Abstract
The purpose of this study was to present a novel and simple drug deposition method to evaluate drug transport of aerosol microparticles across airway epithelial cells. Microparticles containing ciprofloxacin HCl (Cip) and doxycycline (Dox), alone or in a 50:50% w/w ratio, were spray dried and suspended using 2H, 3H-perfluoropentane, model propellant. The suspension was then used to assess deposition, and transport of these drug microparticles across sub-bronchial epithelial Calu-3 cells was also studied. In comparison with other methods of depositing microparticles, this proposed method, using drug suspended in HPFP, provides control over the amount of drugs applied on the surface of the cells. Therefore, cell permeability studies could be conducted with considerably smaller and more reproducible doses, without the physicochemical characteristics of the drugs being compromised or the use of modified pharmacopeia impactors. The suspension of microparticles in HPFP as presented in this study has provided a non-toxic, simple, and reproducible novel method to deliver and study the permeability of specific quantity of drugs across respiratory epithelial cells in vitro.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Over the last decade, the pulmonary route of drug administration has received significant attention by scientists and the pharmaceutical industry. Subsequently, there has been a large number of medicinal aerosol formulations commercialized, with many new formulations and molecules still in the development phase. This interest has resulted in a trend towards the development of improved in vitro methods and models that allow the investigation of the respiratory epithelial permeability to inhalable drug formulations (1,2,3,4,5,6).
Understanding the epithelial permeability of an aerosol formulation is important for predicting therapeutic effectiveness and pharmacokinetics of the active drug. For a short-acting β2-agonist, such as salbutamol sulfate, fast transport across the epithelial barrier resulting in the delivery of the drug to the site of action (β2-agonist receptors being present on the underlying smooth muscle) is desirable, while, for instance, for an antibiotic, used to treat localized respiratory infection, such as tobramycin, increased residence time in the airways may be more favorable (to ensure sustained minimum inhibitory concentrations).
Several approaches have been developed to study the permeability of aerosol particles in vitro. Until the last decade, most approaches utilized liquid-covered epithelia models and studied the permeability of either solutions or suspensions of drug in media, transported from the apical to basolateral compartments of Transwell-based cell cultures (7,8,9,10). However, the major drawback of this method is that the solid-state properties of the formulation are not taken into consideration as parameters affecting cell permeability (i.e., dissolution of the drug in the epithelia surface fluid and interaction of this drug with the epithelia membrane). Furthermore, when these experiments are conducted in a liquid-covered culture, epithelial permeability and surface structure may differ from an air interface culture, more representative of the physiological conditions.
For these reasons, there has been a change from liquid-covered cultures to air interface cell culture (7,11) methods, and the application of cascade impactors to study the deposition and transport of “real” particles across these epithelia (1,3,5,6). Several studies have modified current Pharmacopeia apparatuses, such as the twin-stage impinger (12), Andersen cascade impactor (1), multi-stage liquid impinger (3), and the next-generation impactor (6) to achieve these goals.
While integrated cell-based cascade impactor methodology is useful for determining the transport of deposited aerosol particles, all these methods are limited with respect to controlling the initial amount of drug deposited on the cells. One must be careful not to overload the cells (i.e., deposit multilayers of drug). Furthermore, controlling the initial deposited amount of drug require extensive preliminary formulation-specific studies and in some cases may require altering the formulation to reduce the amount deposited, making dose-ranging studies particularly difficult.
To overcome this limitation, a complementary approach is required that allows the delivery of very specific amounts of aerosol particles (i.e., 0.01–10 μg drug) to air interface cell cultures, without compromising the physicochemical properties of the formulation. One approach to achieve this would be to deposit the formulation as a suspension in a non-aqueous (hydrophobic and volatile) media that has a low surface tension and low boiling point. After addition, the media would rapidly evaporate leaving the drug particles to interact with the surface lining fluid and epithelial cells; transport studies would then be performed. 2H,3H-decafluoropentane (HPFP) is liquid at ambient pressure, with a boiling point of 53.6 °C and surface tension of 13.5 mNm−1. This liquid has been proposed as a model propellant substitute for current hydrofluoroalkane (HFA) propellants used in metered dose inhalers (13). Thus, it is proposed that HPFP may be used as suitable media for the deposition and study of drug transport across air interface epithelia models.
