Abstract
This study aims to assess survival rates in early breast cancer patients treated by conservative breast therapy (CBT), including radiotherapy, compared with those treated by modified radical mastectomy (MRM) alone. The South Egypt Cancer Institute and the Assiut University Oncology Department patients’ records, from January 2010 to December 2017, were searched for T1-2N0-1M0 breast cancer patients treated by CBT or MRM. Patients who did not receive chemotherapy were excluded to reduce the treatment variation. The 5-year locoregional disease-free survival (LRDFS) was 97.3% for the CBT patients was and 98.0% for the MRM patients (P = .675). The 5-year distant disease-free survival (DDFS) was 93.6% for CBS and 85.7% for MRM (P = 0.033). The DFS was 91.9% for the BCT patients and 85.3% for the MRM patients (P = 0.045). The 5-year OS was 98.2% for the CBT patients and 94.3% for the MRM patients, (P = 0.02). By Cox regression analysis, the CBT resulted in significantly better OS, (P = 0.018) and the HR = 0.350, 95% CI 0.146–0.837. The adjusted OS, estimated by the propensity score-based weights, remained superior in CBT than in MRM patients (P < 0.001). CBT resulted in better DDFS, DFS, and OS than MRM. Future randomized trials are needed to confirm these findings and determine the cause.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer remains the most frequently diagnosed cancer worldwide and is the leading cause of cancer-related death in women [1]. Randomized trials have documented breast-conserving therapy (BCT) to be equivalent to mastectomy with respect to survival as primary breast local treatment for women with stage I and stage II breast cancers [2,3,4,5,6], even with long-term follow-up. Over the past few decades since these trials were conducted, substantial changes in breast cancer detection and treatment have occurred, including in the precision of radiotherapy and the decline of its side effects, as well as changes in its indications, but no major randomized trials have compared the two treatment modalities recently [7].
Several recent retrospective studies, however, have reported improved survival, [7,8,9], with BCT compared with mastectomy. Among the largest is a study conducted on more than 130,000 patients from the Surveillance, Epidemiology, and End Results (SEER) database. This study showed superior 5-year and 10-year overall survival with BCT. The authors recommended that the cause should be researched further since the database lacked information including the administration of adjuvant therapy other than radiation [7]. Another American study on more than 112,000 breast cancer patients supports these findings [8], but similarly, this study did not report information on chemotherapy. In a Norwegian study [9] conducted on more than 13,000 women, BCT was similarly concluded to be superior to mastectomy. The authors also recommended more studies to determine whether this benefit is caused by variation in the adjuvant systemic therapy as it was among the missing data.
Because these databases lacked some essential information, such as if chemotherapy has been administered, research is needed to assess if chemotherapy was among the factors causing these survival differences. One possible cause is the radiation therapy given as a part of BCT. We conducted this retrospective study to assess survival differences among the patients treated primarily with MRM alone or BCT with radiation therapy, followed by chemotherapy and hormonal therapy for hormonal positive cancers, to avoid survival differences due to chemotherapy.
Patients and Methods
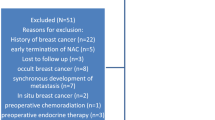
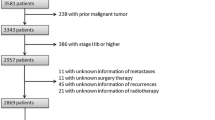
The study proposal was approved by the Ethical Committee of the South Egypt Cancer Institute and the Assiut University Ethical committee. The patients’ files in the South Egypt Cancer Institute and the Assiut Clinical Oncology Department were searched for patients between January 2010 and December 2017. Included patients were female breast cancer patients with pathological stages T1-2N0-1M0. The patients were divided into two groups, those who were treated primarily by conservative breast surgery (CBS) and adjuvant radiotherapy or modified radical mastectomy (MRM) alone. All histological types were eligible. We excluded patients who did not receive chemotherapy.
Adjuvant radiotherapy schedules included in the study were either a conventional or a hypofractionated schedule. The conventional schedule consisted of 50 Gy to the whole breast over 5 weeks, followed by a 12 Gy electron boost to the lumpectomy site in 2 Gy fractions, while in the accelerated schedule, the whole breast received 42.5 Gy in 16 fractions of 2.66 Gy each, and the lumpectomy site received a 12 Gy electron boost divided in 16 fractions of 0.75 Gy each over 3.2 weeks. Adjuvant chemotherapy regimens included were all anthracycline-based with or without taxanes and with Trastuzumab for HER2-positive patients. Hormonal positive cases received adjuvant tamoxifen and or aromatase inhibitors.
