Abstract
Purpose
The purpose of this study was to present a modified Andersen cascade impactor (ACI) as a platform to evaluate the deposition and subsequent transport of aerosol micropaticles across airway epithelial cells.
Methods
The impaction plate of an ACI was modified to accommodate up to eight Snapwells. Aerodynamic particle size distribution of the modified ACI was investigated with two commercially available formulations of Ventolin® (salbutamol sulphate) and QVAR® (beclomethasone dipropionate). Deposition and transport of these drug microparticles across sub-bronchial epithelial Calu-3 cells were also studied.
Results
The modified ACI demonstrated reproducible deposition patterns of the commercially available pressurised metered dose inhalers compared to the standard ACI. Furthermore, the Calu-3 cells could be placed in different stages of the modified ACI. No significant effect was observed among the transport rate of different particle sizes deposited on Calu-3 cells within the range of 3.3 to 0.4 μm.
Conclusions
The use of the cell compatible ACI to assess the fate of microparticles after deposition on the respiratory epithelia may allow for better understanding of deposited microparticles in vivo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Administering a clinically relevant dose of therapeutic agent reproducibly to a specific target site within the airways is technically challenging. Over the last decade considerable effort has been invested in generating and administering aerosols to the lung with increased efficiency. This has resulted in the development of inhaled systems that can deliver over 50% of their nominal dose to the distal regions of the lungs (1). However, improving drug deposition efficiency within the lung may not always translate into improved therapeutic effects. The lung is a complex organ and disposition of the deposited particles will be governed by a multitude of factors, including the physicochemical properties of the drug delivery system (2) and the structure of the epithelia (3,4).
Considering the complexity of the lung, optimising drug delivery using in vitro methods is very challenging. Historically, pharmacopeia approved methods such as the next generation impactor (NGI), multi stage liquid impinger (MSLI) and Andersen cascade impactor (ACI) have been used to predict aerodynamic particle size distributions and thus deposition profiles (5). For example, Swift et al., has shown the relationship between particle size distribution in an impactor and particle deposition in human airways (6).
While these impactors are powerful tools for evaluating the aerodynamic performance of aerosol formulations, they do not give information relating to drug dissolution and transport at the epithelia. To overcome this limitation many authors have attempted to modify conventional impactors for the study of particle dissolution and transport (7,8). These techniques generally utilise artificial membranes and/or dissolution media compared to the more complex lung epithelia; resulting in a collection of data that are physically important, but not physiologically relevant: dissolution based techniques do not incorporate the complex structure of the epithelia surface fluid or the presence of transports within the membrane.
To overcome this limitation, researchers have developed a series of in vitro cell based methods that can be incorporated into classical impactors to provide a better understanding of the fate of microparticles after deposition in the respiratory tract (9,10). Considering the distribution of cells in the airways, ciliated epithelial cells are the most appropriate type for modelling the airway epithelium (11) in the conducting airways. Furthermore, among human airway epithelial cell lines, Calu-3 cells cultured at air-interface configuration have been extensively used as a platform to study microparticle absorption and transport within the lung in vitro (2,12–19).
Recent studies have investigated methods for depositing real aerosol formulations directly onto epithelial cells. For example, the twin stage impinger (TSI) has been used in several studies to deposit dry powder formulations, including varying molecular masses of fluorescein isothiocyanate- conjugated dextran (FITC-dex), salbutamol sulphate, di-sodium chromoglycate, salmeterol xinofoate and fluticasone propionate (12,14–16). The TSI method is relatively simple as it is based on a pharmacopeia twin stage impinger (Apparatus A in the European Pharmacopeia), used for routine quality control. The TSI has an aerodynamic cut-off for Stage 1 of ≤6.4 μm at 60 L.min−1. In this modified apparatus, the collection liquid in stage 2 is removed and a Transwell® containing epithelial cells can be inserted at the base of the impinging jet (12). Upon aerosolisation particles ≤6.4 μm are collected on the cell surface. While this technique is a useful screening tool, Stage 2 in-itself is not an impaction stage and thus the size distribution collected on the Transwell is not known. Furthermore, very little drug is actually deposited on the Transwell when studying pressurised metered dose inhaler (pMDI) systems with the majority either deposited in the flask or collected in the pump filter; therefore, multiple doses are required to achieve measurable quantity of drugs on the epithelial cells (2).