In a previous study by Adi et al. (14), a combination of spray-dried microparticles of doxycycline (Dox) and ciprofloxacin (Cip) for inhalation have shown potential in treatment of lung diseases which require antibiotic therapy, such as cystic fibrosis. The aim of this study was to deliver a suspension of aerosol microparticles (Dox and Cip) using HPFP as delivery vehicle to study the epithelial permeability of specific amounts of microparticles (between 1 and 3 μg of each antibiotic) across Calu-3 bronchial cells.
MATERIALS AND METHODS
Materials
Microparticles containing ciprofloxacin HCl (Cip) (MP; Biomedical Australasia Pty Limited, Sydney, Australia) and doxycycline (Dox) (MP; Biomedical Australasia Pty Limited, Sydney, Australia) alone or in a 50:50% w/w ratio, were spray dried using a Büchi B-290 spray dryer (Büchi Mini Spray Dryer B-191, Flawil, Switzerland) using Milli-Q water as solvent, equipped with a twin-fluid, coaxial atomizer under the following conditions: inlet temperature 110 °C, measured outlet temperature 58 °C, solution feed rate 4 mL min−1, aspirator rate 100%, and atomizing airflow 700 L h−1 (15). Dry powder yields were between 60 and 70%.
Particle Size Measurements
Particle size measurements of the microparticles were conducted using a Malvern Mastersizer 3000 with Scirocco dry dispersion unit (Malvern Instruments Ltd., Malvern, UK). A feed pressure of 4 bar and feed rate of 50% was used, and samples were measured when obscuration values fell between 0.5 and 5%. All samples were analyzed in triplicate over 10-s intervals.
Solvent Purification
2H, 3H-perfluoropentane (HPFP; Apollo Scientific, Cheshire, UK) was purified with chromatographic grade acidic and basic aluminium oxide (Fluka, Gillingham, UK) to remove impurities according to the method described by Rogueda (13).
Cell Biology Assays
Calu-3 cells (ATCC, Rockville, USA) were cultured and propagated according to ATCC recommendations as described previously (7). Cells were seeded onto polyester Transwell inserts (0.33 cm2, 0.4 μm pore size) (Corning Costar, MA, USA) at a density of 5 × 105 cells ml−1 to study the uptake of the Cip and Dox antibiotics. The cell monolayers were allowed to differentiate and polarize for 12–14 days under air interface conditions as previously determined (7).
The viability of Calu-3 cells following evaporation of HPFP was demonstrated by harvesting the cells and confirming the number of viable cells using the trypan blue exclusion method, as described in literature (16).
To ensure the integrity of the cell layer following treatment, 50 μl of HPFP was added to Transwells seeded with Calu-3 cells. Following evaporation of HPFP, the barrier integrity was studied by measuring the transepithelial electrical resistance (TEER) of the monolayers using a Voltohmmeter (EVOM with STX-2 chopstick electrodes, World Precision Instruments, FL, USA). Transport of the paracellular marker fluorescein-Na (Flu-Na) (MW = 376 g/mol and log P = − 1.52) was also assessed to complement TEER results (7).
To determine the effect of HPFP on the mucus glycoproteins following evaporation of HPFP, the mucus layer was stained using alcian blue according to a previously published method (7).