Statistical Analysis
Univariate analysis was performed using the Pearson’s chi-square test to compare patient and tumor characteristics in the CBT patients and the MRM patients. The Kaplan-Meier method was used to assess the survival of the two groups, and the results were compared by the Log-rank test. The Cox regression survival multivariable analysis was done to find the independent variables affecting the OS. Weighting by the inverse probability of treatment (IPT) generated from a propensity score was then performed, adjusting for age, menopausal status, pathology, T stage, N stage, grade, ER, PR, and HER2 status. The weighted data was used to estimate OS and in Cox regression tests. Differences were considered statistically significant at P < 0.05. Statistical Package for the Social Sciences (SPSS) version 22 was used for data processing.
Results
This study included 434 early breast cancer patients, of whom 254 patients were treated by CBS and 180 patients were treated by MRM. Table 1 shows patient and tumor characteristics. There were significant differences in the patients’ ages, menopausal status, and N stage among the two groups. In the MRM, 65.6% patient group were under the age of 50, while only 36.2% of the CBT were below 50 years of age. The premenopausal status was higher in the MRM, being 65.6% and 37.8% in the CBT group. The N stage was one in 45.7% of the CBS and 37.2% in the MRM group. None of the other compared factors differed significantly among the two groups.
The 5-year locoregional disease-free survival (LRDFS) was 97.3% for the CBT patients and 98.0% for the MRM patients, and there was no statistical significance, Fig. 1 (P = .675). The 5-year distant disease-free survival (DDFS) was 93.6% for CBS and 85.7% for MRM, Fig. 2 (P = 0.033). The combined DFS was 91.9% for the BCT patients and 85.3% for the MRM patients, Fig. 3 (P = 0.045).
The 5-year overall survival (OS) was 96.6% for all the patients. It was 98.2% for the CBT patients and 94.3% for the MRM patients, Fig. 4 (P = 0.02). Factors which may affect the survival of the whole group are shown in Table 2. Other than the type of surgery, factors which showed a significant effect on survival were T stage, the clinical nodal stage, and the progesterone receptor status. By Cox multivariable analysis, the only significant factor for OS was the type of surgery with, (P = 0.018) and the HR = 0.350, 95% CI 0.146–0.837 for CBT.
The adjusted OS, estimated by the propensity score-based weights, was still significantly better in CBT patients than in MRM patients, (P < .001). By Cox regression analysis of the weighted data, P < 0.001, HR was 0.189 for CI = 0.076–0.471.
Discussion
Conservative breast surgery with radiotherapy has been recently gaining interest as a possible superior choice to mastectomy alone as it may lead to better survival. This finding has been recently repeatedly proven, from large retrospective studies [7,8,9]. They all lacked information about whether chemotherapy has been given to the patients, which may affect survival. An important difference, in our study, is that all the included patients received chemotherapy to exclude it as a possible cause of a difference in survival. Despite this, the CBT patients had significantly superior DDFS, DFS, and OS.
The 5-year locoregional disease-free survival, in the current study, was 97.3% for the CBT patients and 98.0% for the MRM patients, which was not a statistically significant difference. Similarly, there were no significant differences between CBT and mastectomy in local or regional recurrence found in several previous studies [10,11,12]. However, the 5-year DDFS and cumulative DFS were significantly better in the patients who underwent CBT (P < 0.05). A recent study [13] comparing survival rates with CBT and mastectomy in early breast cancer also reported significantly better 6-year DDFS and cumulative DFS (P < 0.05) with CBT.
The 5-year overall survival (OS) was 96.6% for all the patients involved in this study. There was a statistically significant difference between the OS of the CBT patients and the MRM patients, being 98.2% and 94.3% respectively (P < 0.05). Similarly, CBT resulted in significantly better breast cancer-specific survival compared with mastectomy alone or mastectomy with radiation in a study reporting the survival of patients from the SEER database [7]. The mastectomy with radiation patients was only 3.4% of the studied patients, and worse survival is excepted in this group, as they probably had more risk factors to receive post-mastectomy radiotherapy (PMRT). The 5-year breast cancer–specific survival rates of the patients who underwent BCT and a mastectomy alone were 97% and 94% respectively (P < 0.001), which was comparable with the OS of our patients. The adjusted data using a propensity score maintained a survival advantage (P < 0.001), as did our data. The authors concluded that further research is warranted since there was some missing information in this database including if chemotherapy had been given. In the current study, chemotherapy was given to all the patients, and is thus established not to be the cause of the variation in our patients.