The multi-stage liquid impinger (MSLI) has been previously modified to study the deposition of large porous particles, salbutamol sulphate and budesonide microparticles on Calu-3 cells grown on Transwell inserts (17,18). However, like the TSI, the modified MSLI by Fiegel et al. (17) as well as the later are also limited to one insert per deposition, making collection of data time consuming. The ‘pharmaceutical aerosol deposition device on cell cultures’ (PADDOCC) apparatus (19) can accommodate up to three Snapwells however, particles in the PADDOCC setup are deposited via sedimentation which is in principle different to the other pharmacopeia impactors.
To overcome such issues, Price et al., incorporated an alternative Transwell design into a NGI and studied the deposition and transport of a budesonide pMDI formulation on Calu-3 cells (20). While, this preliminary study showed the potential for incorporation of epithelia cell lines into more advanced pharmacopeia impactors, the effect on aerodynamic cut-off diameter and the validation of the epithelia culture conditions was not fully investigated; including comparison of stage deposition profiles with and without the modified stage in place to confirm no variation in cut-off diameters were observed. However, Price et al., utilised Snapwell® culture wells rather than conventional Transwells, significantly reducing the jet to plate height and allowing the wells incorporation directly into the impaction plate.
While, the MSLI, TSI and recently the NGI, have been modified to study drug-cell interactions, little attention has been given to the ACI. The ACI is one of the core pharmacopeia impactors and has been routinely used for data collection for FDA product registration. To the authors knowledge, the only study incorporating epithelia cell lines into this device was reported by Cooney et al. who studied the deposition of nebulised FITC-dex on Calu-3 cells grown on Transwell inserts (21). However this study removed the impaction plate of stage 4 to incorporate the Transwells on stage 5, substantially increasing the jet to plate distances and flow through the impactor. Furthermore, the impact of the Transwell on the flow profile within the ACI was not considered.
In the current study a commercially available ACI was modified to incorporate epithelial cell lines, grown in large Snapwells (as reported by Price et al. (20)). Specifically, reusable ACI plates were engineered to be incorporated into any of the stages of the impactor allowing discrete particle size collection; at 28.3 L.min−1 these fractions are 9–5.8 μm, 5.8–4.7 μm, 4.7–3.3 μm, 3.3–2.1 μm, 2.1–1.1 μm, 1.1–0.7 μm and 0.7–0.4 μm for stages 0, 1, 2, 3, 4, 5, 6 and 7, respectively. The modified plates can accommodate up to eight Snapwells, containing Calu-3 cell monolayers, that are flush with the impaction plate, at a fixed radius around the circumference. This integration into the impaction plate results in minimal changes in nozzle jet-to-plate distance, meaning that the cut-off efficiency for any particular stage will not be greatly affected. Importantly, the ACI is symmetrical, meaning that collection efficiency will remain constant for Snapwells placed at a fixed radius under any given stage.
Specifically, in this study, the culture of Calu-3 cells in the larger Snapwells was compared to conventional Transwell culture conditions and their incorporation into the ACI and effect on drug deposition, evaluated as a function of ACI stage. Finally, the deposition and transport of two commercially available pMDI formulations (salbutamol sulphate (SS) Ventolin® and beclomethasone dipropionate (BDP) Qvar®) was studied as a function of size fraction.
Materials and Methods
Materials
Two commercially available pMDI formulations, Ventolin (GSK/Allen + Hanburys, Boronia, Australia) and Qvar (3M/iNova Pharmaceuticals, Sydney, Australia), were chosen as model formulations. These specific formulations were chosen as they contain very different drug molecules, different formulation approaches and deposition profiles. Ventolin is a suspension-based formulation containing salbutamol sulphate (SS) suspended in HFA propellant, while Qvar is a solution-based pMDI containing beclomethasone dipropionate (BDP), ethanol co-solvent and HFA. Both SS and BDP are drug molecules used in asthma therapy, however, they have different physicochemical characteristics; BDP is a Biopharmaceutical Classification System (BCS) class II model drug with poor solubility, while SS is a BSC class III with high solubility (22).