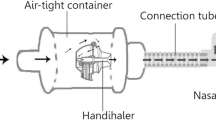
Uptake of Cip and Dox, as single and combination microparticles, was studied following suspension of 200 and 400 μg of single and combination formulation in 1 ml of HPFP, respectively. The suspensions were then vortexed and sonicated for 30 s, and 10 μl of each suspension (Dox, Cip, and Dox-Cip) was added to Calu-3 cells grown on Transwells in a 24-well plate. The plate remained without a lid for 5–10 min in the laminar flow hood until HPFP evaporated from the surface of the cells. This resulted in approximately 2 μg of single-drug formulations and 4 μg of combo formulation on the cell surface. The Transwells were then transferred to a 24-well plate containing 350 μl of Hank’s balanced salt solution (HBSS) (Gibco, Invitrogen, Sydney, Australia) in the basal chamber. At set time points (30, 60, 90, 120, 150, 180, 210, and 240 min), samples of the buffer were taken to measure the drug transport. At the end of the experiment, the cell surfaces were rinsed with buffer and samples collected for analysis. Furthermore, the amount of Cip and Dox present inside the cells was analyzed as described previously (14). The amount of the transported drug, the amount of drug left on the cell surface, and the drug retained within the cells were then analyzed by high-performance liquid chromatography (HPLC) according to the method described by Adi et al. (14).
Statistical Analysis
Data were analyzed using SPSS.17 software. One-way ANOVA with Tukey’s post hoc test (alpha level of p < 0.05) was used to test for significance. Data was represented as the mean ± standard deviation of at least three independent experiments.
RESULTS AND DISCUSSION
Particle size distributions for the spray-dried microparticles are shown in Fig. 1. Analysis of the data shows that powders have similar volumetric particle size distributions, suitable for inhalation drug delivery. Specifically, Cip had D10 = 1.07 ± 0.04 μm, D50 = 1.90 ± 0.07 μm, and D90 = 3.36 ± 0.11 μm; Dox had D10 = 0.64 ± 0.84 μm, D50 = 2.19 ± 1.61 μm, and D90 = 2.56 ± 0.45 μm; and the Dox-Cip combination had D10 = 0.87 ± 0.02 μm, D50 = 1.66 ± 0.05 μm, and D90 = 3.03 ± 0.15 μm, n = 3.
Cell viability results using trypan blue exclusion method showed that 91.3 ± 2.7% cells following evaporation of the HPFP were still viable. This value was achieved relative to the number of viable cells in the control Transwell inserts not exposed to HPFP. This finding shows the non-toxic nature of HPFP to Calu-3 cells in culture.
Comparison of the TEER values before addition and after the evaporation of HPFP showed no significant difference in the measurements. The TEER value was 451 ± 28 Ω.cm2 before and 437 ± 17 Ω.cm2 after HPFP evaporation. These results were further confirmed by Flu-Na permeability; the paracellular permeability was 2.52 ± 0.45 × 10−7 cm s−1 before HPFP addition and 3.01 ± 0.58 × 10−7 cm s−1 after HPFP evaporation. There was no statistically significant difference observed in TEER and permeability values after HPFP evaporation. Furthermore, results were similar to the barrier integrity values obtained in previous study by Haghi et al. that indicated a TEER value of 474 ± 44 Ω cm2 and permeability value of 2.33 ± 0.36 × 10−7 cm s−1, where barrier integrity for Calu-3 epithelial cells was established (7).
Mucus staining with alcian blue and the corresponding analysis of the intensity of the blue color using ImageJ software (NIH, USA) showed no statistically significant difference in the blue intensity measured, indicating that exposure of the Calu-3 cells to HPFP did not alter the amount of mucus present at the epithelia. Figure 2 depicts the mucus staining for the control vs. staining of the cells following evaporation of HPFP. According to cell viability, barrier integrity, and mucus staining results, exposure to HPFP did not alter any of the characteristics deemed essential for drug transport study investigated in a previous study (7).
Analysis of Dox and Cip following the collection of drug samples revealed that the total amount of Cip and Dox on Calu-3 cells were as follows: 2.09 ± 0.32 μg and 2.15 ± 0.54 μg Cip from the single and combination formulation, respectively, and 2.15 ± 0.43 μg and 2.33 ± 0.35 μg Dox from the single and combination formulation, respectively. There was no statistically significant difference observed between the amount of Cip and Dox on Calu-3 cells. The percentage of drug transport illustrates the amount of drug transported relative to the drug recovered after adding together the transported amount, the amount still on the cell surface (apical), and the amount retained within the cells (Fig. 3).