Our findings are also similar to those of Hwang et al. [8], who showed a lower hazard of death with BCT, as we did. In their analysis, stage I or II breast cancer, during the period from 1990 to 2004, was included. They concluded that unaccounted variables representing tumor aggressiveness, such as lymphovascular invasion or extranodal extension, were unlikely to have caused such a significant survival difference between the CBT and mastectomy groups. Whether there was chemotherapy administered was also not known in their study, contrary to our study.
Similar results were reported from other studies [9, 14,15,16]. Again, these studies all lacked information about the systemic treatment. In our patients, the chemotherapy was similar in the two groups and the survival advantage was sustained, so the survival difference, in our patients, is due to another cause.
An observational study based on hospital registries in India showed significantly decreased survival with MRM when compared with BCS. Its comparison was performed stage by stage. The differences in survival between MRM and BCS were significant. The difference was 8.2% for patients with stage II disease and 18.1% for patients with stage III disease [17].
Conflicting results have been reported regarding radiation therapy being the reason for the significantly better survival associated with CBT versus mastectomy. A large population based study, in the Netherlands, including more than 129,000 breast cancer patients, reported the radiation therapy in CBT to be the cause of improved survival [18]. Similarly, Ontilio et al. concluded that the survival advantage they found in 5335 breast cancer patients treated by CBT was probably due to radiation therapy and not the extent of the surgery [19]. Contrarily, in a Danish study which included more than 58,000 breast cancer patients, it was concluded that diversities in RT did not seem to explain survival difference after BCS and mastectomy [20].
A possible explanation for the contradictory reports, regarding radiotherapy causing the survival difference, is that the indications for post-mastectomy radiotherapy (PMRT) have been changing over the time of all of these studies. For instance, many women who received mastectomy only as primary treatment, despite of having one to three positive lymph nodes, would now have PMRT as evidence has emerged and it is no longer optional not to give PMRT in this group of patients [21]. The results of EBCTCG meta-analyses show that radiotherapy after mastectomy and axillary node dissection reduced both recurrence and breast cancer mortality in the women with 1 to 3 positive lymph nodes, even when systemic therapy was administered [3]. Based on these studies, it is currently recommended that PMRT be given in women with positive axillary lymph nodes. These novel findings may explain why patients treated with CBT in the era where three-dimensional radiotherapy causes less complications often has better survival than those treated by mastectomy only while having up to three positive lymph nodes.
In conclusion, CBT resulted in better 5-year DDFS, DFS, and OS than MRM. The 5-year OS for these breast cancer patients was 98.2% for the CBT group and 94.3% for the MRM group, and this was statistically significant. After adjusting the data by weights generated from a propensity score, OS was still better for the CBT patients. Future randomized clinical trials may confirm that CBT gives superior overall survival compared with mastectomy in early breast cancer and to find the cause.