Water used throughout the experiments was purified by reverse osmosis (Milli-Q, Sydney, Australia). All solvents were analytical grade and were supplied by Sigma (Sydney, NSW, Australia). Sterile culture plastic ware was obtained from Sarstedt (Adelaide, Australia).
Cell Culture
The Calu-3 cell line (HTB-55) was obtained from the American Type Cell Culture Collection (ATCC, Rockville, USA) and was maintained according to the provider’s recommendations in complete Dulbecco’s Modified Eagle’s medium: F-12 containing 10% (v/v) fetal calf serum, 1% (v/v) nonessential amino acid solution and 1% (v/v) L-glutamine solution. Cells passages 40–42 were seeded on Snapwell polyester membrane (0.4 μm pore size, 1.12 cm2 Surface area) (Corning Costar, Lowell, MA, USA) at the density of 1.65 × 106 cells.ml−1 in 200 μl apical and 2 ml basal medium. The medium in the apical chamber was removed after 48 h to allow the establishment of air-interface configuration.
Transepithelial Electrical Resistance of Calu-3 Cells
To ensure the formation of the tight junction and suitability of the Calu-3 cells for transport studies, transepithelial electrical resistance (TEER) of the cells was measured over time using an EVOM Voltohmmeter (World Precision Instruments, FL, USA) with STX-2 chopstick electrodes according to the method described by Haghi et al. (23).
Permeability to Fluorescein Sodium
Barrier integrity of the Calu-3 monolayer was also confirmed by the permeability to paracellular marker, fluorescein sodium (flu-Na) (Sigma-Aldrich, Sydney, Australia) (MW 0.367 kDa). Flu-Na permeability was measured at days 5, 8, 11, 15, 17 and 19 after seeding. Briefly 100 μl of flu-Na solution (2.5 mg.ml−1) was added to the apical chamber. Samples of 100 μl were taken every 15 min over 4 h. The fluorescence of flu-Na in the samples was measured using a black, 96-wells plate using a spectrophotometer and associated software (Spectramax M2 and Soft Max pro 4.8, Molecular Devices, Sunnyvale, CA, USA) at excitation and emission wavelengths of 485 and 518 nm, respectively.
Histological Staining for Mucus Production
Alcian blue was used to stain mucus secretion according to the method described by Haghi et al. (23). At days 5, 8, 11, 15, 17 and 19 Calu-3 cells were fixed using 4% (w/v) paraformaldehyde (Sigma-Aldrich, Sydney, Australia). The cells were then stained using alcian blue stain (1% w/v alcian blue in 3% v/v acetic acid/water at pH 2.5) (Fronine Laboratory, Sydney, Australia). Afterwards, the inserts were air-dried and filter membrane cut and mounted on glass slides using Entellan new mounting medium (ProSciTech, Thuringowa, Australia) and sealed. The slides were imaged using an Olympus BX60 microscope (Olympus, Hamburg, Germany) with manual light exposure and ‘one push’ white balance on a background region. Images were then taken using an attached DP71 camera (Olympus). At least 15–20 images were taken per section. The images were post processed using Apple Automater (v 2.0.4 Apple Inc, California, USA) to centre crop 400 × 300 pixel JPEG images. Each image was analysed using Image J (v1.42q, NIH) with Colour Profile (Dimiter Prodanov; Leiden University Medical Center, Netherlands) and Colour Inspector 3D v2.0 (Kai Uwe Barthel; Internationale, Medieninformatik, Berlin, Germany) plugins. A three-dimensional colour space was produced representing the 8-bit red-green-blue (RGB) value of each image. The ratio of blue (RGBB ratio) was calculated by dividing the mean RGBB by the sum of the RGB values for each image (RGBr + RGBG + RGBB).
Development of the Modified ACI Plates
Custom-made ACI plates (Fig. 1) that can accommodate the Snapwells were designed using computer-aided design (CAD) (ANSYS DesignModeler release 13, ANSYS Inc., PA, USA). The CAD drawing was exported as a *.stl file, and a series of modified plates produced in acrylonitrile butadiene styrene (ABS) using a 3D printer (Dimension Elite, MN, USA) with associated software. The plates were designed to hold eight Snapwells, equally spaced at a 29 mm radius from the centre of the plate to the centre of each Snapwell.
