-stage, lymph node-negative breast cancer. Radiother Oncol. 2020;142:186–94.
Chen QX, Wang XX, Lin PY, et al. The different outcomes between breast-conserving surgery and mastectomy in triple-negative breast cancer: a population-based study from the SEER 18 database. Oncotarget. 2017;8(3):4773–80.
Saifi O, Chahrour MA, Li Z, et al. Is breast conservation superior to mastectomy in early stage triple negative breast cancer? Breast. 2022;62:144–51.
Landercasper J, Ramirez LD, Borgert AJ, et al. A Reappraisal of the Comparative Effectiveness of Lumpectomy Versus Mastectomy on Breast Cancer Survival: A Propensity Score-Matched Update From the National Cancer Data Base (NCDB). Clin Breast Cancer. 2019;19(3):e481–93.
Botteri E, Bagnardi V, Rotmensz N, et al. Analysis of local and regional recurrences in breast cancer after conservative surgery. Ann Oncol. 2010;21(4):723–8.
Wapnir IL, Anderson SJ, Mamounas EP, et al. Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in five National Surgical Adjuvant Breast and Bowel Project node-positive adjuvant breast cancer trials. J Clin Oncol. 2006;24(13):2028–37.
Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M. Growing Use of Contralateral Prophylactic Mastectomy Despite no Improvement in Long-term Survival for Invasive Breast Cancer. Ann Surg. 2017;265(3):581–9.
Vila J, Gandini S, Gentilini O. Overall survival according to type of surgery in young (≤40 years) early breast cancer patients: A systematic meta-analysis comparing breast-conserving surgery versus mastectomy. Breast. 2015;24(3):175–81.
Maishman T, Cutress RI, Hernandez A, et al. Local Recurrence and Breast Oncological Surgery in Young Women With Breast Cancer: The POSH Observational Cohort Study. Ann Surg. 2017;266(1):165–72.
McGale P, Taylor C, Correa C, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014;383(9935):2127–35.
Moran MS. Should triple-negative breast cancer (TNBC) subtype affect local-regional therapy decision making? Am Soc Clin Oncol Educ Book. 2014:e32-6.
Adkins FC, Gonzalez-Angulo AM, Lei X, et al. Triple-negative breast cancer is not a contraindication for breast conservation. Ann Surg Oncol. 2011;18(11):3164–73.
Zumsteg ZS, Morrow M, Arnold B, et al. Breast-conserving therapy achieves locoregional outcomes comparable to mastectomy in women with T1–2N0 triple-negative breast cancer. Ann Surg Oncol. 2013;20(11):3469–76.
Haque W, Verma V, Farach A, Brian Butler E, Teh BS. Postmastectomy radiation therapy for triple negative, node-negative breast cancer. Radiother Oncol. 2019;132:48–54.
Elghazaly H, Rugo HS, Azim HA, et al. Breast-Gynaecological & Immuno-Oncology International Cancer Conference (BGICC) Consensus and Recommendations for the Management of Triple-Negative Breast Cancer. Cancers (Basel). 2021;13(9).
Hiotis K, Ye W, Sposto R, Skinner KA. Predictors of breast conservation therapy: size is not all that matters. Cancer. 2005;103(5):892–9.
McGuire KP, Santillan AA, Kaur P, et al. Are mastectomies on the rise? A 13-year trend analysis of the selection of mastectomy versus breast conservation therapy in 5865 patients. Ann Surg Oncol. 2009;16(10):2682–90.
Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States? J Clin Oncol. 2010;28(21):3437–41.
Lautner M, Lin H, Shen Y, et al. Disparities in the Use of Breast-Conserving Therapy Among Patients With Early-Stage Breast Cancer. JAMA Surg. 2015;150(8):778–86.
Fisher CS, Martin-Dunlap T, Ruppel MB, Gao F, Atkins J, Margenthaler JA. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast-conservation therapy regardless of age. Ann Surg Oncol. 2012;19(10):3246–50.
Tan MP. Is there an Ideal Breast Conservation Rate for the Treatment of Breast Cancer? Ann Surg Oncol. 2016;23(9):2825–31.
Gu J, Groot G, Boden C, Busch A, Holtslander L, Lim H. Review of Factors Influencing Women’s Choice of Mastectomy Versus Breast Conserving Therapy in Early Stage Breast Cancer: A Systematic Review. Clin Breast Cancer. 2018;18(4):e539–54.
Acknowledgment
This study was supported by the Associates for Breast and Prostate Cancer Studies (ABCs) foundation and the Fashion Footwear Association of New York (FFANY) foundation.
Disclosures
The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the sources of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors. The authors have no conflict of interest disclosures to report.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Orozco, J.I.J., Keller, J.K., Chang, SC. et al. Impact of Locoregional Treatment on Survival in Young Patients with Early-Stage Breast Cancer undergoing Upfront Surgery. Ann Surg Oncol 29, 6299–6310 (2022). https://doi.org/10.1245/s10434-022-12190-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12190-z