References
Mohammad H, Forouzanfar KJF, Delossantos AM, Lozano R, Lopez AD, Murray CJL, Naghavi M (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: a systematicanalysis. TheLancet 6736:61351–61352
Arriagada R, Le MG, Rochard F, Contesso G (1996) Conservative treatment versus mastectomy in early breast cancer: patterns of failure with 15 years of follow-up data. Institut Gustave-Roussy Breast Cancer Group. J Clin Oncol 14:1558–1564 Available at:
Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Darby S, Mcgale P et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 378(9804):1707–1716. https://doi.org/10.1016/S0140-6736(11)61629-2
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V, Godwin J, Gray R, Hicks C, James S, MacKinnon E, McGale P, McHugh T, Peto R, Taylor C, Wang Y, Early Breast Cancer Trialists' Collaborative Group (EBCTCG) (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366:2087–2106
Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R, Luini A, Aguilar M, Marubini E (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347:1227–1232
Fisher B, Anderson S, Bryant J, Margolese RG, Deutsch M, Fisher ER, Jeong JH, Wolmark N (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241
Agarwal S, Pappas L, Neumayer L, Kokeny K, Agarwal J (2014) Effect of breast conservation therapy vs mastectomy on disease-specific survival for early-stage breast cancer. JAMA Surg 149:267–274
Hwang ES, Lichtensztajn DY, Gomez SL, Fowble B, Clarke CA (2013) Survival after lumpectomy and mastectomy for early stage invasive breast cancer: the effect of age and hormone receptor status. Cancer 119:1402–1411
Hartmann-Johnsen OJ, Karesen R, Schlichting E, Nygard JF (2015) Survival is better after breast conserving therapy than mastectomy for early stage breast cancer: a registry-based follow-up study of Norwegian women primary operated between 1998 and 2008. Ann Surg Oncol 22:3836–3845
Zhou X, Li Y (2016) Local recurrence after breast-conserving surgery and mastectomy following neoadjuvant chemotherapy for locally advanced breast cancer - a meta-analysis. Breast Care (Basel) 11(5):345–351
Chen D, Lai L, Duan C, Yan M, Xing M, Chen J, Zhang F (2014) Conservative surgery plus axillary radiotherapy vs. modified radical mastectomy in patients with stage i breast cancer. Clin Breast Cancer 14(1):e10–e13
Maishman T, Cutress RI, Hernandez A et al (2016) Local recurrence and breast oncological surgery in young women with breast cancer: the POSH observational cohort study. Ann Surg 266(1):165–172
Wang L, Ouyang T, Wang T, Xie Y, Fan Z, Lin B, Li J (2015) Breast-conserving therapy and modified radical mastectomy for primary breast carcinoma: a matched comparative study. Chin J Cancer Res 27(6):545–552. https://doi.org/10.3978/j.issn.1000-9604.2015.11.02
Fisher S, Gao H, Yasui Y, Dabbs K, Winget M (2015) Survival in stage I-III breast cancer patients by surgical treatment in a publicly funded health care system. Ann Oncol 26:1161–1169
Chen K, Liu J, Zhu L, Su F, Song E, Jacobs LK (2015) Comparative effectiveness study of breast-conserving surgery and mastectomy in the general popula- tion: a NCDB analysis. Oncotarget. 6:40127–40140
Hofvind S, Holen Å, Aas T, Roman M, Sebuødegård S, Akslen LA (2015) Women treated with breast con- serving surgery do better than those with mastectomy independ- ent of detection mode, prognostic and predictive tumor characteristics. Eur J Surg Oncol 41:1417–1422
Nandakumar A, Rath GK, Kataki AC et al (2016) Decreased survival with mastectomy vis-à-vis breast-conserving surgery in stage II and III breast cancers: a comparative treatment effectiveness study. J Glob Oncol 3(4):304–313. Published 2016 Oct 12. https://doi.org/10.1200/JGO.2016.004614
Lagendijk M, van Maaren MC, Saadatmand S et al (2017) Breast con- serving therapy and mastectomy revisited: breast cancer-specific survival and the influence of prognostic factors in 129,692 patients. Int J Cancer 142:165–175
Onitilo AA, Engel JM, Stankowski RV, Doi SAR (2015) Survival comparisons for breast conserving surgery and mastectomy revisited: community experience and the role of radiation therapy. Clin Med Res 13:65–73
Christiansen P, Carstensen SL, Ejlertsen B, Kroman N, Offersen B, Bodilsen A et al (2017) Breast conserving surgery ver- sus mastectomy: overall and relative survival—a population based study by the Danish Breast Cancer Cooperative Group (DBCG). Acta Oncol (Madr) 57:19–25
Poortmans PM, Collette S, Kirkove C, van Limbergen E, Budach V, Struikmans H, Collette L, Fourquet A, Maingon P, Valli M, de Winter K, Marnitz S, Barillot I, Scandolaro L, Vonk E, Rodenhuis C, Marsiglia H, Weidner N, van Tienhoven G, Glanzmann C, Kuten A, Arriagada R, Bartelink H, van den Bogaert W, EORTC Radiation Oncology and Breast Cancer Groups (2015) Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med 373:317–327
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sayed, M.M., Mohamed, D.O., Hassan, M.S.F. et al. Is Survival with Conservative Breast Therapy Becoming Superior to That with Modified Radical Mastectomy Alone for the Treatment of Early Breast Cancer in This Era?. Indian J Surg Oncol 14, 243–248 (2023). https://doi.org/10.1007/s13193-020-01188-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-020-01188-2