Validation of the ACI Deposition Profiles with and Without the Modified Plates
Aerodynamic particle size distributions of SS and BDP from each formulation were assessed using the ACI following methodology outlined in the British Pharmacopeia (5). All studies were completed in triplicate with both conventional plates and modified plates, containing Snapwell inserts, replacing either stage 4 or 7 of the ACI (Fig. 1). The modified ACI was connected to a rotary vein pump (Westech Scientific Instruments, Bedfordshire, UK) and the flow rate adjusted to 28.3 L.min−1 using a calibrated flow meter (Model 4040, TSI Model Instruments, Germany).
The pMDIs were shaken, primed to waste and three doses were actuated into the ACI.
After aerosol deposition on wetted cell-free Snapwells, the ACI was disassembled and every stage was washed separately to quantify the total amount. The ACI plate containing the Snapwells was removed and washed to calculate the total amount of drug deposited on this specific stage and on each of the separate wells.
Deposition and Transport of Microparticles on Calu-3 Epithelial Cells by Incorporation into the Modified ACI Plates
Seventeen days post seeding, the Snapwells containing Calu-3 cells cultivated in an air-interface configuration were placed into modified ACI plates. Four cell-containing wells were used for each study, with the remaining wells containing blank inserts. For each formulation, four runs were conducted, where cells were placed in stage 4, 5, 6 and 7 of the ACI, respectively. This allowed the study of different particle size fractions on SS or BDP transport. For each investigation one shot was actuated into the ACI, which was then disassembled and the cell containing wells were removed for study. The inserts were transferred to a 6-well plate containing 600 μl of fresh pre-warmed modified buffer (Hank’s balanced salt solution (HBSS) (Gibco- Invitrogen, Sydney, Australia) supplemented with 4-(2-Hydroxyethyl) piperazine-1-ethanesulfonic acid sodium salt (HEPES) (1% v/v) (Sigma-Aldrich, Sydney, Australia), (±)-α-Tocopherol (vitamin E) (1% v/v) (Sigma-Aldrich, Sydney, Australia) and ethanol 97% (1% v/v) at pH 7.4). Samples of 200 μl were drawn from the basal chamber every hour for SS (and fresh modified buffer replaced the same amount) and after 4 h for BDP. At the end of the experiment, the surface of the Calu-3 cells was washed with buffer and collected for analysis of residual apical drug. This allowed for the calculation of total drug deposited via the cumulative sum of all samples. Metabolism of BDP to its major metabolite, beclomethasone 17-monopropionate (BMP) (approximated to 1:1 stoichiometry), was also accounted for, and used to calculate the total amount of BDP deposited and total drug transported (2).
In order to confirm the integrity of the cell monolayer after drug deposition, sham deposition (using pMDIs containing the HFA propellant and 7% ethanol only) was done with the cells incorporated into the stages of the ACI. Following deposition, the permeability to flu-Na was measured in the control vs. the sham depositions.
Chemical Quantification of Salbutamol and Beclomethasone Microparticles After Aerosols Deposition
Chemical quantification of SS and BDP and its metabolite BMP was conducted using high performance liquid chromatography (HPLC). A Shimadzu Prominence UFLC system equipped with an SPD-20A UV-Vis detector, LC-20AT solvent delivery unit, SIL-20A HT Autosampler (Shimadzu Corporation, Japan) and NovaPak C18 column (5 μm, 150 × 3.9 mm) (Waters Corporation, Milford Massachusetts, USA) were used to quantify SS, BDP and BMP in the samples. The mobile phase for SS was a mixture of methanol: 0.1% w/v aqueous sodium dodecyl sulphate solution (60:40%, v/v). The detector was operating at 276 nm. The flow rate was 1 ml.min−1 and injection volume 100 μl. Standard linearity was obtained between 0.01 and 25 μg.ml−1 (R2 = 0.9999). For BDP and BMP samples data were recorded at a UV Detector wavelength of 240 nm. The mobile phase consisted of a mixture of methanol and 0.05% w/v ammonium acetate aqueous solution (68:32%, v/v). The flow rate was set at 1 ml.min−1 with an injection volume of 100 μl. Linearity of BDP and BMP was obtained between 0.01 and 50 μg.ml−1 (R2 = 0.999).