When comparing single Dox permeability from single vs. combination formulations, a significant difference is observed in the amount and percentage of Dox transported and retained in the epithelial cells (Fig. 3a). Interestingly, this phenomenon is not observed with Cip formulations and the amount and percentage of Cip transported from the single formulation was not significantly different from the amount and percentage of Cip transported from the combination formulation (Table I).
Comparison of the single Dox and Cip formulation revealed that the amount of Cip transported (Fig. 3b) was significantly more than Dox, but no significant difference was observed in the amount of either Cip or Dox retained in the cells. Interestingly, in the combination formulation, no Dox was detected in the basal chamber while the amount of Cip transported was not significantly different from transport of the single Cip formulation. Furthermore, analysis of the amount of Dox in the cells from the combination formulation revealed a significant increase in comparison with Dox from the single formulation. Interestingly, this phenomenon was not observed for Cip and the amount of Cip retained in the cells from single and combination formulations was not significantly different.
These findings can be attributed to the fact that, following particles deposition on the epithelial cells, these particles have to dissolve before being able to cross the epithelial barrier. Since water solubility of Cip at pH 7.4 is considerably higher than Dox (135 mg ml−1 for Cip vs. 2.15 mg ml−1 for Dox), Cip can dissolve in the limited amount of airway surface liquid faster than Dox and consequently has a faster transport across the epithelial barrier. However, in more complex systems, in the presence of a carrier or a second drug, in this case (Dox-Cip), dissolution of Dox could become a rate-limiting step in transport, resulting in a significantly lower transport rate for Dox from combination formulation. This agrees with a previous study where the presence of glycerol in aerosol particles containing beclomethasone dipropionate (BDP) was shown to potentially impact the disposition of BDP in the lungs (17).
In physiological conditions, the number of deposited particles per unit airway surface area is at submicron levels; therefore, in order to gain clear understanding of the interaction between epithelial cells and transport characteristics of these microparticles, development of methods that would allow the deposition of specific quantity of drug on the epithelial cells is essential.
In comparison with other methods of depositing microparticles, this proposed method, using drug suspended in HPFP, provides control over the amount of drugs applied on the surface of the cells. Therefore, cell permeability studies could be conducted with considerably smaller and more reproducible doses, without the physicochemical characteristics of the drugs being compromised, or the use of modified pharmacopeia impactors.
CONCLUSION
In conclusion, one important step in the assessment of an aerosol formulation is the establishment of the permeability profile of drug/s across the epithelial barrier. Specifically, when investigating more complex formulations where excipients or multiple drugs are present in the formulation, or when there is very little material to work with, these factors might impact on the permeability of the drug. In these cases, using methods that allow deposition of small amount (< 10 μg) of drugs without compromising the physicochemical properties of the particles becomes essential.
The suspension of microparticles in HPFP as presented in this study has provided a novel, non-toxic and reproducible method to deliver and study the permeability of specific quantity of drugs across respiratory epithelial cells.
References
Haghi M, Traini D, Young P. In vitro cell integrated impactor deposition methodology for the study of aerodynamically relevant size fractions from commercial pressurised metered dose inhalers. Pharm Res. 2014;31(7):1779–87. https://doi.org/10.1007/s11095-013-1282-2.
Fiegel J, Ehrhardt C, Schaefer UF, Lehr CM, Hanes J. Large porous particle impingement on lung epithelial cell monolayers—toward improved particle characterization in the lung. Pharmaceut Res. 2003;20(5):788–96. https://doi.org/10.1023/A:1023441804464.
Bur M, Rothen-Rutishauser B, Huwer H, Lehr CM. A novel cell compatible impingement system to study in vitro drug absorption from dry powder aerosol formulations. Eur J Pharm Biopharm. 2009;72(2):350–7. https://doi.org/10.1016/j.ejpb.2008.07.019.