Statistical Analysis
All results are expressed as mean ± standard deviation of at least three replicate experiments. Data were analysed by using SPSS® 17.0 statistical software package (SPSS Inc, Chicago, Illinois, USA). Analysis of variance (ANOVA) one-way (with Tukey’s post hoc analysis) was utilized to test for significance (which was quoted at the level of P < 0.05) between treatment groups.
Results
Optimisation of Culture Conditions Using Snapwell Inserts
The Snapwell inserts had a higher surface area (1.12 cm2) than conventional Transwell inserts (0.33 cm2) as used in previous studies (23). While the pore size, material and seeding density were consistent with previous studies, the formation of tight junctions and mucus across this larger membrane were studied to ensure comparative test conditions. In general, the Calu-3 cells grew to confluence within 8 days, when seeded on Snapwell inserts and developed tight epithelial monolayers over 15 days in culture. As an indicator of monolayer integrity, TEER was measured across the Calu-3 cells every 2–4 days from day 5 onwards. Monolayer resistance measurements indicated that Calu-3 cells generate a measurable TEER from day 5 onwards. No significant difference was observed in the TEER from day 15 onwards, with resistance values reaching a plateau of 557.36 ± 58.88 Ω.cm2 (Fig. 2a).
In addition to TEER measurements, apparent permeability was measured at equivalent time points using the paracellular marker, flu-Na (Fig. 2b). A significant decrease in permeability from day 5 onwards was observed. This is consistent with the TEER measurements described above. However, the apparent permeability (Papp) was not the same order of magnitude as in 0.33 cm2 Transwell studies (23) until day 17 and onwards (1.07 × 10−7 ± 5.42 × 10−8 cm. s−1).
Mucus secretion increased with respect to culture time and was measured by the RGBB ratio. Confluent mucus coverage was not observed until day 15 and no statistical difference in RGBB ratio was noticed post 17 days (ANOVA, p > 0.05). Representative images of mucus secretion at days 8, 11, 15, 17 and 19 post seeding and a plot of the RGBB ratio with respect to time are shown in Fig. 3.
The formation of tight junctions and mucus producing epithelia was comparable to previous studies using 0.33 cm2 Transwells (23); however, analysis of the data suggested 17 days culture was needed, in comparison to 11 days, for optimisation of the epithelia to equivalent values of those published using the smaller Transwell design. While TEER values were ≥ 450 Ωcm2 at day 11, the papp did nor reach the 1 × 10−7 order range until day 17, as reported in previous studies (23–25). Subsequently, for transport studies, epithelial cells cultured under air-interface conditions were used after 17 days.
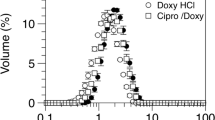
Aerodynamic Particle Distribution of the Formulations with Standard and Modified ACI Plates
Particle size distributions of Ventolin and QVAR pMDI marketed formulations, using the standard and modified ACI plates, are displayed in Fig. 4a and b, respectively. In addition, log-probability plots of the cumulative particle mass undersize for SS and BDP, collected on each stage of the ACI were reported and used to calculate the mass median aerodynamic diameter (MMAD) and geometric standard deviation (GSD). The MMAD and GSD for SS and BDP, with and without the modified ACI plates, on stage 4 or 7 are shown in Table I. In general, the MMAD and GSD values for QVAR were similar to those reported previously (26–28). While, limited literature on the HFA salbutamol formulation is available, the MMAD was in good agreement with the 2.7 ± 0.1 μm value reported by Kotian et al. (29).
Analysis of both the deposition profile and aerodynamic parameters indicated there was no significant difference observed between the aerodynamic particle size distributions of either formulation when the modified plates containing Snapwells were present. Such observations suggest that the modified Snapwell design can be used for routine aerodynamic size fractioning and cell deposition studies.
Drug Transport of SS and BDP from Ventolin and Qvar, Across Calu-3 Epithelial Cells as a Function of Size Fraction
The integrity of the Calu-3 cell monolayer after sham deposition (using pMDIs containing the HFA propellant and 7% ethanol only) showed that there was no significant difference between the permeability values (P > 0.05) of the control and sham deposited cells, indicating the deposition method and the air stream do not damage the monolayer integrity (Data not shown).
The deposition and transport of SS and BDP across Calu-3 air interface cultured cell lines as a function of ACI impactor stage are shown in Tables II and III, respectively. In general, the amount of drug deposited onto each Snapwell was in good agreement with the amount deposited on the whole stage, when conducting the aerodynamic size distribution measurements. This approximated to 1/42 of the amount of total stage deposition, corresponding to the relative surface area of the Snapwell to total plate area.
For SS, results indicated that regardless of the ACI stage number (S4–7) there was no statistical difference in percentage mass transported over 4 h, with >85% being transported. Such observations suggest that neither deposited mass nor size fraction (between 0.4 and 3.3 μm) influenced percentage drug uptake. No significant difference in the percentage transport of BDP (including metabolite) was observed as a function of deposited mass or size fraction between 0.4 and 3.3 μm (stage 4–7 respectively). However, the transport of BDP was significantly slower than SS with ~50% being transported at 4 h.
Discussion
The modified ACI presented in this study allows for the deposition of microparticles generated from pMDI formulations onto multiple Snapwells simultaneously (up to 8). No variation in the aerodynamic particle size distribution was observed when the modified plates were substituted with standard plates (4,7). In this study, two formulations were evaluated; a suspension based formulation containing micronised SS (Ventolin) and a solution-based formulation containing BDP and ethanol (Qvar). While previous studies have investigated the transport of SS and BDP across Calu-3 monolayers, it is difficult to make direct comparison as the formulations and methodologies vary between studies. For example Bur et al., (18,30) studied the transport of SS from commercial dry powder SS formulations and reported significantly slower transport rates (<10% over 4 h). However, in these studies, the time in culture, culture conditions and epithelial barrier properties differed. Furthermore, the particle size of the deposited powders would have been significantly higher using the modified MSLI (stage 3 at 30 L.min−1 has a cut-off diameter around 10 μm) and many of the formulations tested contained large lactose carriers. In a previous study by Haghi et al., (14) using a modified TSI, higher transport rates were observed (≥ 60% over 4 h), however, again the study focused on dry powder formulations and the particle cut-off was higher (≤6.4 μm) than those studied here (≤ 3.3 μm).
Solution based pMDIs containing BDP have been investigated previously. Both Grainger et al., (13) and Haghi et al., (2) utilized the modified TSI to study the deposition and transport of BDP from ethanol containing pMDI formulations. Grainger reported the transport of BDP from Qvar using the modified TSI as 35–55% transport over approximately 70 mins. In our study transport was approximately 50% after 4 h, for similar deposited amounts of drug. While the permeability of flu-Na across the cell line was not reported in the Grainger study, the TEER values of the epithelia were reported as lower than that studied here (320 ± 32 Ω.cm2 in comparison to 557.36 ± 58.88 Ω.cm2). This difference in epithelia tight junctions may relate to the higher transfer rate. In comparison, the previous study by Haghi et al. (2) reported similar barrier function and ~20% BDP transport over a 4 h period (lower than reported here). However, the solution based BDP formulation was designed to generate a courser aerosol cloud, with 50% of the particles having an aerodynamic diameter greater than 2.4 μm (31). Again, using the TSI with a cut-off of 6.4 μm, it is likely that the particles deposited were larger than those studied here.
While this study showed that particle size between 3.3 and 0.4 μm did not appreciably affect transport rate of either SS or BDP, coarser aerosol particles may be affected and warrant further study. An increase in particle diameter from 3.3 μm to 6.4 μm will increase the volume and decrease the surface area by approximately one order of magnitude. While this is an interesting concept it is difficult to study using these formulations since there is limited particles from either Qvar or Ventolin within this higher size range. Future studies should investigate non-commercial formulations where the mass and size can be specifically tuned to a specific size range of ACI plates.
Ultimately, this study presents a cell integrated modified ACI deposition methodology that can capture discrete aerodynamic size fractions without altering the impaction profile of the ACI. This approach can be used to study a range of commercial and non-commercial aerosol formulations using cell lines relating to different regions of the airways.