Hein S, Bur M, Schaefer UF, Lehr CM. A new pharmaceutical aerosol deposition device on cell cultures (PADDOCC) to evaluate pulmonary drug absorption for metered dose dry powder formulations. Eur J Pharm Biopharm. 2011;77(1):132–8. https://doi.org/10.1016/j.ejpb.2010.10.003.
Cooney D, Kazantseva M, Hickey AJ. Development of a size-dependent aerosol deposition model utilising human airway epithelial cells for evaluating aerosol drug delivery. Atla-Altern Lab Anim. 2004;32(6):581–90.
McDonnell C, Shur J, Burns J, Hipkiss D, Price R. Investigation deposition and drug absorption of budesonide microparticles using a cell compatible next generation impactor. In: Publishing DHIl, editor. Respir Drug Deliv USA 2012. p. 785–788.
Haghi M, Young PM, Traini D, Jaiswal R, Gong J, Bebawy M. Time- and passage-dependent characteristics of a Calu-3 respiratory epithelial cell model. Drug Dev Ind Pharm. 2010;36(10):1207–14. https://doi.org/10.3109/03639041003695113.
Grainger CI, Greenwell LL, Lockley DJ, Martin GP, Forbes B. Culture of Calu-3 cells at the air interface provides a representative model of the airway epithelial barrier. Pharm Res. 2006;23(7):1482–90. https://doi.org/10.1007/s11095-006-0255-0.
Mathias NR, Timoszyk J, Stetsko PI, Megill JR, Smith RL, Wall DA. Permeability characteristics of Calu-3 human bronchial epithelial cells: in vitro-in vivo correlation to predict lung absorption in rats. J Drug Target. 2002;10(1):31–40. https://doi.org/10.1080/10611860290007504.
Exiarch H, Haltner-Ukomadu E, Beisswenger C, Bock U. Drug delivery to the lung: permeability and physicochemical characteristics of drugs as the basis for a pulmonary biopharmaceutical classification system (pBCS). J Epithelial Biol Pharmacol. 2010;3:1–14.
Pezzulo AA, Starner TD, Scheetz TE, Traver GL, Tilley AE, Harvey BG, et al. The air-liquid interface and use of primary cell cultures are important to recapitulate the transcriptional profile of in vivo airway epithelia. Am J Physiol Lung Cell Mol Physiol. 2011;300(1):L25–31. https://doi.org/10.1152/ajplung.00256.2010.
Grainger CI, Greenwell LL, Martin GP, Forbes B. The permeability of large molecular weight solutes following particle delivery to air-interfaced cells that model the respiratory mucosa. Eur J Pharm Biopharm. 2009;71(2):318–24. https://doi.org/10.1016/j.ejpb.2008.09.006.
Rogueda PGA. HPFP, a model propellant for pMDIs. Drug Dev Ind Pharm. 2003;29(1):39–49. https://doi.org/10.1081/Ddc-120016682.
Adi H, Young PM, Chan HK, Salama R, Traini D. Controlled release antibiotics for dry powder lung delivery. Drug Dev Ind Pharm. 2010;36(1):119–26. https://doi.org/10.3109/03639040903099769.
Adi H, Young P, Chan HK, Stewart P, Agus H, Traini D. Cospray dried antibiotics for dry powder lung delivery. J Pharm Sci. 2007;97(8):3356–66.
Tolnai SA. Method for viable cell count. Methods Cell Sci. 1975;1:37–8.
Haghi M, Bebawy M, Colombo P, Forbes B, Lewis DA, Salama R, et al. Towards the bioequivalence of pressurised metered dose inhalers 2. Aerodynamically equivalent particles (with and without glycerol) exhibit different biopharmaceutical profiles in vitro. Eur J Pharm Biopharm. 2014;86(1):38–45. https://doi.org/10.1016/j.ejpb.2013.02.020.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haghi, M., Young, P.M. & Traini, D. A Simple and Rapid Method for Deposition and Measurement of Drug Transport Across Air Interface Respiratory Epithelia. AAPS PharmSciTech 19, 3272–3276 (2018). https://doi.org/10.1208/s12249-018-1170-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-018-1170-5