Conclusion
The current study has demonstrated the potential of the cell integrated modified ACI as a novel methodology to investigate the deposition, dissolution and transport of specific narrow size aerosol particle distribution directly to the surface of cultured Calu-3 airways epithelial cells, using two marketed pMDI formulation. This novel in vitro drug deposition apparatus provides an improved deposition model to investigate the fate of aerosol particles at different regions of the airways. Although direct comparison between human studies and in vitro cell work is challenging, commercial software platforms are now available that extrapolate in vivo data from in vitro results (i.e. SIMCYP Ltd-. http://www.simcyp.com). Future studies involve an extension of the current setup towards complex co-culture system of primary epithelial, dendritic cells and macrophages. Furthermore, the use of the same apparatus with non-commercial pMDI formulations and dry powder inhalers are ongoing.
References
Edwards DA, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew ML, et al. Large porous particles for pulmonary drug delivery. Science. 1997;276(5320):1868–72.
Haghi M, Bebawy M, Colombo P, Forbes B, Lewis DA, Salama R, et al. Towards the bioequivalence of pressurised metered dose inhalers 2. Aerodynamically equivalent particles (with and without glycerol) exhibit different biopharmaceutical profiles in vitro. Eur J Pharm Biopharm. 2013. doi:10.1016/j.ejpb.2013.02.020.
Patton JS, Byron PR. Inhaling medicines: delivering drugs to the body through the lungs. Nat Rev Drug Discov. 2007;6(1):67–74.
Bur M, Lehr C-M. Pulmonary cell culture models to study the safety and efficacy of innovative aerosol medicines. Expert Opin Drug Deliv. 2008;5(6):641–52.
Online databese Stationery Office. British Pharmacopoeia, Appendix XII C London. 2012. Accessed 01 June 2013. Available from: http://www.pharmacopoeia.co.uk.
Swift DL. Use of mathematical aerosol deposition models in predicting the distribution of inhaled therapeutic aerosols. In: Hickey AJ, editor. Inhalation aerosols. New York: Marcel Dekker; 1996. p. 51–7.
Davies NM, Feddah MR. A novel method for assessing dissolution of aerosol inhaler products. Int J Pharm. 2003;255(1–2):175–87.
Arora D, Shah K, Halquist M, Sakagami M. In Vitro Aqueous Fluid-Capacity-Limited Dissolution Testing of Respirable Aerosol Drug Particles Generated from Inhaler Products. Pharm Res. 2010;27(5):786–95.
Dunbar C, Mitchell J. Analysis of cascade impactor mass distributions. J Aerosol Med. 2005;18(4):439–51.
Agu RU, Ugwoke MI. In vitro and in vivo testing methods for respiratory drug delivery. Expert Opin Drug Deliv. 2011;8(1):57–69.
Forbes B, Ehrhardt C, Forbes B, Ehrhardt C. Human respiratory epithelial cell culture for drug delivery applications. Eur J Pharm Biopharm. 2005;60(2):193–205.
Grainger CI, Greenwell LL, Martin GP, Forbes B. The permeability of large molecular weight solutes following particle delivery to air-interfaced cells that model the respiratory mucosa. Eur J Pharm Biopharm. 2009;71(2):318–24.
Grainger CI, Saunders M, Buttini F, Telford R, Merolla LL, Martin GP, et al. Critical characteristics for corticosteroid solution metered dose inhaler bioequivalence. Mol Pharm. 2012;9(3):563–9.
Haghi M, Traini D, Bebawy M, Young PM. Deposition, Diffusion and transport mechanism of dry powder microparticulate salbutamol, at the respiratory epithelia. Mol Pharm. 2012;9(6):1717–26.
Haghi M, Salama R, Traini D, Bebawy M, Young P. Modification of disodium cromoglycate passage across lung epithelium in vitro via incorporation into polymeric microparticles. AAPSJ. 2012;14(1):79–86.
Haghi M, Traini D, Postma DS, Bebawy M, Young PM. Mediated fluticasone uptake across Calu-3 cells by salmeterol as combination powder inhaler. Respirology. 2013. doi:10.1111/resp.12146.
Fiegel J, Ehrhardt C, Schaefer UF, Lehr CM, Hanes J. Large porous particle impingement on lung epithelial cell monolayers–toward improved particle characterization in the lung. Pharm Res. 2003;20(5):788–96.
Bur M, Rothen-Rutishauser B, Huwer H, Lehr C-M. A novel cell compatible impingement system to study in vitro drug absorption from dry powder aerosol formulations. Eur J Pharm Biopharm. 2009;72(2):350–7.
Hein S, Bur M, Schaefer UF, Lehr C-M. A new pharmaceutical aerosol deposition device on cell cultures (PADDOCC) to evaluate pulmonary drug absorption for metered dose dry powder formulations. Eur J Pharm Biopharm. 2011;77(1):132–8.
McDonnell C, Shur J, Burns J, Hipkiss D, Price R. Investigation deposition and drug absorption of budesonide microparticles using a cell compatible next generation impactor. Respir Drug Deliv Proc. 2012; Vol 3, pp 785-788. Davis Healthcare Int’l Publishing. Illinois, USA.
Cooney D, Kazantseva M, Hickey AJ. Development of size-dependent aerosol deposition model utilizing human airway epithelial cells for evaluating aerosol Drug Delivery. ALTA. 2004;32(6):581–90.
Exiarch H, Haltner-Ukomadu E, Beisswenger C, Bock U. Drug delivery to the lung: Permeability and physicochemical characteristics of drugs as the basis for a pulmonary biopharmaceutical classification system (pBCS). J Epithelial Biol Pharmacol. 2010;3:1–14.
Haghi M, Young PM, Traini D, Jaiswal R, Gong J, Bebawy M. Time- and passage-dependent characteristics of a Calu-3 respiratory epithelial cell model. Drug Dev Ind Pharm. 2010;36(10):1207–14.
Grainger C, Greenwell L, Lockley D, Martin G, Forbes B. Culture of Calu-3 cells at the air interface provides a representative model of the airway epithelial barrier. Pharm Res. 2006;23(7):1482–90.
Mathias NR, Timoszyk J, Stetsko PI, Megill JR, Smith RL, Wall DA, et al. Permeability characteristics of calu-3 human bronchial epithelial cells: in vitro-in vivo correlation to predict lung absorption in rats. J Drug Target. 2002;10(1):31–40.
Mitchell J, Nagel M, Wiersema K, Doyle C. Aerodynamic particle size analysis of aerosols from pressurized metered-dose inhalers: Comparison of andersen 8-stage cascade impactor, next generation pharmaceutical impactor, and model 3321 aerodynamic particle sizer aerosol spectrometer. AAPS PharmSciTech. 2003;4(4):425–33.
Nagel MW, Wiersema KJ, Bates SL, Mitchell JP. Size analysis of a pressurized metered dose inhaler-delivered solution formulation by an Aerosizer-LD time-of-flight aerosol particle size spectrometer. J Aerosol Med Pulm Drug Deliv. 2002;15(1):75–85.
Hoe S, Young P, Chan H-K, Traini D. Introduction of the Electrical Next Generation Impactor (eNGI) and Investigation of its Capabilities for the Study of Pressurized Metered Dose Inhalers. Pharm Res. 2009;26(2):431–7.
Kotian R, Peart L, Bryner J, Byron PR. Calibration of the modified electrical low-pressure impactor (ELPI) for use with pressurized pharmaceutical aerosols. J Aerosol Med Pulm Drug Deliv. 2009;22(1):55–66.
Bur M, Huwer H, Muys L, Lehr C-M. Drug transport across pulmonary epithelial cell monolayers: Effects of particle size, apical liquid volume, and deposition technique. J Aerosol Med Pulm Drug Deliv. 2010;23(3):119–27.
Lewis DA, Young PM, Buttini F, Church T, Colombo P, Forbes B, et al. Towards the bioequivalence of pressurised metered dose inhalers 1: Design and characterisation of aerodynamically equivalent beclomethasone dipropionate inhalers with and without glycerol as a non-volatile excipient. Eur J Pharm Biopharm. 2013. doi:10.1016/j.ejpb.2013.02.014.
Acknowledgments and Disclosures
A/Professor Traini is the recipient of an Australian Research Council Future Fellowship (project number FT12010063). A/Professor Young is the recipient of an Australian Research Council Future Fellowship (project number FT110100996).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haghi, M., Traini, D. & Young, P. In Vitro Cell Integrated Impactor Deposition Methodology for the Study of Aerodynamically Relevant Size Fractions from Commercial Pressurised Metered Dose Inhalers. Pharm Res 31, 1779–1787 (2014). https://doi.org/10.1007/s11095-013-1282-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-013-1282-2